Abstract
Our previous studies document the expression of adrenoceptors and purinoceptors in the rat prostate neuroendocrine cells (RPNECs). However, a direct investigation of the receptors for acetylcholine (ACh) is still lacking in the prostate neuroendocrine cells. RPNECs were freshly isolated from the ventral lobes of rat prostate by using collagenase. Effects of ACh and various muscarinic antagonists on the intracellular Ca2+ concentration ([Ca2+]c) were investigated by using the fura-2 spectrofluorimetry. Single-cell RT-PCR analysis was applied to identify the transcripts for the muscarinic receptor subtypes. ACh (5 µM) induced a sharp transient increase in the [Ca2+]c of RPNECs, which was independent of the extracellular Ca2+. In the same RPNECs, high KCl (60 mM), phenylephrine (5 µM), UTP (P2Y1/2 agonist, 50 µM), and α,β-meATP (P2X1/3 agonist, 0.5 µM) also increased the [Ca2+]c. The ACh-induced [Ca2+]c change (Δ[Ca2+]c) was blocked by atropine or by para-fluorohexahydrosiladifenidol (M3 antagonist, 0.3 µM), but not by telenzepine (M1 antagonist, 1 µM) and himbacine (M2 and M4 antagonist, 1 µM). The single-cell RT-PCR demonstrated the selective expression of mRNAs for M3 in RPNECs. In summary, RPNECs express M3 muscarinic receptors that are linked to the release of Ca2+ from intracellular stores. The Ca2+ signals of RPNECs might mediate the parasympathetic regulation of prostate gland.
The prostate gland consists of a complex glandular ductal system lined with exocrine epithelial cells, basal cells and neuroendocrine cells embedded in a fibromuscular stromal matrix (1, 2). The secretory epithelial cells in the prostate produce the bulk of human seminal fluid. Neuroendocrine cells in the prostate gland are serotonin- and peptide-containing cells, which are part of a dispersed neuroendocrine regulatory system, called APUD (amine precursor uptake and decarboxylation) system. The functional role of prostate neuroendocrine cells are supposed to be involved in normal prostate growth, benign hyperplasia and cancer development (3-5).
The physiological and pathophysiological function of prostate is under the control of autonomic nervous system as well as the hormonal state (6, 7). The secretion of prostatic fluid, for example, is positively regulated by acetylcholine via muscarinic receptors in the secretory epithelial cells (8, 9). On the other hand, α1-adrenergic stimulation induces the smooth muscle contraction that would help the secreted fluid to be expelled from the lumen of gland (8, 9). The α1-AR mediated smooth muscle contraction has been the rational ground for the use of α1-blockers to relieve the symptom of benign prostatic hyperplasia.
In previous studies, we firstly investigated the physiological and pharmacological properties of various types of single prostate cells encompassing secretory epithelial cell (11, 12), smooth muscle cell (13) and neuroendocrine cells (14-16). After an enzymic digestion of the ventral lobe of rat prostate, the chromogranin-A positive round-shaped cells (putative neuroendocrine cells) are discriminated from the columnar epithelial cells. The putative rat prostate neuroendocrine cells (RPNECs) display typical properties of excitable cells; spontaneous action potentials and voltage-gated Ca2+ currents (14). The pharmacological studies demonstrate that the RPNECs functionally express α1- and α2-adrenergic receptors that are linked to the release of stored Ca2+ and the inhibition of N-type Ca2+ channels, respectively (15). In addition, both ionotropic P2X1 receptors and metabotropic P2Y2 receptors are present in RPNECs and the stimulation of which increases [Ca2+]c via fast Ca2+ influx and stored Ca2+ release, respectively (16).
Compared with the understanding of adrenoceptors and purinoceptors, relatively little is known about the cholinergic effects on prostate neuroendocrine cells. In the neuroendocrine cells from the human adenomatous prostate, the release of histamine is increased two fold by carbachol, which is blocked by the pretreatment with atropine (17). This study indicates the presence of muscarinic receptors in prostate neuroendocrine cells. However, more direct investigation about the effects of acetylcholine on the prostate neuroendocrine cells and the knowledge of the subtype(s) of muscarinic receptors are still lacking.
In the present study, employing the fura-2 fluorescence measurement, we investigated the effects of ACh on [Ca2+]c in freshly isolated RPNECs. Also, a single cell RT-PCR analysis was performed to elucidate the presence of transcripts for a specific subtype of muscarinic receptors in RPNECs.
