Abstract
This study was performed to evaluate the relation of high-sensitivity C-reactive protein (hsCRP) with several cardiovascular risk factors such as age, blood pressure, smoking habit and serum lipids, body mass index, blood glucose, regular exercise, alcohol drinking, white blood cell counts in a cross-sectional survey. Plasma hsCRP was measured by immunoturbidimetry in 202 subjects, aged over 50 yr, who participated in health-check survey in a rural area of Jeollanamdo, Korea. Plasma hsCRP level was 1.9±3.0 mg/dL. There were significant associations between hsCRP levels and age, white blood cell counts, blood glucose, diastolic blood pressure, HDL-cholesterol, body mass index and smoking status. In stepwise multivariate regression analysis, white blood cell counts, age, blood glucose, smoking status and body mass index were independent correlates of hsCRP levels. In conclusion, plasma hsCRP levels were associated with several cardiovascular risk factors, and these data are compatible with the hypothesis that CRP levels may be a marker for preclinical cardiovascular disease. Further what we need now are prospective studies to evaluate the association of C-reactive protein concentrations with subsequent cardiac events.
There is increasing evidence that higher levels of high-sensitivity C-reactive protein (hsCRP) is a predictor of cardiovascular disease (CVD), and may play an important role in the different stages of the development of atherosclerosis (1, 2). The predictive value of CRP was found in apparently healthy subjects (3, 4), in patients with established CVD (5), in several subgroups of the general population (6) and both in men and women (7).
In healthy subjects even a moderate increase of hsCRP within the normal range (hsCRP <5 mg/L) is considered to be predictive for a variety of cardiovascular events, independent from other cardiovascular risk factors (1, 2, 10). The mechanism responsible for this acute phase response in CVD is not yet completely understood. The association between inflammatory markers and other risk factors of CVD, such as age, gender, smoking habits, obesity, diabetes mellitus, education level and social class, low and high-density lipoprotein-cholesterol, high levels of triglycerides, insulin resistance and physical activity supports the idea that the inflammatory markers might be the expression of intermediate mechanisms (7, 9-11).
In order to prevent the incidence of CVD effectively, it is important to weigh the influence of each risk factor on the cardiovascular system. In this context, it must be taken into consideration that various cardiovascular factors are not independent of one another, but have direct or indirect relations (7). For example, the prevalence of hypertension increases with age and hyperlipidemia or glucose intolerance lead to hypertension, which is another main risk factor for coronary heart disease. Effective prevention of CVD should be started with unraveling the network of multiple risk factors (7). The reduction of cardiovascular risk by lifestyle changes, such as diet, weight loss, exercise and smoking cessation has been linked to lower hsCRP levels (11, 12).
In this respect, the relation of inflammation markers to other risk factors are not well understood. Few studies, however, have explored interrelations between levels of CRP and other cardiovascular risk factors, and data from these reports have been inconsistent (13). So this study was performed to identify the relationship between serum hsCRP and traditional cardiovascular risk factors of the community health-check survey participants in a rural area.
Two-hundred two subjects participated the questionnaire survey and health examination program and aged 50 and over years. They are residents in Changneong, Singi, Mokchon, Pyungsa and Singeon villages of Suncheon city, Jeollanamdo. They are supposedly interested in their health state because they voluntarily applied to this survey program. Of 202 subjects examined in this study, few subjects had diseases history (coronary heart disease, stroke, chronic renal failure, cancer, etc.) except hypertension and plasma levels of log-transformed hsCRP were not different between subjects without diagnosed diseases and subjects with diseases. So we analyzed all 202 subjects who participated in this survey.
The program of this study included the questionnaire survey, physical examination and laboratory examinations, such as, blood cell counts, blood lipid profiles and blood chemistry. The physical examination and blood sampling were performed by trained study staffs who were composed of medical student, nursing students and nurses.
Information about socio-demographic variables such as age, sex, educational level, socioeconomic status, marital status, experiences of cigarette smoking and alcohol consumptions was obtained by a self-administered questionnaire. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). Blood pressure was measured twice on at least 5-min interval by mercury sphygmomanometer with the subject in a sitting position and the averaged value was used for analyses.
