Abstract
The objectives of this study were to assess the ultrasonographic (US) findings in patients with knee osteoarthritis (OA) with pes anserinus tendinitis or bursitis (PATB) syndrome and to determine the correlation between the US findings and the response to local corticosteroid injection. We prospectively studied 26 patients with knee OA with clinically diagnosed PATB syndrome. A linear array 7 MHz transducer was used for US examination of the knee. Seventeen patients were injected locally with tramcinolone acetonide in the anserine bursa area. Response to local corticosteroid injection was evaluated by pain visual analog scale (VAS), Western Ontario and MacMaster (WOMAC) osteoarthritis index and Global patient/physician assessment using Likert scale. On US examination, only 2 patients (8.7%) showed evidence of PATB. Pain VAS, WOMAC pain index and WOMAC physical function index improved significantly after corticosteroid injection. Global patient assessment revealed that 2 patients showed best response, 6 good, 1 fair, 8 the same, and none worse. It is of note that the 2 patients who showed the best response were those who showed US evidence of PATB. This finding shows that US can serve as a useful diagnostic tool for guiding treatment in PATB syndrome of OA patients.
Pain in the region of the pes anserinus (PA) insertion is a common rheumatologic condition diagnosed as pes anserinus tendinitis or bursitis (PATB) syndrome. Its diagnosis is entirely based on clinical manifestations, which is marked by spontaneous medial knee pain on climbing or descending stairs, tenderness at the PA insertion, and occasionally local swelling (1). The anserine bursa lies underneath the PA, the name given to the conjoined tendon of the sartorius, gracilis, and semitendinosus muscle at its insertion into the upper medial aspect of tibia, about 5 centimeters distal to the medial aspect of the knee joint (2). PATB syndrome is frequently associated with osteoarthritis (OA) and vice versa. In a previous report, anserine bursitis was clinically diagnosed in 29 (46.8%) among 62 Korean patients with knee OA (3). In contrast, 20 (83.3%) among 24 PATB patients were reported to have radiographic evidence of knee OA (4). As a result, it has been taken for granted that "Pain of OA could have a cause due to periarticular problems, such as anserine bursitis" (5). In addition, PATB syndrome is also associated with obesity or type II diabetes mellitus (DM) (2, 6).
Ultrasonographic (US) evaluation is useful for diagnosing a variety of regional pain syndrome and soft tissue rheumatism and has been increasingly employed in the rheumatologic practice. The objectives of this study were to assess the US findings in patients with knee OA with PATB syndrome and to determine the correlation between the US findings and the response to local corticosteroid injection.
We prospectively studied 26 patients with knee OA diagnosed at a University affiliated rheumatology clinic (all women, mean age 63.4 yr, range 53-77). Sex, age, height, weight, body mass index, and radiographic knee osteoarthritis graded I-IV according to Kellgren and Lawrence (7) were recorded.
PATB syndrome was clinically diagnosed, as described previously with minor modification (6). Briefly, each patient completed a questionnaire regarding knee pain as follows: 1) Have you had knee pain in the last 2 weeks? 2) Does your knee hurt when ascending or descending stairs? 3) Does your knee hurt when performing weight bearing activity? 4) Do you have trouble getting out of a car? All of the patients underwent a complete history and examination, including deep palpation of the anserine bursa at the same location over the medial aspect of the tibia below the knee joint. PATB syndrome was diagnosed if the patient responded positively to the questionnaire 1) and one of 2), 3), or 4) and tenderness was elicited on examination of anserine area.
Patients with the clinical diagnosis of PATB syndrome were enrolled into the US study. For the purpose of comparison between symptomatic and asymptomatic side, patients who complained of tenderness in only one anserine area were included. A linear array 7 MHz transducer (HDI 5000, ATL ultrasound, Bothell, WA, U.S.A.) was used. US examination of the knee and PA was performed as previously reported with minor modification by a radiologist trained in musculoskeletal US (8). The PA was located 2.5-3 cm distal to the medial joint line with the transducer placed longitudinally. The following US examinations were performed: measurement of the thickness of the PA (mean of 3 measures); morphologic intratendinous PA tissue characteristics; presence of anserine tendinitis (both thickening and loss of normal fibrillar echotexture); presence of bursitis (circumscribed anechoic fluid collection of 2 mm or greater).
Seventeen patients were injected locally with triamcinolone acetonide in the anserine bursa area. A mixture of 40 mg triamcinolone acetonide and 1 mL of 2% lidocaine was infiltrated at the point of maximal tenderness in the anserine bursa area. Response to local corticosteroid injection was evaluated by pain visual analog scale (VAS) related to the knee and Global patient/physician assessment using Likert scale 2 weeks after corticosteroid injection (0=best response, complete relief of pain, 1=good response, pain decreased markedly, but pain remains, 2=fair, pain decreased slightly, 3=the same, pain was the same as that before the treatment, 4=worse, pain was worse than that before the treatment). Culturally adapted and validated Korean version of Western Ontario and MacMaster (WOMAC) osteoarthritis index was also used (9).