All procedures on experimental animals were performed in accordance with the guidelines of the Institutional Animal Care and Use Committee (IACUC) of Sungkyunkwan University. Male Sprague-Dawley rats (350-400 g) were killed by 100% CO2 inhalation and the ventral lobe of the prostate gland removed rapidly thereafter. The fibrous capsule was removed and the tissue was cut with scissors into small pieces (1-2 µL) in a phosphate-buffered Ca2+-free Tyrode's solution. The tissue was digested for 25 min at 37℃ in Ca2+-free Tyrode's solution containing collagenase (2 mg/mL, Wako, Japan), trypsin inhibitor (1 mg/mL, Sigma, St. Louis, MO, U.S.A.), bovine serum albumin (3 mg/mL, Sigma) and dithiothreitol (DTT, 1 mg/mL, Sigma). Following digestion and subsequent removal of supernatant, tissue segments were transferred to fresh Tyrode's solution and agitated gently using a fire-polished wide bore (1-2 mm) Pasteur pipette. Isolated cells were isolated daily then stored in fresh solution at 4℃ for up to 6 hr. Dispersed cells were moved into the experiment chamber and examined by using an inverted microscope (IX-70, Olympus, Japan). After the digestion procedure, most of isolated single cells had elongated columnar shape, a typical feature of secretory epithelial cells. Besides columnar cells, we could identify round or oval shape cells with relatively dark cytoplasm that were regarded as RPNECs in the present study. The putative RPNECs were carefully discriminated from damaged or swollen epithelial cells that showed also round or oval shapes but with pale cytoplasm. The reliability of above criteria for identifying RPNECs were assured by constant responses of chosen cells to noradrenaline in [Ca2+]c or to α,β-meATP. Such responses to NA and α,β-meATP are not observed in columnar epithelial cells (15, 16).
Dispersed single cells were loaded with acetoxymethyl ester form of Fura-2 (2 µM) in the Ringer's solution for 20 min at room temperature and then washed out with fresh solution. The putative RPNECs were identified as above criteria, and the region of interest for Fura-2 experiment was set so that the fluorescence from the single RPNEC could be collected selectively. The recording of [Ca2+]c was performed with a microfluorimetric system consisting of an inverted fluorescence microscope (Olympus IX-70, Japan) with a dry-type fluorescence objective lens (×40, NA 0.85), a photomultiplier tube (type R 1527, Hamamatsu, Japan) and Deltascan illuminator (Photon Technology International Inc, Monmouth, NJ, U.S.A.). Light was provided by a 75-W xenon lamp (Ushino, Tokyo, Japan) and a chopper wheel alternated the light path to monochromators (340 and 380 nm) with a frequency of 5 Hz, and intensity of emitted light at 510 nm was measured. As a measure of [Ca2+]c the fluorescence emission ratio at 340 nm/380 nm excitation (F340/380) is presented.
To synthesize first strand cDNA, RPNECs were collected individually by using microelectrodes with inner diameter of about 25-30 µm on the stage of inverted microscope for the patch clamp. After aspiration, the cell was expelled from the pipette into ice cooled 0.2 mL tubes, which contained 2 units of RNase-free DNase (Takara Bio Inc., Shiga, Japan), 40 units of ribonuclease inhibitor (Takara Bio Inc., Otsu, Shiga, Japan), 50 mM Tris-HCl (pH 8.3), 3 mM MgCl2, 75 mM KCl, and 100 mM DTT. The reaction mixture was incubated at 37℃ for 30 min, followed by 95℃ for 5 min. And then reverse transcription reaction was performed in the presence of 0.8 µg of oligo (dT)15 (Roche Applied Science, Indianapolis, IN, U.S.A.), 10 mM each of dATP, dTTP, dGTP and dCCT (Roche Applied Science), and 200 units of SuperScript™ reverse transcriptase (Invitrogen Life Technologies, Carlsbad, CA, U.S.A.). The reaction proceeded for 10 min at 25℃, and for 50 min at 42℃, followed by a 15-min step at 70℃ to inactivate the SuperScript™ reverse transcriptase.
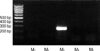
Two rounds of PCR (PTC-0150 MiniCycler™; MJ Research Inc., Waltham, MA, U.S.A.) were performed with outer primers and nested primers of M1, M2, M3, M4, and M5 muscarinic receptors of rat (18, 19). First strand cDNA was used for the first PCR amplification. This mixture was then used for the second nested PCR amplification. PCR reactions were carried out using the 2.5 units of Taq polymerase (Takara Bio Inc.) containing of 10 mM Tris-HCl (pH 8.3), 50 mM KCl, 1.5 mM MgCl2, 10 mM each of dATP, dTTP, dGTP and dCCT, 100 pM each of sense and antisense primers, and DNA template. Temperature cycling proceeded as follows: 1 cycle at 95℃ for 5 min and 45 cycles at 95℃ for 60 sec, 50℃ (for M4) or 55℃ (for M1, M2, M3, M5) for 60 sec, and 72℃ for 60 sec, followed by 72℃ for 10 min. PCR products were then subjected to gel electrophoresis on a 1.5% agarose gel containing ethidium bromide. Primers for the PCR of M1, M2, M3, M4, and M5 are as follows: M1 sense, 5'-GCA CAG GCA CCC ACC AAG CAG-3'; M1 antisense, 5'-AGA GCA GCA GCA GGC GGA ACG-3'; M2 sense, 5'-GGC AAG CAA GAG TAG AAT AAA-3'; M2 antisense, 5'-GCC AAC AGG ATA GCC AAG ATT-3'; M3 