Abstract
A 7-yr-old girl presented with progressive shortening of the right upper arm and limitation of shoulder motion. Pseudohypoparathyroidism associated with Albright's hereditary osteodystrophy was diagnosed by biochemical, hormonal and radiographic studies. Her condition was complicated by severe humerus varus on the right side. Proximal humeral valgization osteotomy and concomitant humeral lengthening resulted in an improvement of the shoulder joint motion and activity in daily life.
Humerus varus is an upper extremity analogue of coxa vara. The radiographic criteria for humerus varus included decreased humeral neck-shaft angle, greater tuberosity overriding the superior margin of the humeral neck, and narrowed proximal humerus width (1). This deformity usually causes a limitation of shoulder motion, especially abduction and flexion, and a shortening of the humerus. Medial physeal arrest, either post-traumatic or post-infectious, of the proximal humerus seems to be the most common cause of this deformity (2). Other etiologies of humerus varus include a number of different hematologic, metabolic diseases and osteochondrodysplasias (3).
Pseudohypoparathyroidism (PHP) is a group of different diseases characterized by resistance to the action of the parathyroid hormone (PTH). Although most of the cases first manifest themselves in the form of hypocalcemic seizures, the skeletal manifestation, which is called Albright's hereditary osteodystrophy (AHO), constitutes a pathognomonic sign in some of the patients affected by PHP. AHO is characterized by short stature, round face, brachydactyly, mental retardation and ectopic calcification (4).
We report a patient with AHO who presented with severe humerus varus, which was treated by valgization osteotomy at the surgical neck of the humerus and concomitant humeral lengthening.
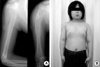
A 7-yr-old girl visited our outpatient clinic complaining primarily of shortening of her left upper extremity and limitation of the right shoulder motion, which were detected 2 yr ago. She had been taken care of by her college-educated mother since birth, who stated that the patient had been very healthy without any serious illness. Her medical record did not show any significant health problem. Her height was 124 cm (70% among the age matched normal population), and her weight was 31 kg (95%). She had a round face and short neck, and her teeth showed signs of yellowish discoloration. Her hands and feet were short and broad, and all of her fingers and her 3rd, 4th and 5th toes of both sides were short. More than 10 subcutaneous calcifications were detected in the hands, chest wall and abdominal wall. A physical examination at age 8 yr and 10 months revealed 10 degrees active and 40 degrees passive forward flexion of the right shoulder. The active and passive abductions of the right shoulder joint were 50 and 100 degrees, respectively. Passive external rotation was 50 degrees on the right and 90 degrees on the left. The distance from the acromion to the cubital crease measured 16 cm on the right side and 21 cm on the left side (Fig. 1A). Radiographic examination showed that the round but flattened humeral head was retroverted with a varus orientation (Fig. 1B). All of the metacarpals and the phalanges of the hand were short and broad with coned epiphyses, while the 3rd, 4th and 5th metatarsals were short as compared with the 1st and 2nd metatarsals (Fig. 1C, D). There was no calcification in either the brain or the kidney, as determined by MRI and ultrasonography.
Biochemical study revealed hypocalcemia (6.9 mg/dL), hyperphosphatemia (8.1 mg/dL) and the serum level of intact parathyroid hormone was 552 pg/mL (reference, 10-65 pg/mL). The thyroid function test showed the presence of a euthyroid state while the serum level of thyroid stimulating hormone (TSH) was elevated to 13.0 IU/mL (reference, 0.4-4.1 IU/mL). Serum levels of lutenizing hormone (LH) and follicle stimulating hormone (FSH) were normal. Her skeletal age was advanced for her chronologic age, and her intelligence quotient was 75 at age 10 yr.
Surgical treatment was performed at age 8 yr and 10 months. Medical treatment with calcium carbonate and active vitamin D3 was started on the day before the operation and continued thereafter. Proximal humeral valgus osteotomy was fixed with Ilizarov apparatus, and the humerus was lengthened at the distal corticotomy site. Under image-intensifier the position of the shoulder joint to obtain the optimal glenohumeral articulation was deteremined to be valgization 65 degrees, internal rotation 30 degrees and forward flexion 10 degrees. Osteotomy was performed at the surgical neck, and the amount of planned correction could be achieved by controlling the Ilizarov rings. Distal corticotomy was made at the distal metaphysiodiaphyseal junction via anterolateral approach, identifying and protecting the radial nerve. After 7 days of latency period, gradual lengthening at a rate of 0.75-1.0 mm/day was carried out. The external fixator was removed at postoperative 5.5 months with an overall length gain of 10 cm, resulting in a healing index of 0.55 month/cm (Fig. 2A). After four years of follow-up, both proximal humeral physes were closed, and the residual shortening of the right humerus was 1.2 cm (Fig. 2B). She could actively abduct her right shoulder to 75 degrees, flex forwardly to 60 degrees. Passive abduction was 120 degrees and passive forward flexion was 150 degrees. The range of motion of the right elbow was not decreased. The patient stated that she had experienced an improvement in her daily life such as face washing, eating and combing.
