Abstract
It is surprising that about 24% of patients with benign osteoporotic vertebral fracture die within a year from respiratory infection and urinary tract infection because of coughing and voiding difficulties, depending on the sites of compression fractures. We reviewed 500 patients on whom percutaneous vertebroplasty (PVP) was performed, at 612 levels in terms of patient selection, operation technique, medication, and clinical outcomes during the follow-up course for 2 yr study period. To confirm the most painful level among the multiple fracture sites, physical examination after facet joint block under the fluoroscope was the most reliable method. The mean total lumbar spine fracture threshold of bone mineral density was 0.81±0.05 g/cm2. The mean changes of numeric rating scale scores, Oswestry Disability Index except sex life, and Karnofsky performance status were -72.00, -83.50 and +60.62% in the osteoporosis group and -51.89, -45.02, and 69.03% in the tumor group. Complications related to the procedure were lateral spinal cord damage, transient paresthesia and transient hypotension. PVP with facet joint block is a profitable method for the vertebral compression fracture because of low risk and short duration of procedure with a high chance to result in pain relief and early mobilization.
An increasing number of patients are suffering from vertebral compression and destructive lesions from osteoporosis and cancer in the aging society. Although the optimum time for the procedure is controversial, percutaneous vertebroplasty (PVP) or kyphoplasty is a the key technique to reduce life-threatening pneumonia, urinary tract infection and other complications from prolonged bed rest and unrelieved back and radiating flank, abdomen and groin pain (1). PVP with or without uni- or bi-lateral facet joint blocks gives the patient immediate pain relief and it also allows fast recovery of ambulation.
Excluding 30 cases of operations by bipedicular approaches, we reviewed 500 patients who had undergone PVP at 612 vertebral levels in terms of the criteria of patient selection, operation technique, clinical outcomes and the follow-up course including medication and the medial branch lesioning of the posterior ramus.
This study was approved by the Ethics Committee for Human Study of Pusan National University Hospital, and informed consent was obtained from each patient. After excluding 30 cases of operations by bilateral pedicular approach without the concept of radicular pain due to facet joint loading, a total of 500 patients suftering from vertebral compression and destructive fractures from osteoporosis and cancer had PVP with or without facet joint blocks for two years.
We analyzed the period of pain, numeric rating scale (NRS) scores for pain, Oswestry Disability Index (ODI) except the data about sex life, and Karnofsky performance status (KPS) before and after the procedure.
Neurologic examinations were performed to rule out other disorders. Supraspinous tenderness was marked with a paper clip for vertebroplasty, and adjacent facet joint tenderness was pointed with a marking pencil for facet joint block in prone position. CT or MRI and radioactive bone scan were done. For the performance of the unipedicular approach, we measured the angle and distance from the midline on the skin from the CT or MRI.
Basic laboratory tests for preoperative workup and for postoperative follow-up included coagulation tests, liver and renal function tests, and bone mineral density (BMD).
On operation, we performed uni- or bilateral facet joint blocks before PVP according to the complaint of patients, usually neighboring the lesion of the vertebrae.
Lidocaine (1%) was infiltrated from the skin to periosteum near the pedicle under the fluoroscopic guidance. We performed epidural analgesia before or during the procedure around the level of stable vertebral fractures in some patients who could not maintain a prone position. And we injected 30 mg ketorolac and 50 µg of fentanyl intravenously. In some patients who complained of severe anxiety about the procedure, we gave 2-3 mg of midazolam intramuscularly before the procedure or intravenously during the procedure.
Under the fluoroscope, the entry point of local anesthetic needle and 11 gauge out-diameter 10 cm length vertebroplasty needle (J-type Bone Marrow Needle®, Manan Medical Product, Wheeling, IL, U.S.A.) became the meeting point of trajectory line from the pedicle to the body in the lateral view and sagittal line away from the midline in the antero-posterior (AP) view. The distance from the midline to sagittal line was determined by CT or MRI.
From the AP view, the target point was the upper lateral part of the pedicle. A small incision was made with No. 15 scalpel. Under the lateral view of fluoroscope, a vertebral needle was advanced carefully through the pedicle by manual turning and pressing of a handle without a hammer. The final reaching point would be anterior 1/4 to 1/3 on the lateral view and midline of the vertebral body on the AP view. Under continuous monitoring using the fluoroscope, the contrast medium was injected through the vertebral needle and any evidence of leakage of contrast media to intravenous and epidural space was checked. After testing of the filling into the body and leakage into the intravenous and epidural space of contrast media, antibiotics-containing polymethyl methacrylate (PMMA) cement was injected by using an injector. The whole injection procedure was monitored with a continuous fluoroscopy to avoid possible leakage. The skin was closed by skin closure (Steri-Strip®, 3M, St. Paul, MN, U.S.A.) and piroxicam patch (Trast Patch®, SK Pharma., Seoul, Korea).