sense, 5'-CAC AGG CAG TTC TCG AAG CT-3'; M3 antisense, 5'-AGG ACG GTA GCT TGG TAG AG-3'; M4 sense, 5'-AGT GCT TCA TCC AGT TCT TGT CCA-3'; M4 antisense, 5'-CAC ATT CAT TGC CTG TCT GCT TTG-3'; M5 sense, 5'-CTC ATC ATT GGC ATC TTC TCC A-3'; M5 antisense, 5'-GGT CCT TGG TTC GCT TCT CTG T-3'; M1 nested sense, 5'-CCT CCC AAA AGC TCC CCA-3'; M1 nested antisense, 5'-TGT CCC GGA AGG CTT TGT-3'; M2 nested sense, 5'-GAA GGA AAA GAA GGA ACC TGT-3'; M2 nested antisense, 5'-GTC CTG GTC ACT TTC TTT TCC-3'; M3 nested sense, 5'-CTC GAA GCT GTA GCA GCT ATG-3'; M3 nested antisense, 5'-GGA GCT ATG GCC TGG ACG CTT GAG G-3'; M4 nested sense, 5'-ACC CGG CAG TGA CCT TTG-3'; M4 nested antisense, 5'-TTA CAA TTT GAA TCT TGG ACC AT-3'; M5 nested sense, 5'-GAA CCT CTA CAC GAC CTA CAT C-3'; M5 nested antisense, 5'-CCC GGT AGA TCC GGC AGT AG-3'.
All the experiments were performed in phosphate-buffered
saline (PBS) containing 145 mM NaCl, 1.6 mM K2HPO4, 0.4 mM KH2PO4, 1 mM MgCl2, 2 mM CaCl2 and 5 mM D-glucose at pH 7.4 titrated with NaOH. CaCl2 was omitted in the enzymatic isolation of single prostate cells.
The following drugs were used: acetylcholine chloride, para-fluoro-hexahydrosiladifenidol (pF-HHSiD) hydrochloride, 4-hydroxy-2-butynyl-1-trimethylammonium-m-chlorocarbamilate chloride (McN-A-343), telenzepine dihydrochloride, himbacine hydrochloride, and 4-diphenyl acetoxy-N-methyl piperidine methobromide (4-DAMP) (Sigma-Aldrich, Seoul, Korea). All other drugs except pF-HHSiD were dissolved in distilled water. Stock concentration (1 mM) of pF-HHSiD was prepared in dimethylsulfoxide. Dilutions to working concentrations were made in PBS solution.
The data are presented as original recordings, current-voltage (I-V) curves, histograms and bar graphs of mean±S.E.M. (for n cells tested). When necessary, Student's t-test for paired samples was applied, since the control and test recordings were made from the same cell. Probability value below 0.05 (p<0.05) was regarded as significant.
Among the dispersed prostate cells, we could discriminate the putative neuroendocrine cells with a round shape and relatively dark cytoplasm from the columnar epithelial cells and the thin smooth muscle cells as has been described previously (12, 14-16). The Fura-2 fluorescence ratio (F340/380, see Materials and methods) was measured in RPNECs. An application of ACh (5 µM) induced a transient increase in [Ca2+]c which is followed by a plateau-like level above the control (Fig. 1). In the same RPNECs, the effects of high K+ (60 mM), phenylephrine (PhE, 5 µM), UTP (20 µM), and α,β-meATP (0.5 µM were confirmed since the adrenergic and purinergic (both P2X and P2Y) stimulations as well as the membrane depolarization increase the [Ca2+]c of RPNECs (15, 16). Summary of Ca2+ responses to various stimuli demonstrate that the effect of ACh is stronger than the KCl-induced depolarization (p< 0.05) and similar with the responses to PhE, UTP and α,β-meATP (Fig. 1B).
The ACh-induced increase in [Ca2+]c (ACh-Δ[Ca2+]c) was not affected by the removal of extracellular Ca2+ (Fig. 2A), indicating a mechanism of Ca2+ release from the intracellular stores (e.g. endoplasmic reticulum). In the adrenal chromaffin cells, ACh activates nicotinic ionotropic receptors that induce membrane-depolarization as well as direct Ca2+ influx (20). In RPNECs, however, the pretreatment with atropine (1 µM), a representative antagonist of muscarinic receptors, completely blocked ACh-Δ[Ca2+]c (Fig. 2B). This result excludes the involvement of nicotinic ACh receptors in RPNECs (Fig. 2B).
To identify the subtype(s) of muscarinic receptors in RPNECs, effects of subtype-specific pharmacological agents were examined (21, 22). A pretreatment with telenzepine (1 µM), an M1-sepecific antagonist, did not affect the amplitude of the ACh-Δ[Ca2+]c (93±9.0% of control, n=4, Fig. 3A). Also, the M1-specific agonist (McN-A-343 1 µM) had no effect on the [Ca2+]c of RPNECs (Fig. 3B, n=3). In the same RPNEC where telezepine had negligible effect, a pretreatment with pF-HHSiD (0.3 µM), a specific M3 antagonist, completely blocked the ACh-Δ[Ca2+]c in a reversible manner (Fig. 3A, n=5). A lower concentration of pF-HHSiD (0.1 µM) showed partial inhibitory effects (38±20.5% of control, n=4). Also, 4-DAMP (1 µM), another subtype-selective antagonist for M3 receptors, blocked the ACh-Δ[Ca2+]c (n=2, data not shown). Finally, himbacine (1 µM), an antagonist for M2 and M4 receptors, showed a partial inhibitory effect on the ACh-Δ[Ca2+]c (Fig. 3C, 64±9.1% of control, n=5).
Next, to further identify the muscrainic receptor subtype in RPNECs, a nested RT-PCR was performed with isolated RPNECs (see Materials and methods). Among the tested primers, only the M3-specific pairs showed a positive result (Fig. 4). The same results were confirmed in three separate experiments.
