Abstract
We analyzed the prostate cancer data of 317 Korean men with clinically localized prostate cancer who underwent radical prostatectomy at Asan Medical Center between June 1990 and November 2003 to construct nomograms predicting the pathologic stage of these tumors, and compared the outcome with preexisting nomograms. Multinomial log-linear regression was performed for the simultaneous prediction of organ-confined disease (OCD), extracapsular extension (ECE), seminal vesicle invasion (SVI) and lymph node metastasis (LNM) using serum prostate-specific antigen (PSA), Gleason score and clinical stage. Nomograms representing percent probabilities were constructed and compared with those presented by Partin et al. by calculating areas under the receiver operating characteristics (ROC) curves. Median serum PSA at surgery was 10.8 ng/mL, and median biopsy Gleason score was 7. Overall OCD, ECE, SVI and LNM rates were 59.6%, 20.5%, 11.7% and 8.2%, respectively, and areas under the curves were 0.724, 0.626, 0.662, and 0.794, respectively. Pathologic stage of localized prostate cancer in Korean men may be predicted using the Partin table, with acceptable accuracy for OCD and LNM, but less so for ECE and SVI.
Surgery for clinically localized prostate cancer is most effective when the cancer is organ- or specimen-confined (1). Much effort has therefore been expended on the accurate preoperative prediction of the final pathologic stage of the tumor, the single most important prognostic indicator. Using serum prostate-specific antigen (PSA), biopsy Gleason score and clinical stage, as well as a variety of other clinical variables and their combinations, pretreatment nomograms have been constructed for the prognosis of these tumors (1-9). Although these nomograms have aided clinicians in counseling patients and selecting optimal treatment methods, the validity and general applicability of these tables have been questioned, especially in regard to their extrapolation to populations and groups other than those in which the nomograms were originally constructed (4, 10, 11).
The incidence of prostate cancer in Korean men has been increasing, necessitating the construction of nomograms based on Korean data. When compared with age-matched men in Western countries, Korean men have lower normal ranges of serum PSA (12) and smaller average prostate gland volumes. To generate prediction nomograms for Korean men, we have analyzed prostate cancer data from a single institute and compared nomograms constructed from these data with preexisting nomograms (1). Furthermore, we have assessed the applicability of these nomograms to the Korean population and determined the necessity of nomograms based solely on Korean data.
A total of 317 Korean men (mean age 64.3 yr, range 40 to 83) with clinically localized prostate cancer who underwent radical retropubic prostatectomy and bilateral pelvic lymphadenectomy at Asan Medical Center between June 1990 and November 2003 were the subjects of this study. Inclusion criteria included a pre-biopsy serum PSA level (Hybritech Tandem-CIS assay) and transrectal ultrasonography or digital guided sextant or ten-site prostate needle biopsy and/or transurethral resection of the prostate, with preoperative histological grade according to the Gleason histological scoring system. Patients who had received any form of neoadjuvant hormonal therapy were excluded. Using the preoperative variables, all patients were assigned a clinical stage in accordance with the TNM system (1997).
Radical prostatectomy specimens were examined microscopically in histological sections at multiple levels after routine fixation. Briefly, each surgical specimen was weighed and its external surface was covered in India ink before fixing in 10% formalin. The prostate gland and seminal vesicles were step-sectioned perpendicular to the apical-basal axis for examination. Pathological stages were assigned in accordance with the TNM system (1997). All lymph nodes were analyzed by routine paraffin sections in addition to previous frozen sections. Critical pathological parameters considered as diagnostic of organ confinement status were extracapsular extension (ECE), seminal vesicle invasion (SVI) and lymph node metastasis (LNM). Patients with negative surgical margins, no ECE, no SVI and no LNM were considered to have organconfined disease (OCD).