For 2 hr after the procedure, hypotension, dyspnea, and sensory or motor problems were checked in the recovery room, and we asked patients to walk with help, and when possible the patient was discharged.
The patients were followed-up at 1 week, 1, 2, 3, 6, 9, and 12 months after the procedure. We measured the BMD of lumbar spine and femur every 3 months.
After the procedure, the major analgesics for the pain control were changed from codeine-paracetamol-ibuprofen mixture (Myprodol®, Adcock Ingram Pharmaceuticals, Johannesburg, South Africa) to tramadol-acetaminophen mixture (Ultracet®, Janssen Korea, Whasung, Korea) for 1 week, and then we usually stopped the analgesic administration. Medication for osteoporosis was 70 mg of alendronate sodium (Fosamax®, Merck Sharp & Dohne, de Mexido, S. A de C.V, Mexico) weekly with or without 60 mg of raloxifene HCl (Evista®, Eli Lily & Co, Hamsphire, U.K.) daily. BMD was measured by dual energy radiography absorptiometry (DEXA, Lunar PRODIGY, GE System, Madison, WI, U.S.A.) at 3-month intervals.
After facet joint blocks, we evaluated the period of relapse of symptoms and the need for denervation of medial branch of posterior ramus.
Unless indicated otherwise, the data were presented as mean±SD. The data were analyzed by using Wilcoxon signed rank test of nonparametric test for therapeutic effects including NRS, ODI, and KPS before and after PVP with facet joint block between the osteoporosis and tumor groups and for the comparison of combination effects of alendronate and raloxifene in osteoporosis.
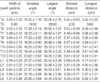
In 500 patients, PVP was performed on 612 vertebral levels with or without facet joint blocks during the 2-yr study period. The demographic data of the patients are shown in Table 1.
Before the procedure, 10 patients suffered from pneumonia, 7 patients complained of voiding difficulties, and 4 patients had mild dementia due to posttraumatic organic disorder after the osteoporotic vertebral compression fractures.
After conservative treatment with corset and medication for 2 weeks, 96.2% (500/520) of patients wanted to receive PVP because of insufficient pain control.
Eighty eight percent of patients (440/500) who complained of radicular pain to the flank, abdomen, or the buttock, received uni- or bilateral facet joint block around the fractured vertebrae before PVP. In 30 cases of patients by bilateral pedicular approach without the concept of the radicular pain due to facet joint loading, the mean reduction of ODI except sex life, NRS scores for pain and KPS were 56.1±8.8%, 3.5±1.2, and 42.2±12.6, compared with 82.2±11.2%, 5.4±1.3 and 52.3±14.5 in subsequent 500 cases of patients with who had simultaneous facet joint block.
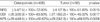
The distribution of vertebral levels of operations and pedicle width, angle and distance from the midline on the skin from the CT or MRI targeting to the anterior 1/3 to 1/4 for PVP with unipedicular approach are shown in Table 2 and Table 3. It was possible to perform unipedicular approach from T4 to L5 level. During the procedure, 74.3% (455/612) levels showed epidural and/or vascular leakage of contrast media under the fluoroscopy.
The mean changes of NRS scores for pain, ODI except sex life, and KPS were -72.00, -83.50 and +60.62% in the osteoporosis group and -51.89, -45.02, and +69.03% in the tumor group (Table 4).
As for the diagnostic tools to pinpoint the painful levels among the multiple fractures, plane radiography film, CT or MRI, and bone scan showed discrepant results. To confirm the most painful level among the multiple fracture sites and to get the clinical success to relieve pain, physical examination after facet joint block under the fluoroscope was the most reliable method.
During the follow-up course, 60% (264/440) of the patients who received facet joint block complained of recurring radicular pain in 3.5±1.2 months (range, 1.8 to 11.2 months). Among them, 50% (132/264) received conventional radiofrequency ablation.
Complications related to the procedure were 1 case of lateral spinal cord syndrome on L1, 3 cases of transient paresthesia for 1 week, and 1 case of severe hypotension (70/40 mmHg) with bradycardia related to anterior leakage to the sympathetic nerves, which was immediately recovered by ephedrine.
The mean changes of lumbar spine and femoral neck BMD after 3 and 6 months of treatment with alendronate (ALN) with or without raloxifene (RLX) in the osteoporotic group were shown in Table 5.
With regard to conservative treatment which includes bed rest, analgesic medication, and orthotics, conservative therapy takes a long time and can cause difficult problems. Uncontrolled continuous pain can cause difficulties in coughing and mobilization, which finally leads to respiratory and urinary tract infection and eventual possible dementia. trauma toward dementia. We should consider spinal fracture as a major trauma in one's life. Therefore, we tried to reduce hospital stay much as possible to minimize patients' maladaptation from life-style including space (home to hospital), caring person (family to nursing personnel), and time (including sleeping and feeding).
