Abstract
Ceramides play major roles in maintaining the epidermal barrier. It has been sus-pected that the depletion of ceramides, associated with disrupted barrier function in the epidermis, leads to the clinical manifestation of dryness and inflammation seen in patients with psoriasis. The aim of the present study was to determine the relation-ship between the level of ceramide synthesis in the epidermis and the clinical severity in patients with psoriasis. Samples from lesional and unlesional epidermis obtained from psoriasis patients were incubated with [14C]serine, an initiator of ceramide syn-thesis. otal ceramide was fractionated using high performance thin layer chromato-graphy, and the radioactivity was measured. The clinical severity of psoriasis was graded according to the psoriasis area and severity index scoring system. The level of ceramide synthesis in the lesional epidermis of patients was significantly lower than that in the unlesional epidermis and bore a negative correlation with the clinical severity of psoriasis. The present results suggest that the decreased level of ceramide synthesis in the epidermis contributes to the clinical severity of psoriasis.
The fundamental function of the epidermis is the provision of an efficient barrier against water loss through the skin (1). This epidermal barrier is formed from the extracellular lipidenriched membranes of the stratum corneum and is organized into membranous multilayers with a repetitive lamellar structure. The intercellular lipid lamellae is composed predominantly of ceramides, cholesterol, and fatty acids which originate from polar lipid precursors provided by cells in the basal layer of the epidermis (2, 3).
Ceramides are the main lipids of the stratum corneum (3, 4). During keratinization, almost all of the epidermal phospholipids, found abundantly in the basal layer, disappear and ceramides, synthesized de novo from phospholipid intermediates, remain within the stratum corneum (4). Ceramide-rich intercellular lipid lamellae are thought to be of particular importance in maintaining the structural integrity of epidermal barrier (5, 6). Depletion of ceramides in the stratum corneum has been suggested as an etiological factor for dryness and barrier disruption in skin conditions such as atopic dermatitis and essential fatty acid deficiency (EFAD) (7-10). The marked depletion of ceramides in the stratum corneum was reported in the patients of atopic dermatitis (7, 8). In essential fatty acid (EFA)-deficient animals, reduction in the levels of lipids, especially ceramides, was shown to bear a correlation to disruptions in the epidermal barrier (9, 10). Several investigators have already addressed the question of altered epidermal ceramide distribution in psoriasis; a negative correlation between ceramide content and transepidermal water loss has been suggested (11-17). However, only limited information is yet available on alterations in the synthesis, not the level, of epidermal ceramides in conditions involving skin dryness and barrier disruption, including psoriasis. In this study, the alterations in epidermal ceramide synthesis as assessed using [14C]serine, and its correlation with the clinical severity was examined in patients with psoriasis.
Ten Korean psoriasis patients (2 women; 8 men) ranging in the age from 21 to 35 yr took part in the present study involving ceramide synthesis. Six Korean psoriasis patients (2 women: 4 men) ranging in the age from 15 to 34 yr took part in the part of the present study involving fatty acid analysis. All of the subjects, who had given their informed consent, had psoriasis vulgaris as identified through clinical and histological assessment and have not been treated either systemically or topically for at least 1 month prior to punch biopsy.
Biopsies using 4-mm punch were taken from the lesional or unlesional skin of the lower extremities, back or arms. Separation of the epidermis was done as described previously (14): specifically, the epidermis was separated from whole skin biopsies by overnight incubation at 4℃ in a one to one (v/v) mixture of Dispase solution (Roche Molecular Biochemicals, Manheim, Germany) and Hank's balanced salt solution (HBSS) (Gibco BRL, Life Technologies, Rockville, MD, U.S.A.).
The clinical severity was assessed using the psoriasis area and severity index (PASI) scoring system. The PASI score is calculated as follows: PASI=0.1(Eh+Ih+Dh)Ah+0.2(Eu+Iu+Du)Au+0.3(Et+It+Dt)At+0.4(El+Il+Dl)Al, where E=erythema; I=infiltration; D=desquamation; A=area; h=head; u=upper extremities; t=trunk; l=lower extremities. A numerical value is given to the extent of the lesions in each area: 1=<10%; 2=10-30%; 3=30-50%; 4=50-70%; 5=70-90%; and 6=90-100%. E, I, and D are scored according to a five-point scale (0=no symptoms; 1=slight; 2=moderate; 3=marked; 4=very marked) to obtain a final PASI score between 0 and 72. The PASI score of the patients who took part in this study ranged between 2.4 and 22.4; this range corresponds to mild and moderate psoriasis. Only those patients with PASI<25 were enrolled in this study in order to determine whether alterations in the level of either ceramide synthesis or fatty acids bear a close-enough correlation to the clinical severity in mild to moderate status of psoriasis.