Antecubital venous blood was collected into a plain tube and a tube containing EDTA (1 mg/mL) in the morning after the subjects had fasted overnight. Plasma was separated by centrifugation at 4℃ and stored at -80℃ until assayed. Routine laboratory tests, including blood cell counts, blood lipid profiles and blood chemistry, were performed using automatic analyzers. Plasma levels of hsCRP were measured by a immunoturbidimetry on Cobas Integra 700 analyser (Roche, Germany). For hsCRP, we used reagents containing specific monoclonal (CRP) antibody coated to polystyrene particles (Roche).
SPSS, version 9.0 (SPSS Inc., Chicago, IL, U.S.A.) was used for all statistical calculations. Characteristics of the study subjects were expressed by means and standard deviations for continuous variables. Categorical variables were presented as absolute and relative frequencies. Due to the skewed distribution of hsCRP levels, we used its natural log-transformation in the analysis and presented geometric mean and geometric standard deviation. Comparisons between general and clinical characteristics and sex were performed by Student t-test and chi-square test. Natural log-transformed hsCRP levels of three or more groups were compared using analysis of variance (ANOVA) followed by Scheffe's post hoc test. Correlation coefficients between hsCRP and continuous variables were calculated by Pearson's correlation analysis and partial correlation coefficients were computed after adjustment for age. Finally stepwise multiple linear regression analysis was used to evaluate relationships between hsCRP and cardiovascular risk factors. The dichotomous variable such as smoking experience was put into categories, 0 (no) and 1 (yes). A p-value of <0.05 was considered to indicate statistical significance.
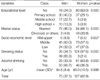
General characteristics of the 202 subjects, 75 men and 127 women, are listed in Table 1. There were statistically different distributions in general characteristics between men and women. In particular, men had higher educational level, more married status, more frequent smoking and alcohol drinking experiences.
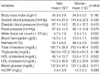
There were well-expected differences in physical and laboratory findings between men and women. Men had higher white blood cell count, hemoglobin, hematocrit, and total cholesterol levels and lower HDL-cholesterol and LDL-cholesterol levels than women. HsCRP levels, however, was not significantly different between men and women (Table 2).
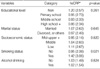
Table 3 shows geometric means and geometric standard deviations of hsCRP levels according to general characteristics. HsCRP levels were significantly higher in persons who had smoking experience.
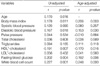
Table 4 shows the results of unadjusted and age-adjusted correlation analyses of factors relating to log-transformed hsCRP level. Plasma hsCRP level had significant positive correlation with age, body mass index, diastolic blood pressure, fasting blood glucose and white blood cell counts. Although the correlation between plasma hsCRP and HDL-cholesterol was negatively significant, other blood lipid profile, such as total cholesterol, triglyceride and LDL-cholesterol did not significantly correlate with hsCRP. Adjustment for age had minimal impact on these association.
The results of stepwise multiple regression analysis is shown in Table 5. In stepwise multiple regression analysis, white blood cell counts, age, fasting blood glucose, smoking and body mass index remained as factors showing independent association with plasma hsCRP, and these factors accounted for 16.5% of the variance in hsCRP levels.
Several prospective epidemiologic studies have demonstrated a positive association between CRP levels and the risk of future cardiovascular disease (14). Risk factors of cardiovascular diseases are often related to one another. For example, hypertension is often associated with glucose intolerance and hypercholesterolemia. Simple reduction of blood pressure or lowering of serum lipids alone may reduce the risk of cardiovascular diseases to some extent (15). Therefore, in order to prevent the occurrence of cardiovascular diseases more effectively, comprehensive reductions of cardiovascular risk factors should be considered, and it is important to understand the interrelationship of each risk factor (7).
With regard to the pathogenesis of cardiovascular diseases, the inflammatory response is now considered to be independent risk factor to the development of cardiovascular diseases (16). Especially inflammatory components are believed to contribute greatly to instability and rupture of atheromatous plaque that leads to atherothrombotic events (17, 18).