Using the three preoperative variables, serum PSA, biopsy Gleason scores and clinical stage, a multinomial log-linear regression was performed to predict the percent probability of OCD, ECE, SVI and LNM. The nomograms were constructed from the predicted percent probabilities at 95% confidence intervals for the final model. Internal validation was analyzed from 1000 additional bootstrap samples to determine sensitivity, specificity, positive predictive value and negative predictive value. For comparison with preexisting nomograms, receiver-operating-characteristics (ROC) curves were drawn, and the areas under the curves (AUC's) were calculated, using the nomograms presented by Partin et al. (1). All statistical analyses were performed using SPSS for Windows, version 11.5.
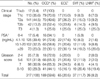
The distribution of the patients and their final pathological findings with respect to each clinical parameter are shown in Table 1. At the time of surgery, the median serum PSA was 10.8 ng/mL, and the median biopsy Gleason score was 7. Overall OCD, ECE, SVI and LNM rates were 59.6%, 20.5%, 11.7% and 8.2%, respectively.
Of the 317 patients, 17 (5.4%) had clinical stage T1a or T1b, 113 (35.6%) had T1c, 183 (57.7%) had T2 and only 4 (1.3%) had T3. Noticeably, all cases of clinical stages T1a and T1b had OCD. Clinical stage T2a and T2b tumors showed similar findings on all the pathological parameters examined. OCD in clinical stage T2a and T2b tumors was markedly reduced, to 49.6% and 52.4% respectively, when compared with the 100.0% and 70.0% observed in stage T1a,b and T1c tumors (p<0.05). Of the 317 men, 17 (5.4%) had preoperative serum PSA levels of 4.0 ng/mL or less, a value generally considered the normal cutoff; 16 of these 17 patients (94.1%) had OCD. In addition, 125 patients (39.4%) had preoperative serum PSA levels between 4.1 and 10.0 ng/mL, 102 (32.3%) between 10.1 and 20.0 ng/mL and 73 (23.0%) higher than 20.0 ng/mL. Gleason scores below 7 were observed in 126 (39.8%) of the 317 patients, whereas 98 (30.9%) had Gleason scores of 7 and 93 (29.3%) had Gleason scores higher than 7.
The results of the multinomial log-linear regression analysis to predict the final pathologic stage from the patients' clinical parameters are shown in Table 2. Numbers represent probability (%) and the dash (-) represents lack of sufficient data to calculate probability. From the internal validation analysis, our model predicted the probability of OCD to 69.6 %, ECE to 75.8%, SVI to 86.2% and LNM to 93.2%. Table 3 shows the sensitivity, specificity, positive predictive value and negative predictive value achieved for various predicted probability cutoff values for OCD when assessed in the 1000 validation bootstrap samples.
With increasing incidence of prostate cancer, continuing controversy surrounds the choice of treatment for men with clinically localized prostate cancer. Although patients with OCD demonstrate markedly improved disease-free survival when compared with men with extraprostatic disease (1, 13, 14), the actual rate of OCD, as determined in pathologic specimens at surgery, is reported to be 60% to 70% at best (10). That is, as many as 30% to 40% of patients with clinically 'localized' prostate cancer receive radical operation unnecessarily. This situation has prompted efforts to develop methods for more accurate preoperative prediction of the final pathologic stage. In the past decade, many prediction tables and plots have been generated based on combinations of preoperative parameters (1-5, 8, 15, 16). However, while aiding physicians in selecting treatment methods, the general applicability of these nomograms has been questioned, especially in regard to their extrapolation to population groups other than those in which they were generated (4, 10, 11).
The increasing incidence of prostate cancer in Korean men has raised the same questions to Korean physicians, especially since Korean patients have clinically distinct characteristics (12). When compared with Caucasian or Japanese men, age-matched Korean men have lower normal serum PSA ranges, and their average total prostate volumes are intermediate between those of Caucasian and Japanese men. In addition, Korean men have a lower cancer probability and detection rate on needle biopsy within the same PSA ranges compared to Caucasians. Conceivably, these distinctive features may limit the usefulness of preexisting nomograms, necessitating verification of their applicability to this population or construction of prediction tables based on data from Korean men only.