Because the process of ceramide synthesis is initiated by incorporation of serine, ceramide synthesis was determined by incubating the separated epidermis (4-mm punch biopsy specimen) in 1 mL Krebs bicarbonate buffer (pH 7.5) containing [14C]serine (0.1 µCi/mL) at 37℃ for 16 hr as a previously described method (15). After incubation, the epidermis was washed with PBS and homogenized. The total lipids were extracted using a CHCl3: MeOH (2:1, v/v) mixture. The extracted lipids (lower phase) were subjected to high performance thin layer chromatography (HP-TLC) on 0.20-mm silicagel 60-coated plates (Whatman, Clifton, NJ, U.S.A.) according to the modified method reported by Uchida et al. (16). Specifically, the samples applied on the plates were first eluted up to 1.0 cm and then up to 3.5 cm using a CHCl3: MeOH: acetone (76: 20:4, v/v/v) solution, then up to 7.5 cm using a CHCl3: Acetone: MeOH (80:10:10, v/v/v) solution, and finally up to the top using a CHCl3: Ethylacetate: Ether: MeOH (76:20:6:2, v/v/v/v) solution. Each stage of elution was carried out after the plates were completely air-dried. The ceramide-containing fractions that comigrated with their respective standards were visualized by 2,7-dichlorofluorescein spray and eluted from the plates using a CHCl3:MeOH (2:1, v/v) solution. The eluates were dried in N2 gas and the radioactivity was measured using a Beckman scintillation counter.
To compare each samples, the level of radioactivity was normalized according to the amount of protein extracted from the separated epidermis. The upper phase of lipid extraction stage, which contained epidermal homogenates, was centrifuged at 800 g for 5 min to remove tissue debris, and the protein concentration was determined according to the modified Lowry method (17) using bovine serum albumin as a standard. De novo synthesis of ceramides was assessed as cpm/µg protein.
Fatty acids are found chiefly in the intercellular lipid lamellae of the epidermal barrier (2, 3). The fatty acid profiles of the total lipid contents extracted from the separated epidermis were determined by gas chromatography after transmethylation in 6% methanolic HCl (18). The gas chromatography device employed (Hewlett-Packard 5730A) was equipped with a SPB-225-fused silica capillary column (30 m×0.25 mm×0.15 µm, Supelco, Bellefonte, PA, U.S.A.) with an initial oven temperature of 140℃ which increases by 4℃/min to a final temperature of 240℃. Detection was performed by using a flame ionization detector (FID). Methylheptadecanoate was used as an internal standard to assess the relative amounts of various fatty acids. The separated fatty acids were also identified by comparing retention times of the external standards (Supelco, Bellefonte, PA, U.S.A.).
Statistical significance of the differences in the levels of ceramide synthesis and fatty acids between lesional and unlesional samples of psoriasis patients was assessed by paired t-test. Correlation between the levels of ceramide synthesis and PASI scores was determined using Pearson correlation test. p-values<0.05 were considered to be statistical significance.
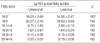
The levels of ceramide synthesis in the lesional and unlesional epidermis, and the PASI scores of the subjects are shown in Table 1. Although the absolute level of ceramide synthesis differed between the patients, the level of ceramide synthesis in the lesional epidermis was always significantly less (p<0.01) than that in the unlesional epidermis, with the percentage reduction ranging from 4.32 to 78.80. A highly significant positive correlation between the percentage reduction of ceramide synthesis and PASI score was observed (r=0.967, p=0.0004), as shown in Fig. 1. These results indicate that the level of ceramide synthesis is inversely correlated with the PASI score in mild to moderate psoriasis.
The levels of fatty acids were analyzed from total lipid extracts of lesional and unlesional epidermis of subjects (Table 2). The levels of saturated fatty acids such as palmitic (16:0) and stearic acids (18:0) were higher than the overall level of unsaturated fatty acids. However, there were no significant differences in the levels of these fatty acids between lesional and unlesional epidermis. Furthermore, the level of linoleic acid (18:2n-6), a major unsaturated fatty acid which is essential for maintaining the epidermal barrier (20, 21), was not altered in the lesional epidermis of the subjects. In addition, no correlation was observed between the level of fatty acids and the PASI score (data not shown).
Although decreased ceramide levels have been reported in skin conditions involving dryness and barrier disruption such as psoriasis (7-17), alterations in the level of ceramide synthesis in this context has not been examined, and the possible relationship between such change and the clinical severity of psoriasis even less. The present study shows that the level of ceramide synthesis is significantly reduced in the lesional epidermis, which inversely correlates with the clinical severity in mild to moderate psoriasis.