The present study demonstrates the existence of M3 subtype of muscarinic receptors in the RPNECS. The stimulation of muscarinic receptors evoked a strong release of Ca2+ from intracellular stores of RPNECs, similar with the actions of P2Y2 and α1-adrenergic stimulations in the same neuroendocrine cells (15, 16). Muscarinic ACh receptors belong to a family of G protein-coupled receptors. Molecular cloning studies have identified five muscarinic subtypes that are highly homologous but distinct gene products. Among them the M1, M3 and M5 receptors are coupled to Ca2+/phospholipid second messenger system (22).
The prostate is richly innervated by both noradrenergic and cholinergic fibers (7). Cholinergic stimulations are known to regulate diverse physiological functions such as regulating the force and rate of heart, smooth muscle contraction, glandular secretory activity, cell growth and proliferation (23, 24). The majority of muscarinic receptors in the prostate is located in the glandular epithelium but is also detectable in stromal tissue (25, 26). The presence of M3 muscarinic receptors in rat prostate has been previously suggested from the radioligand binding assay and the density of M3 receptors decreases in aged rats (27). However, that study was performed with the whole prostate gland whereas our present study demonstrates the specific presence of M3 receptors in the neuroendocrine cells.
Consistent with the major location of muscarinic receptors, in vivo activation of muscarinic receptors within the prostate gland causes glandular secretion in the dog and rat (9, 10, 28). In fact, the stimulation of secretory epithelial cells of rat prostate with ACh induced an increase of [Ca2+]c with concomitant activations of K+ channels and Cl- channels, both are indispensable for the fluid secretion in various exocrine glands (11, 12). Muscarinic receptor activation also stimulated exocrine secretion of epidermal growth factor in the rat prostate (29). Acetylcholine also causes contraction of prostate smooth muscle from rabbits, pigs, rats and guinea pigs (30-32). However, the contractile effect often requires very high concentration of ACh (e.g. >0.1 mM in guinea pig) and is much smaller than the contractile responses produced by α-adrenoceptor agonists.
Recently, there is evidence that muscarinic receptor activation plays a role in cell growth in the prostate gland, and the mitogenic effects of muscarinic stimulation has been proposed (7, 23). Also, carbachol was found to increase [3H]-thymidine uptake in the prostate tumour LNCaP cell line (23). Considering the potential role of neuroendocrine cells in the growth of prostate gland, the regulation of paracrine/endocrine secretion from the neuroendocrine cells by autonomic nerves could be a crucial step in physiological functioning of the prostate gland. The present study focuses on the effects of muscarinic stimulations on the Ca2+ signaling in RPNECs. In RPNECs, the stimulation of α1 adrenaline receptors changes the membrane potential as well as triggering the InsP3-induced Ca2+ release mechanism (12, 33).
The subtypes of muscarinic receptor in the prostate appear to be species dependent. The reported subtypes responsible for the modification of contractile responses are M1, M2 and M3 for guinea pig, dog and rat prostates, respectively (24). The presence of M3 subtype in rat prostate was deduced from the binding studies and contractile responses to carbachol and muscarinic antagonists. However, a more rigorous antibody study combined with RT-PCR analysis suggests a regional difference depending on the lobe of prostate; the ventral lobe predominantly express M3 receptors whereas the dorsolateral lobes express M2 receptors in rat prostate (34). The neuroendocrine cells investigated in our present study were obtained from the ventral lobes of rat prostate, and the conclusion of M3 receptors in RPNECs is consistent with the previous study of the general pattern of muscarinic receptors in the whole gland (27).
In summary, the RPNECS express M3 subtype of muscarinic receptors, the stimulation of which evoked a strong Ca2+ signal. Considering the general role of neuroendocrine cells in visceral organs, a part of the physiological effects triggered by acetylcholine released from terminal nerves inside the prostate may be mediated by the stimulation of neuroendocrine cells.
Figures and Tables
Fig. 1
Ca2+ responses to various agonists in RPNECs. (A) representative traces of F340/380 demonstrating the effects of PhE (5 µM), UTP (20 µM), ACh (5 µM) and α,β-meATP (0.5 µM) on [Ca2+]c of an RPNEC. The results demonstrated in this figure were obtained from the same cell. (B) Summary of the extent of changes in fluorescence ratio (ΔF340/380) by various agonists and potassium-induced depolarization (KCl 60 mM). The number of tested cells are five to ten for each bar, respectively.