For multiple osteoporotic or metastatic fractures, it was to decide the order of PVP procedure. Gaughen et al. (2) took the evidence of edema on MRI or increased uptake on bone scan rather than preoperative spinous process tenderness as affecting the clinical success of PVP. In our experience, the level of PVP in multiple spine fractures was not radiography film, active lesions on the bone scan, or MRI. Checking the thoracic or lumbar plain series with paper clip markings on the back had a gap because maximal tenderness point on physical examination in prone position was different from that of the films in erect position. There were usually intractable spinous tenderness below two or three levels from the levels on plain films. Despite multiple levels of active lesions on bone scan and edema on MR, the range of intractable painful sites requiring vertebroplasties were smaller.
Facet joint block before PVP had two major roles, one was to let patients lie down during the procedure under the local anesthesia and the other was to let the operator find out the exact level among the multiple fractures by elimination of radiating pain to the flank, abdomen, groin or buttock. It should be reminded that performing PVP over the three levels simultaneously will increase the risk of asymptomatic leakage of cement, and most of patients cannot endure the prone position during the procedure.
In 88% (440/500) of patients who complained of radicular pain to the flank, abdomen, or buttock, uni- or bilateral facet joint block around the fractured vertebrae was essential prior to PVP because the injected bone cement obscured the adjacent facet joints, and radicular pain would be decreased to a tolerable level during PVP. Our choice to select the correct level among the multiple fractures was spinous process tenderness under the fluoroscope by the aid of facet joint block before PVP for the best clinical outcomes.
Leakage of cement into the intravenous and epidural space would be a threatening condition. To reduce the risk and operating time, first of all, continuous monitoring of filling and leakage of contrast media and cement under the fluoroscopic guidance is most important, even though the risk of radiation hazard is increased. Second, if only leakage of contrast media occurs without the evidence of filling into the body, inserting 2-3 slices of absorbable gelatin sponge (Spongostan®, Johnson & Johnson Medical Limited, Gargrave, Skipton, U.K.) through the vertebral needle is helpful to reduce the chance of leakage into the venous and epidural space. Epidural and/or vascular leakages of contrast media occurred on 455/612 levels (74.3%). After filling with gelatin in the vertebroplasty needle, 2-3 mL of normal saline was injected and the appearance of filling and leakage of contrast media was observed again. At least, confirmation of filling the vertebral body first and subsequent small leakage into the venous and epidural space would be an acceptable condition to inject cement. Third, it is better to push the needle in rather than pull back when the needle contacted with vessels and filled with blood in aspiration despite the insertion of absorbable gelatin sponge. Fourth, abandon to inject more volume of cement for the intensity of the body of the vertebra. The introduction of 20% bone cement by volume results in a significant increase in the compressive strength of intact lumbar vertebrae; however, upper thoracic vertebrae do not demonstrate a similar improvement in strength. There was no difference in the stiffness of the vertebrae injected with cement regardless of location. Cement leakage was frequently noted with 20% cement injection, especially in the specimens with higher BMD. The location of the cement did not appear to have an effect on the loading behavior of the bone but should be controlled to minimize the chance of cement escaping into the spinal canal (3). From to this article and our experience, in the metastatic compression fractures with higher BMD, the increase of the temperature and resultant ablation of the nerve endings of the sinovertebral and sympathetic nerves around the body could be the important mechanisms to reduce pain than the strength improvement due to a volume increase. After the diagnosis of bone metastasis, the median survivals were 12 months in patients with breast carcinoma, 6 months in patients with prostate carcinoma, and 3 months in patients with lung carcinoma (4). According to other reports, the median survival rate was 48 months when metastases were confined to the skeletal system in patients with breast carcinoma, but it decreased to only 9 months if visceral metastases were also present (5). Finally, barium sulfate mixed with the cement would be helpful for observing the appearance of filling the body despite unknown foreign body reaction and somewhat reduced degree of strength augmentation.
During the follow-up course, 60% (264/440) of the patients who received facet joint block complained of recurring radicular pain in 3.5±1.2 months (range, 1.8 to 11.2 months). Among them, 50% (132/264) received conventional radiofrequency ablation, 90℃ for 90 sec with 10 mm active tip and 10 cm long, on the medial branches of the posterior ramus. The patients who received radiofrequency ablation did not experience recurrence of the symptom or neuropathic pain related the neural ablation within 6 months. Further long-term follow-up study is necessary.
For past several years, a patient who could not lie in prone position during the procedure was not considered a good candidate for PVP. However, we kept a continuous epidural catheter and reduced pain with local anesthetics before the procedure after checking MRI and CT films and then removed it after the procedure. Intractable pain and inability to take a suitable position during PVP procedure are not contraindications any more.