The epidermal barrier assumes the structure of a lipid-enriched multilamellae in the stratum corneum, which lipid content is predominantly composed of ceramides, cholesterol and free fatty acids (2, 3). Ceramides bearing the moieties of amidelinked non-hydroxy acid, α-hydroxy acid, or ω-hydroxy acid and ester-linked fatty acids on sphingosine provide the driving force for lamellar assembly (19), and these structural moieties are thought to be important in maintaining the structural integrity of epidermal barrier against water loss through the skin (5, 6). Correspondingly, decreases in the level of ceramides have been associated with skin conditions involving dryness and barrier disruption, such as atopic dermatitis (7, 8), EFAD (9, 10), xerosis (21), and psoriasis (11-17). Such skin conditions are characterized by changes in the levels of free fatty acids, especially linoleic acid (LA) (18:2n-6) (19, 20). The lamellar granules in linoleate-deficient animals have been reported to contain amorphous and consequently only fragmentary lamellae in the stratum corneum (20). In view of the functional importance of LA in maintaining the structural integrity of the epidermal barrier (19, 20), the linoleate moiety of ceramide 1 thus appears to favor lipid lamellar packing (22). However, the assessment of the lesional epidermis of psoriasis patients revealed no alteration in the levels of LA or other fatty acids compared with the unlesional epidermis of the same patients (Table 2). In addition, no relationship was observed between the levels of fatty acids and the PASI score in mild to moderate psoriasis. On the other hand, the level of ceramide synthesis was significantly reduced in the lesional epidermis of patients (Table 1). These results are in concordance with the results of earlier studies in which decreases in the levels of ceramides, specifically ceramide 1, 4, and 5, have been shown to be associated with increased transepidermal water loss in the psoriatic epidermis (11). Furthermore, a positive correlation between the percentage reduction of ceramide synthesis in the lesional epidermis and clinical severity (r=0.967, p=0.0004) has been demonstrated in this study (Fig. 1). Only those patients with mild to moderate psoriasis took part in our study, our data demonstrate that reduction of ceramide synthesis in the lesional epidermis is sensitive enough to make an inverse correlation with clinical severity in mild to moderate status of psoriasis.
The level of ceramides in the epidermis is regulated by a balance in the activity of ceramide generating enzymes such as serine palmitoyl transferase in the de novo synthesis pathway, sphingomyelinase, and β-glucocerebrosidase and that of the degradative enzyme such as ceramidase (23). Ceramides in the stratum corneum are originally derived from sphingomyelin and β-glucosylceramides. No apparent difference in sphingomyelinase and β-glucocerebrosidase activities was observed between patients with atopic dermatitis and agedmatched controls (23, 24). As opposed to the usage of stripped stratum corneum in previous studies (23, 24), the whole epidermis was used in the present study. The percentage reduction of ceramide synthesis was observed in this study together with the finding that no change in sphingomyelinase and β-glucocerebrosidase activities is observed in the stratum corneum (23, 24), which seems to indicate a depression in the activity of serine palmitoyl transferase in the lesional epidermis of psoriasis patients. Extremely high activities of ceramidase (25) and sphingomyelin deacylase (26), which hydrolyze sphingomyelin into sphingophosphorylcholine and free fatty acid, have been demonstrated to be the metabolic features leading to low levels of ceramides in the stratum corneum in atopic dermatitis; however, ceramidase activity was not altered in the stratum corneum in psoriasis (25). Together with these findings, the present data suggest that the dramatic reduction in ceramide synthesis, which has been found to bear a significant correlation to the clinical severity, is caused by a decrease in the activity of serine palmitoyl transferase. However, the complete relationship between ceramide content and activity of ceramide-metabolizing enzymes in the psoriatic skin remains to be clarified.
In conclusion, we demonstrate that the level of ceramide synthesis is significantly reduced in the lesional epidermis, which is sensitive enough to make an inverse correlation with clinical severity in mild to moderate status of psoriasis. We are not certain whether this finding is primary or secondary event in psoriasis. However, we suggest that the reduction of synthetic capacity of ceramide is the important one of the severity-related factors.
Figures and Tables
Fig. 1
Correlation between percentage reductions of ceramide synthesis in lesional epidermis and PASI scores of subjects.