Data are presented as mean±S.D. for continuous variables and as frequency (%) for categorical variables. A p-value was calculated by Student's t-test for continuous variables or by chi-square test for categorical variables. A p value of p<0.05 was considered statistically significant and all the statistical analyses were performed using SPSS for Windows (Version 10.0, Chicago, IL, U.S.A.).
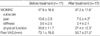
Table 1 shows baseline demographic characteristics of the subjects.
On US examination, only 2 patients (7.7%) showed US evidence of PATB. In one patient, marked thickening and loss of normal fibrillar echotexture of symptomatic side compared to asymptomatic side was observed (Fig. 1). In the other patient, anechoic fluid collection in the symptomatic anserine bursa area was noted (Fig. 2). Positive US finding of PATB did not correlate with age, duration of osteoarthritis, body mass index or radiographic grading of OA. The thickness of PA tendon was significantly greater in symptomatic side compared to asymptomatic side, but when the 2 patients with US evidence of PATB were excluded, the difference was not statistically significant (Table 2). Other US findings in these patients included the following : suprapatellar pouch effusion 22 (84.6%), degenerative spur change 16 (61.5%), popliteal cyst 4 (15.4%), infrapatellar bursitis 1 (3.8%). Superficial patellar bursitis was not found in any of our patients.
Local corticosteroid was injected in 17 patients. The demographic and clinical characteristics of these 17 patients were not different from those of 9 patients who were not injected with corticosteroids except that those who were injected were older than those who were not injected (Table 1). Pain VAS significantly decreased from 73.1 mm before corticosteroid injection to 50.7 mm after injection (p=0.0004, Table 3). WOMAC pain index and WOMAC physical function index also improved significantly after corticosteroid injection (10.6 and 33.8 before corticosteroid injection and 7.5 and 27.4 after injection, p=0.007 and 0.006, respectively). Global patient assessment using Likert scale revealed that 2 patients showed best response, 6 good, 1 fair, 8 the same, and none worse (Table 4). Global physician assessment revealed that 2 patients showed best response, 4 good, 5 fair, 1 the same, and 5 worse. It is of note that the 2 patients who showed the best response were those who showed US evidence of PATB. It is also of note that after the corticosteroid injection, tenderness on deep anserine palpation disappeared in only 5 patients (29%) including the 2 patients that showed US evidence of PATB.
Currently, it is a common practice to diagnose soft tissue rheumatic problem clinically and to treat it empirically, sometimes using local corticosteroid injections. Many of these soft tissue rheumatic problems, however, are elusive to diagnose by imaging modalities or pathological examination. Previous reports on radiographic finding of PATB are rare. In a report by Hall and Joffe (10), computed tomography (CT) imaging revealed a sharply defined low-attenuation cyst lying immediately beneath the pes anserinus tendon in a patient with non-tender mass on the anteromedial aspect of the leg below knee. The mass was not enhanced after injection of intravenous contrast material. Notably, the authors pointed out that distension of the anserine bursa is not synonymous with the clinical syndrome of anserine bursitis, because the case patient did not have any symptoms pertaining to the knee, and that the clinical syndrome of anserine bursitis actually may be a tendinitis or a fascitis involving the insertions of the pes anserinus tendon. In another report, anserine bursa was visualized both by ultrasonography and CT (11). In accordance with our result, ultrasonography demonstrated a cystic mass located on the anteromedial surface of the proximal tibia. CT guided aspiration of bursa was perfomed along with intrabursal injection of methylprednisolone, which led to resolution of symptoms. Few studies systematically elucidate the morphological characteristics of the PA insertion and bursa in clinically diagnosed PATB syndrome by imaging modalities. Because US examination is an excellent and a widely used technique for imaging superficial soft tissues, it can be routinely used as a diagnostic tool to improve the assessment of joints and soft tissues. One study examined US features of the PA and subcutaneous medial knee fat in patients with clinically diagnosed PATB syndrome (8). Of 37 patients, anserine bursitis was diagnosed in only 3 knees and PA tendinitis in 1. Another study which systemically assessed the musculoskeletal US findings in patients with type 2 diabetes mellitus (DM) showed that 28.6% of clinical PATB syndrome had PA tendinitis findings (12). In line with these reports, our study showed that only a minority of clinically diagnosed PATB syndrome patients had US evidence of PATB. This discrepancy between clinical and US findings could be explained in 3 different ways. First, US examination may not delineate the PA tendon abnormalities involved in the PATB syndrome. In this regard, a corroboration with magnetic resonance imaging (MRI) would be intriguing. However, because tissues with few mobile protons emit little or no signal and therefore the internal architecture of the tendon may not be well demonstrated by MRI, this limitation in visualization of tendon abnormality may also happen with MRI. Second, the tenderness elicited by deep palpation of anserine area may not stem from PA tendon or anserine bursa, but from other structures not adequately visualized by US. In our patients, the most common US finding was suprapatellar effusion followed by degenerative spur change, all of which are primary findings of underlying knee OA. Small numbers of patients had popliteal cyst, and infrapatellar bursitis, but these lesions are not likely to be responsible for the tenderness around the anserine area in the majority of our patients. Third, the point of tenderness by deep palpation may be another tender point with unusually low threshold for perception of tenderness. For instance, about 30% of normal controls elicited tenderness on deep palpation of anserine area (unpublished observation).