Fig. 2
ACh stimulates muscarinic receptors coupled to store Ca2+ release in RPNECs. (A) ACh induced increase in F340/380 is repeated in the presence and absence of extracellular Ca2+. (B) The ACh-induced ΔF340/380 is completely blocked by the application of atropine (1 µM), which is partially reversed by washout of atropine.

Fig. 3
M3 subtype of muscarinic receptors in RPNECs. (A) ACh (5 µM) was repetitively applied (closed bars) while measuring the F340/380 in RPNECs. The pretreatment with pF-HHSiD (0.3 µM) completely blocks the ACh-induced ΔF340/380. Note that the pretreatment with telenzepine has no effect on ACh-induced ΔF340/380. (B) McN-A-343 (1 µM), an M1-selective agonist, has no effect on [Ca2+]c. (C) The ACh-induced ΔF340/380 is not blocked by the pretreatment with himbacine (1 µM), an antagonist specific to M2 and M4 subtypes.

ACKNOWLEDGEMENT
This research was supported by Grant 03-PJ1-PG3-21400-0007 from the Korea Health 21 Research and Development Project, Ministry of Health and Welfare, Republic of Korea.
References
1. Lee C, Holland JM. Jones TC, Mohr U, Hunt RD, editors. Anatomy, histology, and ultra-structure (correlation with function), Prostate, Rat. Genital System (Monographs on Pathology of Laboratory Animals). 1987. Berlin, Heidelberg: Springer-Verlag;239–251.