CRP is an acute phase reactant, which is marker for underlying systemic inflammation. When measured with a high sensitivity assay, CRP levels also appear to have predictive value for cardiovascular morbidity and mortality. Moreover, baseline levels of CRP predict the risk of future myocardial infarction, stroke, and peripheral atherosclerosis, even after adjustment for other known cardiovascular risk factors (14).
So in this study, we investigated the factors relating to the plasma hsCRP level. As a result of our analysis, white blood cell counts, age, fasting blood glucose, smoking and body mass index are the independent factors relating to plasma hsCRP level. In addition, blood pressure (BP) and HDL-cholesterol level also had significant correlations with plasma hsCRP. These results are consistent with current evidence supporting the importance of inflammation in atherogenesis. Similarly, these data suggest important relationships between inflammation and traditional cardiovascular risk factors.
Inflammation has been hypothesized to play a role in the development of hypertension, and several cross-sectional studies demonstrate higher CRP levels among those individuals with elevated BP (14, 19, 20). CRP has been reported to decrease production of nitric oxide by endothelial cells, and thus might indirectly promote vasoconstriction, leukocyte adherence, platelet activation, oxidation, and thrombosis. CRP also has been reported to have proatherosclerotic properties by upregulating angiotensin type I receptor expression, affecting the renin-angiotensin system and contributing to the pathogenesis of hypertension (21, 22).
In those studies (14, 19, 20), CRP has been more strongly associated with systolic BP than diastolic BP, which is consistent with the emerging importance of systolic BP as a means of cardiovascular risk prediction. But in this study, diastolic BP was more strongly correlated with CRP than systolic BP, and BP was not associated with hsCRP in multivariate analysis.
It is conceivable that components of insulin resistance syndrome, such as hypertension, glucose intolerance and dyslipidemia promote atherosclerosis which involves inflammatory process (7). In our study, blood glucose and diastolic blood pressure was associated with levels of plasma hsCRP.
Smoking is well supposed to give chemical and oxidative stimuli to the cardiovascular system and cause inflammation (13). It has recently been reported that moderate alcohol consumptions reduces circulating CRP (23). But in the present study, when we divided the subjects according to the alcohol drinking status, the plasma hsCRP level was not significantly affected by the alcohol drinking.
We know from literature that CRP has been positively associated with body weight and fatness in men and women of different ages (24-26). More precisely, central obesity and the presence of visceral adipose tissue might be a key promoter of low-grade chronic inflammation (24). Fat cells produce cytokines, in particular IL-6 that induces the synthesis of CRP by the liver. This may be of pathogenic significance as CRP stimulates the uptake of LDL by macrophages, induces complement activation which may cause cellular damage in the artery, and enhances monocyte production of tissue factor, thus enhancing the risk of thrombosis (25). A recent study suggested that both in cross-sectional and in longitudinal studies body mass index but not physical activity is associated with CRP (27). These results are similar to the results we found in multivariate analysis.
We analysed that CRP was negatively related to HDL-cholesterol in correlational analysis, but it was no longer significant after control for other risk factors. The negative association between CRP and HDL-cholesterol might be explained by interaction between CRP and very low density lipoproteins (28).
Several limitations of these data should be taken into account. First, because of the cross-sectional design, relationships between hsCRP and other cardiovascular risk factors cannot be deemed causal in nature. Additionally, it is impossible that unmeasured variables may account for the relationships observed. Last, because our study subjects consisted of a relatively healthy and older volunteer population in a rural area, caution should be exercised when generalizing these data to other general populations. Despite these limitations, inherent with any cross-sectional studies, our results are consistent with known previous reports and are supported by biological plausibility.
In summary, CRP are independently related to several clinical cardiovascular risk factors among general population in some rural area. Further what we need now are prospective studies to evaluate the association of C-reactive protein concentrations with subsequent cardiac events.
Figures and Tables
References
1. Danesh J, Whincup P, Walker M, Lennon L, Thomson A, Appleby P, Gallimore J, Pepys MB. Low grade inflammation and coronary heart disease: prospective study and updated meta-analysis. BMJ. 2000. 321:199–204.
2. Rifai N, Ridker PM. High-sensitivity C-reactive protein: a novel and promising marker of coronary heart disease. Clin Chem. 2001. 47:403–411.

3. Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997. 336:973–979.

4. Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000. 342:836–843.

5. Haverkate F, Thompson SG, Pyke SD, Gallimore JR, Pepys MB. European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. Production of C-reactive protein and risk of coronary events in stable and unstable angina. Lancet. 1997. 349:462–466.

6. Kuller LH, Tracy RP, Shaten J, Meiahn EN. Relation of C-reactive protein and coronary heart disease in the MRFIT nested case-control study. Multiple Risk Factor Intervention Trial. Am J Epidemiol. 1996. 144:537–547.
7. Saito M, Ishimitsu T, Minami J, Ono H, Ohrui M, Matsuoka H. Relations of plasma high-sensitivity C-reactive protein to traditional cardiovascular risk factors. Atherosclerosis. 2003. 167:73–79.

8. Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002. 105:1135–1143.

9. Hak AE, Stehouwer CD, Bots ML, Polderman KH, Schalkwijk CG, Westendorp IC, Hofman A, Witteman JC. Associations of C-reactive protein with measures of obesity, insulin resistance, and subclinical atherosclerosis in healthy, middle-aged women. Arterioscler Thromb Vasc Biol. 1999. 19:1986–1991.

10. Geffken D, Cushman M, Burke GL, Polak JF, Sakkinen PA, Tracy RP. Association between physical activity and markers of inflammation in a healthy elderly population. Am J Epidemiol. 2001. 153:242–250.

11. Heilbronn LK, Clifton PM. C-reactive protein and coronary artery disease: influence of obesity. J Nutr Biochem. 2002. 13:316–321.
12. Tchernof A, Nolan A, Sites C, Ades PA, Poehlman ET. Weight loss reduces C-reactive protein levels in obese postmenopausal women. Circulation. 2002. 105:564–569.

13. Mendall MA, Patel P, Ballam L, Strachan D, Northfield TC. C-reactive protein and its relation to cardiovascular risk factors: a population based cross sectional study. BMJ. 1996. 312:1061–1065.
14. Rohde LE, hennekens CH, Ridker PM. Survey of C-reactive protein and cardiovascular risk factors in apparently healthy men. Am J Cardiol. 1999. 84:1018–1022.

15. Reaven GM. Insulin resistance and compensatory hyperinsulinemia: role in hypertension, dyslipidemia, and coronary heart disease. Am Heart J. 1991. 121:1283–1288.

16. Ross R. Atherosclerosis-an inflammatory disease. N Engl J Med. 1999. 340:115–126.
17. van der Wal AC, Becker AE, van der Loos CM, Das PK. Site of intimal rupture or erosion of thrombosed coronary athersclerotic plaques is characterized by an inflammatory process irrespective of the dominant plaque morphology. Circulation. 1994. 89:36–44.
18. Maseri A. Inflammation, atherosclerosis, and ischemic events - exploring the hidden side of the moon. N Engl J Med. 1997. 336:1014–1016.

19. Sesso HD, Bruing JE, Rifai N, Blake GJ, Gaziano JM, Ridker PM. C-reactive protein and the risk of developing hypertension. JAMA. 2003. 290:2945–2951.

20. Bermudez EA, Rifai N, Buring J, Manson JE, Ridker PM. Interrelationships among circulating interleukin-6, C-reactive protein, and traditional cardiovascular risk factors in women. Arterioscler Thromb Vasc Biol. 2002. 22:1668–1673.

21. Devaraj S, Xu DY, Jialal I. C-reactive protein increases plasminogen activator inhibitor-1 expression and activity in human aortic endothelial cells; implications for the metabolic syndrome and atherothrombosis. Circulation. 2003. 107:398–404.
22. Wang CH, Li SH, Weisel RD, Fedak PW, Dumont AS, Szmitko P, Li RK, Mickle DA, Verma S. C-reactive protein upregulates angiotensin type 1 receptors in vascular smooth muscle. Circulation. 2003. 107:1783–1790.

23. Imhof A, Froehlich M, Brenner H, Boeing H, Pepys MB, Koenig W. Effect of alcohol consumption on systemic markers of inflammation. Lancet. 2001. 357:763–767.

24. Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Elevated C-reactive protein levels in overweight and obese adults. JAMA. 1999. 282:2131–2135.

25. Heilbronn L, Clifton PM. C-reactive protein and coronary artery disease: influence of obesity, caloric restriction and weight loss. J Nutr Biochem. 2002. 13:316–321.

26. Hwang JS, Lee SH, Park HS. The association between C-reactive protein and obesity among Korean men. J Assoc Fam Med. 2003. 24:58–63.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download