The main interest of this case lies in the association of the humerus varus with PHP, which is a group of heterogeneous disorders in which the patients exhibit tissue resistance to PTH. Biochemically, it is characterized by hypocalcemia, hyperphosphatemia, and an increased serum PTH level. Patients who are affected by this disorder exhibit a variety of renal cyclic AMP responses to exogenous PTH, have various developmental and skeletal abnormalities collectively referred to as AHO, and exhibit tissue resistance to other hormones such as thyroid-stimulating hormone, gonadotropins and glucagons (5). Many features of AHO seem to be caused by premature and selective closure of specific physes. Although the metacarpals and metatarsals, especially the 4th and 5th, are the most frequently affected bones, it seems that other physes can also be affected. It has been suggested that premature closure of the neural arches and neurocentral synchondroses of the vertebrae cause spinal stenosis in pseudohypoparathyroidism (6).
A molecular genetic study of patients with AHO revealed inactivating mutations in the GNAS1 gene encoding the Gs protein (7, 8), a key component of the G protein complex, which modulates adenylate cyclase and the PTH signal transduction cascade (9). The PTH/PTHrP receptor signal is well known to act on the physeal chondrocytes as a mitogen and inhibitor of terminal differentiation (10). Therefore, it seems probable that the unresponsiveness of the physeal chondrocytes to PTH may contribute to early closure of the physes. However, it has yet to be explained why only certain specific physes show such a phenomenon. In our case, all of the metacarpals, the phalanges of the hands, and the 3rd, 4th and 5th metatarsals were affected, suggesting a high propensity for physeal closure. This makes it all the more likely that the right proximal humeral physis was a consequence of AHO.
However, there is still a possibility in this case, that humerus varus developed as a result of subclinical injury or infection of the proximal physis during the neonatal period. In four patients who developed humerus varus in the series of Ellefsen et al. (2), a proximal humeral injury was not considered or diagnosed during birth although a definite shoulder injury was noted at that time.
Humerus varus resulting from the premature closure of proximal humeral physis is always associated with humeral shortening since about 80% of humeral growth takes place at the proximal physis. Severe varus deformity of the proximal humerus is usually complicated by marked limitation of abduction and forward flexion due to the impingement of the greater tuberosity against the acromion. Corrective wedge osteotomy has been warranted for the functional improvement of the shoulder joint. Tension band wiring (1) or plate and screws (11, 12) were reported as the fixation method for humeral valgization osteotomy. We performed humeral lengthening and valgization osteotomy simultaneously, using an Ilizarov ring fixator. This technique allowed easier control of the proximal humeral osteotomy fragment, in such a way as to obtain the exact amount of correction that was planned preoperatively. Moreover, the healing and rehabilitation period of valgization osteotomy was overlapped with that of the humeral lengthening, thus keeping the treatment period to a minimum. After 10 cm lengthening of the humerus, and valgization-internal rotation-forward flexion osteotomy of the proximal humerus, the shoulder joint range of motion improved by 50-600% and the patient felt a subjective improvement of the function, which sustained during the 4 yr of follow-up.
Finally, it is interesting to note the exceptionally rapid healing of the distraction gap that occurred in the process of humeral lengthening in this case. The healing index of humeral lengthening by distraction osteogenesis is reportedly around 1 month/cm according to several authors (13-16) while it was 0.55 month/cm in this case. Relatively young age at the time of surgery might have contributed to rapid new bone formation, but there is a possibility that unresponsiveness to PTH action also be beneficial to intramembranous ossification by distraction osteogenesis. At least, distraction osteogenesis may be considered a safe surgical option for PHP patient with AHO.
Figures and Tables
 | Fig. 1Preoperative photograph and radiographs. (A) The right humerus is 5 cm shorter than the contralateral side at the age of 8 yr and 10 months. (B) Humerus varus deformity is observed on the right side. (C) All the metacarpals and phalanges are short and thick. (D) Brachymetatarsia of the 3rd, 4th and 5th resulting from premature physeal closure is observed. |
References
1. Gill TJ, Waters P. Valgus osteotomy of the humeral neck: a technique for the treatment of humerus varus. J Shoulder Elbow Surg. 1997. 6:306–310.