We found that 17 of 317 patients (5.4%) had serum PSA levels below 4.0 ng/mL, and that 8 of these patients (47.1%) harbored cancer cells with poor differentiation, as shown by a Gleason score of 7 or higher. Similarly, 69 of 125 patients (55.2%) with serum PSA levels between 4.1 and 10.0 ng/mL had tumors with a Gleason score of 7 or higher, a surprisingly high proportion considering the low serum PSA levels. Likewise, of the 191 patients with a Gleason score of 7 or higher, 77 (40.3%) had serum PSA levels lower than 10.0 ng/mL.
When compared with age-matched Caucasians (1), Korean men showed a higher OCD rate at all PSA concentrations. When matched by Gleason score and clinical stage, Korean men also showed a higher OCD rate, except for those with a Gleason score between 2 and 4. In addition, when compared with Caucasian men, Korean men showed a lower ECE rate at all PSA concentrations, Gleason scores and clinical stages. In contrast, Korean men showed a higher rate of SVI at all PSA ranges and clinical stages, as well as an overall lower rate of LNM. These results indicate that Korean men have a higher rate of OCD, a lower rate of ECE and LNM, and a higher probability of SVI than Caucasian men (1). Although Korean men tend to show a higher probability of OCD, once the disease extends out it tends to invade into the seminal vesicles first. This may be due to the biological aggressiveness of the cancer cells, the relatively smaller volumes of the prostate gland, or the anatomical relationship between the seminal vesicles and the gland, which may facilitate cancer progression at an earlier stage when the tumor mass is smaller.
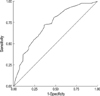
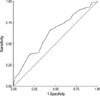
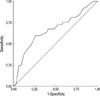
ROC analyses were performed to assess the discriminative ability of the Partin tables. A test is generally considered to have an acceptable discriminative power when the AUCs are higher than 0.7 on an ROC curve. AUCs regarding OCD and LNM were 0.724 and 0.794. Thus, despite the apparent differences in preoperative parameters and pathological stage, the Partin tables were able to accurately predict OCD and LNM in Korean men. However, the AUC's for ECE and SVI were lower (0.626 and 0.662, respectively), indicating that the Partin tables are less accurate for predicting ECE and SVI in Korean men. As previously mentioned, Korean men have a higher rate of OCD and SVI, but a lower rate of ECE and LNM, compared to the results of Partin et al. (1), but the differences in ECE and SVI were more pronounced than those in OCD and LNM. This may indicate that the prostate cancer characteristics of Korean men are similar to those of Caucasian men or that the larger number of cases integrated in the Partin table contributed to a statistical difference.
The descriptive cancer statistics presented in this study provide representative data that illustrate the characteristics of prostate cancer in Korean men. The prediction nomograms we have generated will assist physicians in counseling Korean men with prostate cancer regarding the probability of their tumor being at a specific pathological stage. Furthermore, these nomograms will assist doctors and their patients to make more informed treatment decisions based on pathological stage, risk tolerance and the values they place on various potential outcomes. In addition, these nomograms may aid in rational selection of patients to undergo radical curative surgery, specifically in Korean men with clinically localized prostate cancer. However, it should be remembered that the data in this study and the nomograms generated come from a single institute, which may limit the applicability of our results. At the present time, a larger multi-institutional study is underway to generate more accurate and representative results.
In conclusion, nomograms predicting the pathologic stage of clinically localized prostate cancer in Korean men have been constructed and validated with accuracy using data from a single institute. With increasing incidence, these nomograms may serve a useful tool in making therapeutic decisions for Korean men with newly diagnosed prostate cancer. A larger scale, multi-center study with validation test is warranted for a more representative data.
Figures and Tables
Fig. 1
Receiver operating characteristics (ROC) curve for organ confined disease (area under the curves [AUC] 0.724).
References
1. Partin AW, Kattan MW, Subong EN, Walsh PC, Wojno KJ, Oesterling JE, Scardino PT, Pearson JD. Combination of prostate-specific antigen, clinical stage, and Gleason score to predict pathological stage of localized prostate cancer: a multi-institutional update. JAMA. 1997. 277:1445–1451.