The entry point of the needle should be the upper lateral part of the pedicle on the AP view of fluoroscope to reduce the risk of nerve root damage below the pedicle and cord damage medial to the pedicle. If a needle with single bevel shaped stylet (6) is used for PVP, it is important to turn the direction of bevel upward or downward, which will determine the final end point of the needle.
Before the injection of cement, a small amount of local anesthetics, 1 mL of 1% lidocaine, reduced the pain associated with volume expansion without complications. For an esthetic view and wound care, a small transverse incision along the crease of the back for introducing the vertebral needle with #15 scalps was better than bruising with a dull 11-gauge needle without incision. And after finishing the procedure, skin closure without suture and piroxicam patch for 2 days' analgesia were applied on the wound. There was no skin wound infection or osteomyelitis despite no more dressing on the wound and no antibiotic medication. Most of patients could take a shower one week after their first visit to the outpatient department.
Preoperative medications were a codeine-containing mixture including acetaminophen and ibuprofen, muscle relaxants, and alendronate with or without raloxifene according to their economic status and contraindications. After the procedure, the major analgesic medication was changed into tramadol-acetaminophen mixture. Patients who complained of radicular pain related to facet joint syndrome were prescribed gabapentin and/or amitriptyline or nortrityline before and after the facet joint blockade.
Complications related to the procedure were 1 case of lateral spinal cord syndrome on L1 that occurred while trying to aim the vertebral needle to the midline of the body on the unipedicular approach, 3 cases of transient paresthesia for 1 week, and 1 case of severe hypotension (70/40 mmHg) with bradycardia related to anterior leakage to the sympathetic nerves, which was immediately recovered by ephedrine. According to the Society of Interventional Radiology (SIR) Quality Improvement Guidelines for PVP using SIR Standards of Practice Committee Classification of Complications of by Outcome, there were 1 case in the class D of major complications (Require major therapy, unplanned increase in level of care, prolonged hospitalization over 48 hr) and 3 cases in the class B of minor complications (Normal therapy, no consequence, includes overnight admission for observation only) (7).
As for the mechanism of pain relief in PVP, the sensory role of nerve endings within compact bone has become the focus for two reasons. First, increasing the rigidity of the bone through the injection and subsequent hardening of PMMA cement is expected to reduce bone deformation during weight bearing, and hence to reduce the mechanical forces applied to nociceptive endings within the bone. Second, since the cement itself is toxic for the nerve tissue, PVP causes at least partial denervation of the bone matrix (8). Facet joint pain radiating to the dermatome is a neuropathic pain of the medial branch of posterior ramus probably originating from the tightened narrow space between the superior and inferior articular processes.
A few patients showed mixed features of osteoporosis and tumor on the vertebrae. We tried to identify the nature of the disease-causing compression fracture by using bone marrow aspiration biopsy during PVP. There was no tumor cell on the aspirate smear and cell block among all the specimens. Non-specific acute and chronic inflammations were found in only three osteoporotic specimens. It was impossible to get tumor cells in the primary or secondary tumorous vertebral compression fracture by aspiration biopsy. Instead of using the aspiration biopsy, bone tissue punch biopsy by trephine needle would be helpful to prove the cause of vertebral compression fracture (9).
Some doctors believe that PVP causes new fractures adjacent to the initial level of PVP because diminishment of the compliance of one vertebra by means of cement injection may place the remainder of the axial skeleton at greater risk for collapse. However Kallmes and Jensen (6) reported that one-half of new fractures were occurring adjacent to the initial PVP level, but 68% of fractures in multiple osteoporotic fractures were at contiguous levels before the PVP. We do agree that there is no evidence of increasing risk of new fracture by preceding PVP. In our opinion, it is more important rather to improve the BMD score than to be concerned about the risk of subsequent fracture after PVP.
Similar to the results from a to previous study (10), combined treatment with alendronate and raloxifene resulted in greater increase of BMD than the single-agent group (11). If the combination regimen is not affordable, alendronate is our choice to increase by one standard deviation BMD and to reduce the risk of new fracture after PVP. Known predictive fracture risk decrease in BMD by one standard deviation at spine and hip were 2.3 and 2.6 respect 1.5 to all other sites (12, 13). Raloxifene was added to alendronate, except in male patients and patients with breast cancer (14).
Figures and Tables
Table 2
The distribution of 612 vertebral levels in 500 patients who underwent percutaneous vertebroplasty with joint block according to the patient group