2. Ellefsen BK, Frierson MA, Raney EM, Ogden JA. Humerus varus: a complication of neonatal, infantile, and childhood injury and infection. J Pediatr Orthop. 1994. 14:479–486.

4. Taybi H. Taybi H, Lachman RS, editors. Metabolic disorders. Radiology of syndromes, metabolic disorders, and skeletal dysplasias. 1996. 4th ed. St. Louis: Mosby;706–708.
5. Levine MA, Downs RW Jr, Moses AM, Breslau NA, Marx SJ, Lasker RD, Rizzoli RE, Aurbach GD, Spiegel AM. Resistance to multiple hormones in patients with pseudohypoparathyroidism: association with deficient activity of guanine nucleotide regulatory protein. Am J Med. 1983. 74:545–556.
6. Okada K, Iida K, Sakusabe N, Saitoh H, Abe E, Sato K. Pseudohypoparathyroidism-associated spinal stenosis. Spine. 1994. 19:1186–1189.

7. Miric A, Vechio JD, Levine MA. Heterogeneous mutations in the gene encoding the alpha subunit of the stimulatory G protein of adenylyl cyclase in Albright hereditary osteodystrophy. J Clin Endocrinol Metab. 1993. 76:1560–1568.
8. Patten JL, Johns DR, Valle D, Eil C, Gruppuso PA, Steele G, Smallwood PM, Levine MA. Mutation in the gene encoding the stimulatory G protein of adenylate cyclase in Albright's hereditary osteodystrophy. N Engl J Med. 1990. 322:1412–1419.

9. Levine MA. Pseudohypoparathyroidism. from bedside to bench and back. J Bone Miner Res. 1999. 14:1255–1260.

10. Chung UI, Lanske B, Lee K, Kronenberg H. The parathyroid hormone/parathyroid hormone-related protein receptor coordinates endochondral bone development by directly controlling chondrocyte differentiation. Proc Natl Acad Sci USA. 1998. 95:13030–13035.
11. Solonen KA, Vastamaki M. Osteotomy of the neck of the humerus for traumatic varus deformity. Acta Orthop Scand. 1985. 56:79–80.

12. Verstreken L, Lamoureux J. Idiopathic humerus varus treated by osteotomy and progressive lengthening. A case report. Acta Orthop Belg. 1986. 52:86–92.
13. Aldegheri R, Dall'Oca C. Limb lengthening in short stature patients. J Pediatr Orthop B. 2001. 10:238–247.

14. Kashiwagi N, Suzuki S, Seto Y, Futami T. Bilateral humeral lengthening in achondroplasia. Clin Orthop. 2001. 391:251–257.

15. Yang CB, Huang SC. Humeral lengthening using the Ilizarov technique. J Formos Med Assoc. 1997. 96:291–294.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download