2. Partin AW, Yoo J, Carter HB, Pearson JD, Chan DW, Epstein JI, Walsh PC. The use of prostate specific antigen, clinical stage and Gleason score to predict pathological stage in men with localized prostate cancer. J Urol. 1993. 150:110–114.

3. Ackerman DA, Barry JM, Wicklund RA, Olson N, Lowe BA. Analysis of risk factors associated with prostate cancer extension to the surgical margin and pelvic node metastasis at radical prostatectomy. J Urol. 1993. 150:1845–1850.

4. Egawa S, Suyama K, Arai Y, Matsumoto K, Tsukayama C, Kuwao S, Baba S. A study of pretreatment nomograms to predict pathological stage and biochemical recurrence after radical prostatectomy for clinically resectable prostate cancer in Japanese men. Jpn J Clin Oncol. 2001. 31:74–81.

5. Badalament RA, Miller MC, Peller PA, Young DC, Bahn DK, Kochie P, O'Dowd GJ, Veltri RW. An algorithm for predicting nonorgan confined prostate cancer using the results obtained from sextant core biopsies with prostate specific antigen level. J Urol. 1996. 156:1375–1380.

6. Rogers E, Gurpinar T, Dillioglugil O, Kattan MW, Goad JR, Scardino PT, Griffith DP. The role of digital rectal examination, biopsy Gleason sum and prostate-specific antigen in selecting patients who require pelvic lymph node dissections for prostate cancer. Br J Urol. 1996. 78:419–425.

7. Epstein JI, Walsh PC, Carmichael M, Brendler CB. Pathologic and clinical findings to predict tumor extent of nonpalpable (Stage T1c) prostate cancer. JAMA. 1994. 271:368–374.

8. Narayan P, Gajendran V, Taylor SP, Tewari A, Presti JC Jr, Leidich R, Lo R, Palmer K, Shinohara K, Spaulding JT. The role of transrectal ultrasound-guided biopsy-based staging, preoperative serum prostate-specific antigen, and biopsy Gleason score in prediction of final pathologic diagnosis in prostate cancer. Urology. 1995. 46:205–212.

9. Egawa S, Suyama K, Matsumoto K, Satoh T, Uchida T, Kuwao S, Koshiba K. Improved predictability of extracapsular extension and seminal vesicle involvement based on clinical and biopsy findings in prostate cancer in Japanese men. Urology. 1998. 52:433–440.

10. Blute ML, Bergstralh EJ, Partin AW, Walsh PC, Kattan MW, Scardino PT, Montie JE, Pearson JD, Slezak JM, Zincke H. Validation of Partin tables for predicting pathological stage of clinically localized prostate cancer. J Urol. 2000. 164:1591–1595.

11. Kattan MW, Stapleton AM, Wheeler TM, Scardino PT. Evaluation of a nomogram used to predict the pathologic stage of clinically localized prostate carcinoma. Cancer. 1997. 79:528–537.

12. Ku JH, Ahn JO, Lee CH, Lee NK, Park YH, Byun SS, Kwak C, Lee SE. Distribution of serum prostate-specific antigen in healthy Korean men: influence of ethnicity. Urology. 2002. 60:475–479.

13. Paulson DF. Impact of radical prostatectomy in the management of clinically localized disease. J Urol. 1994. 152:1826–1830.

14. Stein A, deKernion JB, Smith RB, Dorey F, Patel H. Prostate specific antigen levels after radical prostatectomy in patients with organ confined and locally extensive prostate cancer. J Urol. 1992. 147:942–946.

15. Puppo P, Perachino M. Clinical stage, prostate-specific antigen and Gleason grade to predict extracapsular disease or nodal metastasis in men with newly diagnosed, previously untreated prostate cancer. Eur Urol. 1997. 32:273–279.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download