Abstract
This study was undertaken to identify risk factors for postoperative voiding dysfunction and factors having impact on patient global satisfaction after a tension-free vaginal tape (TVT) procedure. Two hundred and eighty-five women who underwent the TVT procedure for stress urinary incontinence were analyzed to identify risk factors predictive of voiding dysfunction. Postoperative voiding dysfunction was defined as a peak urinary flow rate (PFR) <10 mL/sec (straining voiding, n=17) or residual urine volume >30% of bladder capacity (incomplete emptying, n=13). The global satisfaction rate was 91.6%. Voiding dysfunction developed in 29 (10.2%) patients. Among the factors, PFR was only factor of significance for voiding dysfunction. There was no significant difference between patients with and without voiding dysfunction in terms of their satisfaction. But postoperative PFR <10 mL/sec significantly compromised global satisfaction after the surgery. In those patients with a preoperative PFR <20 mL/sec, there were more patients with postoperative PFR <10 mL/sec. Peak urinary flow rate is an important factor for the postoperative voiding dysfunction. The inevitable decline in PFR can compromise patients' satisfaction with the procedure, when their postoperative PFR was <10 mL/sec.
Female stress urinary incontinence is an ancient problem. Following the "hammock hypothesis" by DeLancey, which describes the pathophysiology of female stress incontinence (1), the tension-free vaginal tape (TVT) procedure for treatment of stress urinary incontinence in women was introduced in 1996 (2). The TVT procedure is a minimally invasive surgical method for treating female urinary incontinence that has gained widespread popularity. The procedure requires positioning of a vaginal tape precisely underneath the mid-urethra with no tension, to restore urethral support.
With techniques used previously, most studies report a high cure rate and long-term durability (3). Surgeons who consider adopting the TVT procedure for their patients need to give attention not only to the efficacy of the procedure but also to the potential complications and untoward effects which may impact upon patient satisfaction and quality of life. Voiding dysfunction is a well recognized complication when using suburethral sling procedures (4, 5). It has been reported that subjective and objective voiding patterns could change after the TVT procedure (6). Voiding dysfunction has been estimated to occur at a rate of 1.5-20% after the TVT procedure (7, 8). Therefore, it is of interest to understand the reason why significant postoperative voiding dysfunctions follow the procedure and to determine whether those symptoms are predictable preoperatively. In this study, we evaluated comprehensive risk factors that may be predictive of postoperative voiding dysfunction, and factors having impact on patient satisfaction after the TVT procedure.
Between March 1999 and May 2002, 437 women with stress urinary incontinence underwent the TVT procedure in the urology department at our institution. We excluded 90 patients with a maximum follow up of less than six months and/or incomplete postoperative data and a further 62 patients without preoperative data to comprehensively analyze risk factors for postoperative voiding dysfunction. We retrospectively analyzed the remaining 285 patients by chart-reviews or telephone survey (by one person). The evaluation of surgical results including satisfaction, sense of urine loss, pad test, and others was performed six months after the surgery. Average age, mean symptom period, and mean parity were 51 yr, 6.9 yr, and 2.8 times, respectively. Preoperative symptom grade was I (loss of urine only with coughing, sneezing or lifting heavy objects) in 128 patients, II (loss of urine with minimal activity such as walking or arising from the sitting position) in 153 and III (totally incontinent while upright) in four patients (9). The study population included 10 patients who had previously undergone anti-incontinence surgeries, such as the Raz procedure, fascia lata sling, Burch colposuspension and anterior vaginal wall sling. Six patients had a history of vaginal hysterectomy and 45 patients underwent transabdominal hysterectomy in the past. The reasons for hysterectomy were uterine prolapse (n=2), cervical cancer (n=3), and abnormal uterine bleeding or uterine myoma (n=46). Concurrent hysterectomy, correction of cystocele, stone removal from the ureter or bladder, urethral caruncle excision and posterior vaginal repair were performed in seven, six, two, one and 20 patients, respectively. Most of the procedures (n=249) were performed under local and intravenous anesthesia (midazolam 1.5 mg and propofol 1.5 mg/kg) except for 36 women who needed general or spinal anesthesia for their concurrent procedures (Table 1).
Preoperative evaluation included medical history, physical examination, urinalysis, urine culture, a 3 days voiding diary, 1-hr pad test proposed by the International Continence Society (10), postvoid residual urine volume measurement, uroflowmetry, and urodynamic study including measurement of Valsalva leak point pressure (VLPP), maximal urethral closing pressure (MUCP), and pressure flow study.
All surgeries were performed by one urologist with even tension adjustment using long Mayo scissors as a spacer. The vaginal pack was removed 2 hr after the surgery. The bladder was emptied and catheter was not indwelled at the end of the procedure. If an adequate voiding was noted, determined as two consecutive voidings with a residual urine volume less than 100 mL, the patients were discharged within 24 hr. If a patient failed to void or if the bladder was injured during the procedure, a urethral catheter was placed and then removed the next day. For patients who failed to void or who were found to have a postvoid residual urine volume greater than 100 mL on two consecutive voidings, intermittent self-catheterization was recommended.