2. Xue Y, Smedts F, Verhofstad A, Debruyne F, de la Rosette J, Schalken J. Cell kinetics of prostate exocrine and neuroendocrine epithelium and their differential interrelationship: new perspectives. Prostate Suppl. 1998. 8:Suppl. 62–73.

3. Cockett AT, di Sant' Agnese PA, Gopinath P, Schoen S, Abrahamsson PA. Relationship of neuroendocrine cells of prostate and serotonin to benign prostatic hyperplasia. Urology. 1993. 42:512–519.

4. Abrahamsson PA, Cockett AT, di Sant' Agnese PA. Prognostic significance of neuroendocrine differentiation in clinically localized prostatic carcinoma. Prostate Suppl. 1998. 8:Suppl. 37–42.

5. Hong SJ, Kwon SM, Kim SI, Oh HY, Chung BC. Expression of neuroendocrine cells in benign prostate hyperplasia and the effect of dihydrotestosterone. Korean J Urol. 2003. 44:267–271.
6. Huggins C, Clark PJ. Quantitative studies of prostatic secretion. II. The effect of castration and of estrogenic injections on the normal and on the hyperplastic prostate glands of dogs. J Exp Med. 1940. 72:747–761.
8. Smith ER, Illievski V, Hadidian Z. The stimulation of canine prostatic secretion by pilocarpine. J Pharmacol Exp Ther. 1966. 151:59–65.
9. Wang JM, McKenna KE, Lee C. Determination of prostatic secretion in rats: effect of neurotransmitters and testosterone. Prostate. 1991. 18:289–301.

10. Smith ER. The stimulation of canine prostatic secretion by sympathomimetic amines. J Pharmacol Exp Ther. 1967. 156:227–231.
11. Kim JH, Hong EK, Choi HS, Oh SJ, Kim KM, Uhm DY, Kim SJ. K+ channel currents in rat ventral prostate epithelial cells. Prostate. 2002. 51:201–210.
12. Kim JH, Shin SY, Nam JH, Hong EK, Chung YS, Jeong JY, Kang J, Uhm DY, Kim SJ. Adrenergic regulation of the intracellular [Ca2+] and voltage-operated Ca2+ channel currents in the rat prostate neuroendocrine cells. Prostate. 2003. 57:99–110.
13. Kim JH, Shin SY, Yun SS, Kim TJ, Oh SJ, Kim KM, Chung YS, Hong EK, Uhm DY, Kim SJ. Voltage-dependent ion channel currents in putative neuroendocrine cells dissociated from the ventral prostate of rat. Pflugers Arch. 2003. 446:88–99.