Table 3
Pedicle width, angle and distance from the midline on the skin on CT or MRI targeting to the anterior midline 1/3 to 1/4 for PVP with unipedicular approach
References
1. Haczyński J, Jakimiuk A. Vertebral fractures: a hidden problem of osteoporosis. Med Sci Monit. 2001. 7:1108–1117.
2. Gaughen JR Jr, Jensen ME, Schweickert PA, Kaufmann TJ, Marx WF, Kallmes DF. Lack of preoperative spinous process tenderness does not affect clinical success of percutaneous vertebroplasty. J Vasc Interv Radiol. 2002. 13:1135–1138.

3. Higgins KB, Harten RD, Langrana NA, Reiter MF. Biomechanical effects of unipedicular vertebroplasty on intact vertebrae. Spine. 2003. 28:1540–1548.

4. Sherry MM, Greco FA, Johnson DH, Hainsworth JD. Breast cancer with skeletal metastases at initial diagnosis. Distinctive clinical characteristics and favorable prognosis. Cancer. 1986. 58:178–182.

5. Sherry MM, Greco FA, Johnson DH, Hainsworth JD. Metastatic breast cancer confined to the skeletal system. An indolent disease. Am J Med. 1986. 81:381–386.
7. McGraw JK, Cardella J, Barr JD, Mathis JM, Sanchez O, Schwartzberg MS, Swan TL, Sacks D. SIR Standards of Practice Committee. Society of Interventional Radiology quality improvement guidelines for percutaneous vertebroplasty. J Vasc Interv Radiol. 2003. 14:827–831.

8. Niv D, Gofeld M, Devor M. Causes of pain in degenerative bone and joint disease: a lesson from vertebroplasty. Pain. 2003. 105:387–392.

9. Minart D, Vallẽe JN, Cormier E, Chiras J. Percutaneous coaxial transpedicular biopsy of vertebral body lesions during vertebroplasty. Neuroradiology. 2001. 43:409–412.

10. Johnell O, Scheele WH, Lu Y, Reginster JY, Need AG, Seeman E. Additive effects of raloxifene and alendronate on bone density and biochemical markers of bone remodeling in postmenopausal women with osteoporosis. J Clin Endocrinol Metab. 2002. 87:985–992.

11. Kim KH, Lee HJ, Baik SW, Kim HK, Kwon JY, Kim CH. Comparison of bone mineral density of lumbar spine in osteoporotic patients treated with percutaneous vertebroplasty. Korean J Anesthesiol. 2004. 46:302–305.

12. Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996. 312:1254–1259.

13. Kim KH, Yoon JY. Measurement of bone mineral density of lumbar spine in osteoporotic patients treated with percutaneous vertebroplasty. Korean J Anesthesiol. 2003. 45:749–753.

14. Fabian CJ, Kimler BF. Chemoprevention of breast cancer: implications for postmenopausal women. Drugs Aging. 2002. 19:43–78.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download