Voiding dysfunction was defined as having a peak flow rate less than 10 mL/sec (straining voiding) or a residual urine volume greater than 30% of the maximum cystometric capacity (poor emptying) on two or more readings (11). An ultrasound postvoid residual was measured.
Between patients with (n=29) and without (n=256) voiding dysfunction, multiple factors related to patient characteristics (age, parity, body mass index, history of hysterectomy or anti-incontinence surgery), symptoms and physical examination (symptom grade, 1-hr pad test, presence of concomitant urge incontinence, and cystocele), preoperative urodynamic study (peak urinary flow, volume of residual urine, MUCP, VLPP, maximal bladder capacity, maximal detrusor pressure, and detrusor pressure at peak flow rate), combined surgeries (simultaneous hysterectomy, anterior and posterior colporrhaphy, or correction of cystocele), and bladder perforation by a needle instrument were compared respectively. Uroflowmetry pattern had a normal configuration (uninterrupted) and bell-shaped form in most subjects and was therefore not analyzed. We determined the subjective and objective cure rate by a questionnaire and clinical examination, respectively. If patients had no urine loss after the procedure or social continence, a term coined in a previous report meaning that any perceived wetting by the patient was controlled by tissues or a small minipad, we considered them to be subjectively cured. We determined the objective cure rate by a 1-hr pad test and a stress test. Patients with pads containing less than 2 g of urine and a negative stress test were considered cured. Univariate analysis was performed to identify risk factors predictive of voiding dysfunction. All patients were requested to answer a global satisfaction question in one of four ways, such as "very satisfied", "satisfied", "so-so", and "dissatisfied", and an intention to recommend the surgery to others in two ways, such as "yes" or "no", at six months after their surgery. We correlated patients' satisfaction with postoperative voiding status and investigated which factor is related to the patients' global satisfaction. The chi-square test was used to compare percentage frequencies. Univariate analyses were performed using the Student's t-test, with p<0.05 considered statistically significant.
Mean operative time and the length of hospital stay were 28.4 min and 1.4 days, respectively. There was a significant decrease in peak flow rate by uroflowmetry preoperatively vs. postoperatively (30.1 vs. 23.5 mL/sec, p=0.0001) with a mean decline of 6.6 mL/sec. However, change in volume of residual urine was not significant (16.7 vs. 20.5 mL, p=0.271). Two hundred and sixty-one patients (91.6%) favored the procedure in answers to a global satisfaction questionnaire. There were 268 patients (94.0%) with an intention to recommend the surgery to others. Subjective and objective cure rates were 93.7% and 90.9%, respectively.
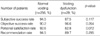
Voiding dysfunction developed in 29 (10.2%) of the 285 patients. Patient's peak flow rate only showed significant differences between the normal voiding group and voiding dysfunction group (preoperative peak urinary flow rate: 30.8 vs. 23.7 mL/sec, p=0.004, Table 2). When we generated an ROC curve for peak urinary flow rate, the area under the curve was 0.684; sensitivity and specificity were 22.3% and 55.2% at 20.9 mL/sec, and 33.6% and 34.5% at 23.9 mL/s, respectively (Fig. 1). When we compared the difference in patients' satisfaction rate between patients with preoperative peak flow rate lower and higher than 20 mL/sec according to this result, there was no statistical difference between them (data not shown). Also, there was no statistically significant difference between those with and without voiding dysfunction in terms of cure rates, patients' satisfaction and intention to recommend the surgery to others (Table 3). Postoperative peak urinary flow rate was less than 12 mL/sec in 23 patients, less than 10 mL/sec in 17 patients, and less than 8 mL/sec in six patients. The mean decline in peak urinary flow rate from their preoperative value was 13.4 mL/sec for patients with less than 12 mL/sec, 12.7 mL/sec for patients with less than 10 mL/sec, and 12.9 mL/sec for patients with less than 8 mL/sec. When we stratified all patients by these 3 postoperative peak flow rate values, significantly lower level of global satisfaction was noted from patients with a peak urinary flow rate less than 8-10 mL/sec, though the statistics were not significant for patients passing 12 mL/sec (Table 4). The mean preoperative peak urinary flow rates were 21.6 and 20.3 mL/sec in patients with less than 10 and 8 mL/sec postoperatively. In patients with a preoperative peak urinary flow rate less than 20 mL/sec, of less than 10 mL/sec than more than 20 mL/sec (Table 5).
The TVT procedure has rapidly become a widely performed operation in Korea. It offers advantages over conventional repairs: it is quick and can be done under local anesthesia. Though the procedure is well known as an effective approach with a high long-term cure rate, Boustead (12) indicated that 1.5-20% of patients can develop postoperative voiding dysfunction. The question is whether these postoperative voiding dysfunctions are predictable preoperatively, whether patients' satisfaction is related with voiding dysfunction, and whether there are pre- or postoperative risk factors predictive of patients' satisfaction. We previously reported that peak urinary flow rate is an independent prognostic factor for immediate postoperative urinary retention after the TVT procedure and its significant influence on patient satisfaction (13).