There are a paucity of data regarding the effectiveness of local corticosteroid injection in patients with PATB syndrome. In a report by Larsson and Baum (13), there was a significantly better result when steroids were used compared to when lidocaine alone was used 1 month after the injections. Seventy-one percent of patients injected had improved significantly after a follow up of 2-61 months. However, another report revealed that only 24% of patients showed good response and among these only a third experienced total relief of pain (14). This discrepancy probably results from the differences in methodology, such as retrospective or prospective design, or the definition of response.
Although pain VAS and WOMAC index improved significantly in our patients after injection, less than half of patients responded that they had more than good response and only 11.8% reported complete relief of their discomfort. Because all of our patients had knee OA, relief of symptoms of PATB alone may not be sufficient for alleviation of knee discomfort. In addition, WOMAC scale has not been validated for the assessment of symptom change in PATB syndrome previously. Despite this limitation, it is of note that only those patients who had US evidence of PATB showed complete relief of discomfort after corticosteroid injection.
In conclusion, among knee OA patients with clinically diagnosed PATB syndrome, only a minority had US findings indicative of PATB. Local corticosteroid injection resulted in complete relief of pain only in those patients with US findings of PATB. Recently, evidence that US exam can serve as a useful tool to determine the usage of non-steroidal anti-inflammatory drug versus acetaminophen in knee OA has been suggested (15). Also for optimal management of soft tissue problems in knee OA, assessment by imaging modalities such as US examination is useful.
Figures and Tables
Fig. 1
Ultrasonographic finding of tendinitis in the pes anserinus. Marked thickening of symptomatic side compared to asymptomatic side is observed along with loss of normal fibrillar echotexture.

Fig. 2
Ultrasonographic finding of anserine bursitis. Anechoic fluid collection measuring 13 mm in maximal diameter is noted.
ACKNOWLEDGEMENT
This study was supported by a grant from the Hallym University Medical Center (01-2004-09).
References
1. Biundo JJ. Schumacher HR, editor. Regional rheumatic pain syndromes. Primer on the rheumatic diseases. 1997. 11th ed. Atlanta (GI): Arthritis Foundation;144.
3. Kang I, Han SW. Anserine bursitis in patients with osteoarthritis of the knee. South Med J. 2000. 93:207–209.

4. Brookler MI, Mongan ES. Anserine bursitis, a treatable cause of knee pain in patients with degenerative arthritis. California Medicine. 1973. 119:8–10.
5. Dieppe PA, Buckwalter JA. Klippel JH, Dieppe PA, editors. Management of limb joint osteoarthritis. Rheumatology. 1998. 2nd ed. London, U.K.: Mosby;8.9.1.
6. Cohen SE, Mahul O, Meir R, Rubinow A. Anserine bursitis and non-insulin dependent diabetes mellitus. J Rheumatol. 1997. 24:2162–2165.
7. Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957. 16:494–502.

8. Uson J, Aguado P, Bernad M, Mayordomo L, Naredo E, Balsa A, Martin-Mola E. Pes anserinus tendino-bursitis: what are we talking about? Scand J Rheumatol. 2000. 29:184–186.
9. Bae SC, Lee HS, Yun HR, Kim TH, Yoo DH, Kim SY. Cross-cultural adaptation and validation of Korean Western Ontario and McMaster Universities (WOMAC) and Lequesne osteoarthritis indices for clinical research. Osteoarthritis Cartilage. 2001. 9:746–750.

11. Voorneveld C, Arenson AM, Fam AG. Anserine bursal distension: diagnosis by ultrasonography and computed tomography. Arthritis Rheum. 1989. 32:1335–1338.
12. Unlu Z, Ozmen B, Tarhan S, Boyvoda S, Goktan C. Ultrasonographic evaluation of pes anserinus tendino-bursitis in patients with type 2 diabetes mellitus. J Rheumatol. 2003. 30:352–354.
13. Larsson L, Baum J. The syndrome of anserine bursitis: an overlooked diagnosis. Arthritis Rheum. 1985. 28:1062–1065.
14. Abeles M. Anserine bursitis. Arthritis Rheum. 1986. 29:812–813.
15. Do JH, Hur SE, Paek SI, Nah JM, Kim CH, Lee SH, Park SH, Cho CS, Kim HY, Kim WU. Comparison of clinical efficacy between nonsteroidal anti-inflammatory drugs and acetaminophen in knee osteoarthritis according to ultrasonographic findings. J Korean Rheum Assoc. 2004. 11:14–24.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download