References
1. Elias PM, Menon GK. Structural and lipid biochemical correlates of the epidermal permeability barrier. Adv Lipid Res. 1991. 24:1–26.

2. Rogers J, Harding C, Mayo A, Banks J, Rawlings A. Stratum corneum lipids; the effect of ageing and the seasons. Arch Dermatol Res. 1996. 288:765–770.

3. Gray GM, White RJ, Williams RH, Yardley HJ. Lipid composition of the superficial stratum corneum cells of pig epidermis. Br J Dermatol. 1982. 106:59–63.

4. Hedberg CL, Wetz PW, Downing DT. The time course of lipid biosynthesis in pig epidermis. J Invest Dermatol. 1988. 91:169–174.

5. Grubauer G, Feingold KR, Harris RM, Elias PM. Lipid content and lipid type as determinants of the epidermal permeability barrier. J Lipid Res. 1989. 30:89–96.

6. Wertz PW, Cho ES, Downing DT. Effect of essential fatty acid deficiency on the epidermal sphingolipids of the rat. Biochim Biophys Acta. 1983. 753:350–355.

7. Imokawa G, Abe A, Jin K, Higaki Y, Kawashima M, Hidano A. Decreased level of ceramides in stratum corneum of atopic dermatitis: an etiologic factor in atopic dry skin. J Invest Dermatol. 1991. 96:523–526.

8. Matsumoto M, Umemoto N, Sugiura H, Uehara M. Difference in ceramide composition between "dry" and normal skin in patients with atopic dermatitis. Acta Derm Venereol (Stockh). 1999. 79:246–247.
9. Burr GO, Burr MM. Nutrition classics from J Biol Chem 82: 345-67, 1929. A new deficiency disease produced by the rigid exclusion of fat from the diet. Nutr Rev. 1973. 31:248–249.
10. Chung S, Kong S, Seong K, Cho Y. γ-Linolenic acid in borage oil reverses epidermal hyperproliferation in guinea pigs. J Nutr. 2002. 132:3090–3097.

11. Motta S, Monti M, Sesana S, Mellesi L, Ghidoni R, Caputo R. Abnormality of water barrier function in psoriasis. Role of ceramide functions. Arch Dermatol. 1994. 130:452–456.
13. Serup J, Blichmann C. Epidermal hydration of psoriasis plaques and the relation to scaling. Measurement of electrical conductance and transepidermal water loss. Acta Derm Venereol. 1987. 67:357–359.
14. Macheleidt O, Kaiser HW, Sandhoff K. Deficiency of epidermal protein-bound ω-hydroxyceramides in atopic dermatitis. J Invest Dermatol. 2002. 119:166–173.

15. Tohyama J, Oya Y, Ezoe T, Vanier MT, Nakayasu H, Fujita N, Suzuki K. Ceramide accumulation is associated with increased apoptotic cell death in cultured fibroblasts of sphingolipid activator protein-deficient mouse but not in fibroblasts of patients with Farber disease. J Inherit Metab Dis. 1999. 22:649–662.

16. Uchida Y, Hara M, Nishio H, Sidransky E, Inoue S, Otsuka F, Suzuki A, Elias PM, Holleran WM, Hamanaka S. Epidermal sphingomyelins are precursors for selected stratum corneum ceramides. J Lipid Res. 2000. 41:2071–2082.

17. Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the folin phenol reagent. J Biol Chem. 1951. 193:265–275.

18. Tang W, Ziboh VA. Reversal of epidermal hyperproliferation in essential fatty acid deficient guinea pigs is accompanied by rapid generation of inositol triphosphate. Arch Dermatol Res. 1988. 280:286–292.

19. Wertz PW, Swartzendruber DC, Abraham W, Madison KC, Downing DT. Essential fatty acids and epidermal integrity. Arch Dermatol. 1987. 123:1381–1384.

20. Elias PM, Brown BE. The mammalian cutaneous permeability barrier: defective barrier function in essential fatty acid deficiency correlates with abnormal intercellular lipid deposition. Lab Invest. 1978. 39:574–583.
21. Akimoto K, Yoshikawa N, Higaki Y, Kawashima M, Imokawa G. Quantitative analysis of stratum corneum lipids in xerosis and asteatotic eczema. J Dermatol. 1993. 20:1–6.

22. Bouwstra JA, Gooris GS, Dubbelaar FE, Weerheim AM, Ijzerman AP, Ponec M. Role of ceramide 1 in the molecular organization of the stratum corneum lipids. J Lipid Res. 1998. 39:186–196.

24. Jin K, Higaki Y, Takagi Y, Higuchi K, Yada Y, Kawashima M, Imokawa G. Analysis of beta-glucocerebrosidase and ceramidase activities in atopic and aged dry skin. Acta Derm Venereol. 1994. 74:337–340.
25. Aioi A, Tonogaito H, Suto H, Hamada K, Ra C, Ogawa H, Maibach H, Matsudas H. Impairment of skin barrier function in NC/Nga Tnd mice as a possible model for atopic dermatitis. Br J Dermatol. 2001. 144:12–18.

26. Hara J, Hoguchi K, Okamoto R, Kawashima M, Imokawa G. High expression of sphingomyelin deacylase is an important determinant of ceramide deficiency leading to barrier disruption in atopic dermatitis. J Invest Dermatol. 2000. 115:406–413.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download