Prevalence and predictors of voiding dysfunction after various sling procedures have been identified but unfortunately vary among different institutions. The most likely reason for this difference is the lack of standard definitions of voiding dysfunction. For instance, Groutz et al. (14) defined it as a maximum flow rate less than 12 mL/sec, or residual urine volume greater than 100 mL. Stanton et al. (15) defined voiding difficulty as a peak flow rate less than 15 mL/sec (if at least 200 mL had been voided), or greater than 200 mL of residual urine on two or more readings. Lose et al. (9) defined impaired bladder emptying as a peak flow rate less than 15 mL/sec for patients younger than 60 yr and less than 10 mL/sec for patients 60 yr or older (at a voided volume greater than 150 mL). In terms of the TVT procedure, Wang et al. (16) defined normal voiding as a postvoid residual urine <100 mL, frequency of six of fewer voids per day and two or fewer per night, and a urinary stream considered normal by the patient.
The definition of voiding dysfunction in the current study is a peak urinary flow rate less than 10 mL/sec (voided volume greater than 100 mL) as straining voiding, or residual urine volume greater than 30% of the maximum bladder capacity as poor emptying on two or more readings. Based on our definition, 29 (10.2%) patients were included in the voiding dysfunction group. Among the clinical factors, preoperative peak flow rate only showed significant differences between the normal voiding and voiding dysfunction groups (Table 2). When we generated an ROC curve for peak urinary flow rate, the area under the curve was 0.684; sensitivity and specificity were 22.3% and 55.2% at 20.9 mL/sec, and 33.6% and 34.5% at 23.9 mL/sec, respectively (Fig. 1). This means peak urinary flow rate can effectively estimate the risk of voiding dysfunction and predict postoperative urinary retention. Anti-incontinence surgeries cannot avoid inducing some degree of obstruction to the lower urinary tract. The TVT procedure is not much different in this regard, although this procedure is completely tension free. Sander et al. (6) reported the peak urinary flow rate decreased from a preoperative 29.4 mL/sec to postoperative 24.5 mL/sec (p=0.036). There was a significant decrease in the peak urinary flow rate preoperatively versus postoperatively (30.1 mL/sec; 23.5 mL/sec, respectively, p<0.001) with an average decline of 6.6 mL/sec in our study. From our results, the risk of developing voiding dysfunction can be effectively stratified by the average decline in peak urinary flow rates. The intriguing point is that voiding dysfunction itself did not have a significant impact on patient satisfaction in most patients. This means most patients are still satisfied with gaining continence at the expense of a decrease in flow rate and a 6.6 mL/sec decline in peak urinary flow rate is modest enough to endure for most of the patients. Likewise, the preoperative peak flow rate predictive of voiding dysfunction, 20 mL/sec in the current study, could not effectively predict patients' satisfaction after the surgery. Furthermore, we could not find any relevance between patients' satisfaction and preor postoperative risk factors in patients with normal voiding and even in patients with voiding dysfunction. However, when we stratified all patients into subgroups according to specific postoperative peak flow rates, if a patient already had a low peak urinary flow rate that was not able to buffer the inevitable decline, or the decline in peak urinary flow rate was severe enough to be less than 10 mL/sec, global satisfaction with the procedure was significantly compromised. This result signifies patients' satisfaction depends much more on postoperative peak flow rate itself than on voiding dysfunction. Though we could not find any significant correlation between preoperative peak flow rate and patients'satisfaction in this study, the descent of peak flow rate was more significant in patients with less than 10 and 8 mL/sec postoperatively and preoperative peak flow rate was already lower in them (about 20 mL/sec) comparing to the mean preoperative peak flow in all patients (about 30 mL/sec). In this context, this ostensibly "tension-free" procedure may actually only be "tension-tolerable" in a sense. In any situation where the tension is intolerable, patients' satisfaction on the gaining of continence can be overcome by the disappointing urinary flow rate as shown in this study. Therefore, all efforts decreasing tension should be taken in applying vaginal tape and particular attention should be given to patients with already low preoperative peak flow rate in terms of placement of vaginal tape and preoperative warning of potential voiding risk after the procedure.
Peak flow rate is the most important factor in predicting postoperative voiding dysfunction. Patient satisfaction on the highly curative TVT procedure is not significantly influenced by postoperative voiding dysfunction based on the current definition. However, the inevitable decline in peak urinary flow rates may compromise patient satisfaction with the procedure when their postoperative flow rate is less than 10 mL/sec.
Figures and Tables
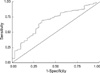 | Fig. 1ROC curve for peak flow rate. Area under curve was 0.684. Sensitivity and specificity were 22.3% and 55.2% at 20.9 mL/sec, respectively. This means peak urinary flow rate may estimate the risk of voiding dysfunction as effectively as it predicts postoperative urinary retention. |
References
1. DeLancey JO. Structural support of the urethra as it relates to stress urinary incontinence: the hammock hypothesis. Am J Obstet Gynecol. 1994. 170:1713–1720.

2. Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996. 7:81–85.

3. Ward KL, Hilton P, Browning J. A randomized trial of colposuspension and tension-free vaginal tape (TVT) for primary genuine stress incontinence. Neurourol Urodyn. 2000. 19:386–388.
4. Bidmead J, Cardozo L. Sling techniques in the treatment of genuine stress incontinence. BJOG. 2000. 107:147–156.

5. Leach GE, Dmochowski RR, Appell RA, Blaivas JG, Hadley HR, Luber KM, Mostwin JL, O'Donnell PD, Roehrborn CG. Female stress urinary incontinence clinical guidelines panel summary report on surgical management of female stress urinary incontinence. J Urol. 1997. 158:875–880.

6. Sander P, Moller LM, Rudnicki PM, Lose G. Does the tension-free vaginal tape procedure affect the voiding phase? Pressure-flow studies before and 1 year after surgery. BJU Int. 2002. 89:694–698.

7. Ulmsten U, Johnson P, Rezapour M. A three-year follow up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol. 1999. 106:345–350.

8. Olsson I, Kroon U. A three-year postoperative evaluation of tension-free vaginal tape. Gynecol Obstet Invest. 1999. 48:267–269.

9. Stamey TA. Endoscopic suspension of the vesical neck for urinary incontinence in female. Report on 203 consecutive patients. Ann Surg. 1980. 192:465–471.
10. Abrams P, Blaivas JG, Stanton SL, Andersen JT. The standardisation of terminology of lower urinary tract function. The international continence society committee on standardisation of terminology. Scand J Urol Nephrol Suppl. 1998. 114:5–19.
11. Lose G, Jorgensen L, Mortensen SO, Molsted-Pedersen L, Kristensen JK. Voiding difficulties after colposuspension. Obstet Gynecol. 1987. 69:33–38.

12. Boustead GB. The tension-free vaginal tape for treating female stress urinary incontinence. BJU Int. 2002. 89:687–693.

13. Hong B, Park S, Kim HS, Choo MS. Factors predictive of urinary retention after a tension-free vaginal tape procedure for female stress urinary incontinence. J Urol. 2003. 170:852–856.

14. Groutz A, Gordon D, Lessing JB, Wolman I, Jaffa A, David MP. Prevalence and characteristics of voiding difficulties in women: are subjective symptoms substantiated by objective urodynamic data? Urology. 1999. 54:268–272.

15. Stanton SL, Ozsoy C, Hilton P. Voiding difficulties in the female: prevalence, clinical and urodynamic review. Obstet Gynecol. 1983. 61:144–147.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download