14. Kim SJ, Shin SY, Lee JE, Kim JH, Uhm DY. Ca2+-activated Cl- channel current in rat ventral prostate epithelial cells. Prostate. 2003. 55:118–127.
15. Oh SJ, Kim KM, Chung YS, Hong EK, Shin SY, Kim SJ. Ion channel currents of smooth muscle cells isolated from the prostate of guinea-pig. BJU Int. 2003. 92:1022–1030.
16. Kim JH, Nam JH, Kim MH, Koh DS, Choi SJ, Kim SJ, Lee JE, Min KM, Uhm DY, Kim SJ. Purinergic receptors coupled to intracellular Ca2+ signals and exocytosis in the rat prostate neuroendocrine cells. J Biol Chem. 2004. 279:27345–27356.
17. Polge A, Gaspard C, Mottet N, Guitton C, Boyer JC, Choquet A, Combettes S, Bancel E, Costa P, Bali JP. Neurohormonal stimulation of histamine release from neuroendocrine cells of the human adenomatous prostate. Prostate. 1998. 34:1–9.

18. Iismaa TP, Kerr EA, Wilson JR, Carpenter L, Sims N, Biden TJ. Quantitative and functional characterization of muscarinic receptor subtypes in insulin-secreting cell lines and rat pancreatic islets. Diabetes. 2000. 49:392–398.

19. Lai J, Shao XM, Pan RW, Dy E, Huang CH, Feldman JL. RT-PCR reveals muscarinic acetylcholine receptor mRNA in the pre-Bötzinger complex. Am J Physiol Lung Cell Mol Physiol. 2001. 281:L1420–L1424.
20. Fonteriz RI, Garcia-Sancho J, Gandia L, Lopez MG, Garcia AG. Permeation and inactivation by calcium and manganese of bovine adrenal chromaffin cell calcium channels. Am J Physiol Cell Physiol. 1992. 263:C818–C824.

21. Eglen RM, Watson N. Selective muscarinic receptor agonists and antagonists. Pharmacol Toxicol. 1996. 78:59–68.

22. Hulme EC, Birdsall NJ, Buckley NJ. Muscarinic receptor subtypes. Ann Rev Pharmacol Toxicol. 1990. 30:633–673.

23. Rayford W, Noble MJ, Austenfeld MA, Weigel J, Mebust WK, Shah GV. Muscarinic cholinergic receptors promote growth of human prostate cancer cells. Prostate. 1997. 30:160–166.

24. Ventura S, Pennefather J, Mitchelson F. Cholinergic innervation and function in the prostate gland. Pharmacol Ther. 2002. 94:93–112.

25. Lepor H, Kuhar MJ. Characterization and localization of the muscarinic cholinergic receptor in human prostate tissue. J Urol. 1984. 132:397–402.
26. Ruggieri MR, Colton MD, Wang P, Wang J, Smyth RJ, Pontari MA, Luthin GR. Human prostate muscarinic receptor subtypes. J Pharmacol Exp Ther. 1995. 274:976–982.
27. Yazawa H, Honda K. The M3-muscarinic cholinoceptor subtype in rat prostate and its down regulation by aging. Jpn J Pharmacol. 1993. 61:319–324.

28. Farrel JI. The newer physiology of the prostate gland. J Urol. 1938. 39:171–185.
29. Jacobs SC, Story MT. Exocrine secretion of epidermal growth factor by the rat prostate: effect of adrenergic agents, cholinergic agents, and vasoactive intestinal peptide. Prostate. 1988. 13:79–87.

30. Lau WA, Pennefather JN. Muscarinic receptor subtypes in the rat prostate gland. Eur J Pharmacol. 1998. 343:151–156.

31. Najbar-Kaszkiel AT, Di Iulio JL, Li CG, Rand MJ. Characterization of excitatory and inhibitory transmitter systems in prostate glands of rats, guinea-pigs, rabbits and pigs. Eur J Pharmacol. 1997. 337:251–258.
32. Seki N, Suzuki H. Electrical and mechanical activity of rabbit prostate smooth muscles in response to nerve stimulation. J Physiol (Lond). 1989. 419:651–653.

33. Kim JH, Shin SY, Uhm DY, Kim SJ. Effects of noradrenaline on the membrane potential of prostatic neuroendocrine cells of rat. Korean J Physiol Pharmacol. 2003. 7:47–52.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download