Abstract
The main objectives of the current study were to evaluate the efficacy and safety of a CEOP-E regimen for patients with aggressive non-Hodgkin's lymphoma (NHL). Fifty-one consecutive patients with newly diagnosed aggressive NHL were enrolled in the study. Median age of patients was 57 (range, 18-75) yr old, and male to female ratio was 1.32:1. Diffuse large B cell lymphoma (68.8%) was the most common histological subtype. Thirty patients (58.8%) had Ann Arbor stage III or IV diseases at diagnosis. One course of chemotherapy consisted of an intravenous combination of cyclophosphamide 750 mg/m2, epirubicin 50 mg/m2, vincristine 2 mg, etoposide 80 mg/m2 on day 1 and oral administration of 100 mg prednisone on days 1 to 5 (CEOP-E). A complete response or unconfirmed complete response was achieved in 31 (63.3%) out of 49 evaluated patients. With a median follow-up of 16.3 months, 26 events including relapse and death were observed. The estimated 2-yr survival rate for all patients and disease free survival rate for patients achieving complete re-sponse was 58.9% and 57.1%, respectively. Episodes of febrile neutropenia occurred in 5 (10.2%) patients. Transient episodes of ECG abnormality (1st degree AV block) were observed in 2 patients. Accordingly, the CEOP-E regimen produced comparable results to those of other regimens, including CHOP, in terms of the response rate and overall survival. The current regimen seemed to minimize the cardiac toxicity due to an accumulated dose of anthracycline in the treatment of aggressive NHL.
Patients with aggressive non-Hodgkin's lymphoma (NHL) can be cured with various chemotherapy regimens, yet the cure rates vary according to the pretreatment prognostic variables. Even though several attempts at devising more effective regimens, cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) combination chemotherapy, which showed 44% of complete response rate (CR), 42% of 3-yr disease free survival (DFS) rate, and 54% of 3-yr overall survival (OS) rate, is still considered as the best available chemotherapeutic regimen for aggressive NHL (1, 2). Although chemotherapy can cure most patients with a localized disease, only 30% to 40% of patients with an advanced disease are cured (1-4). Therefore, the major concern for treating aggressive NHL is still to prolong survival and reduce treatment-related toxicity.
Etoposide has already been reported as an active agent in the treatment of aggressive NHL (5, 6). In a first-line therapy, a phase II study with CHOP plus etoposide regimen showed 93% of response rate and 43 months of median survival (5). Moreover, various combination regimens including etoposide are widely used for treating refractory or relapsed lymphomas. As regards anthracyclines that are effective in treating NHL, doxorubicin is most commonly used. However, Lambertenghi et al. (7) reported 59% of CR rate and 67% of 7-yr DFS rate with CEOP regimen, replacing doxorubicin with epirubicin (4'-epidoxorubicin). Previous other studies also have indicated that epirubicin, a derivative of doxorubicin with a different configuration of the hydroxyl group at the 4'position, might be equally effective with less cardiac and hematologic toxicity (7-9).
Accordingly, the current phase II study was conducted to evaluate the response rate, toxicity, and survival of a modified CHOP regimen (the addition of etoposide and replacement of doxorubicin with epirubicin) for patients with aggressive NHL.
Patients entered onto this study were required to fulfill the following eligibility criteria: (1) histologically proven aggressive non-Hodgkin's lymphoma; (2) age between 15 and 75 yr; (3) Eastern Cooperative Oncology Group Scale performance status of 3 or less; (4) at least one measurable lesion; (5) adequate function of bone marrow (WBC count ≥4,000/µL and platelet count ≥100,000/µL), liver (serum bilirubin level ≤2.0 mg/dL and serum transaminase level ≤two times the upper limit of normal range, and kidney (serum creatinine level ≤1.5 mg/dL); (6) normal cardiac function; (7) no other severe medical conditions; (8) no other active malignancy; and (9) provision of written informed consent.
All cases were reviewed by an expert hematopathologist for diagnostic confirmation and classified according to the revised European-American classification of lymphoid neoplasm system (10). Pretreatment evaluation comprised complete blood cell counts, routine chemistry measurement including serum lactate dehydrogenase (LDH), chest and abdominal CT scan, bone marrow examination and other tests when clinically indicated. The disease stage was determined using the Ann Arbor criteria, and all patients were evaluated for the presence of risk factors according to the International Prognostic Index based on age, stage, performance status, number of extranodal sites of disease, and LDH (11).
One course of chemotherapy consisted of an intravenous combination of cyclophosphamide 750 mg/m2, epirubicin 50 mg/m2, vincristine 2 mg, and etoposide 80 mg/m2 on day 1 and oral administration of 100 mg prednisone on days 1 to 5 (CEOP-E), which was repeated every 3 weeks. Patients with a stage I or II disease were planned to receive four courses of chemotherapy followed by involved-field radiotherapy (30-40 Gy), while patients with an advanced disease were planned to receive six courses of chemotherapy followed by radiotherapy to bulky sites. Chemotherapy was withheld for 1 week until the neutrophil count was higher than 1.5×103/µL and the platelet count more than 100×109/L. If febrile neutropenia or grade IV neutropenia occurred, the starting dose of cyclophosphamide, epirubicin, and etoposide was reduced by 25% in the subsequent course of treatment. The prophylactic use of a colony-stimulating factor was not permitted. To evaluate the cardiac toxicity, electrocardiography and chest radiography were performed before and after every second course of chemotherapy and 2D echocardiography was conducted when clinically indicated.
The patient response was evaluated after three courses of treatment and 1 month after completion of treatment. In patients with a stage I or II disease, the response evaluated after completion of radiotherapy was regarded as a maximal response. A complete response was defined as the disappearance of all clinical evidence of disease and normalization of those biochemical abnormalities (e.g. LDH). An unconfirmed complete response was defined as a residual lymph node mass with a diameter greater than 1.5 cm after a 75% or more reduction in the sum of the diameters of all measurable lesions. A partial response was defined as a 50% or more reduction in the sum of the diameters of all measurable lesions that persisted for at least 4 weeks, no increase in the size of any preexisting lesions, and no new lesions. A stable disease was defined as less than a partial response, yet not progressive. A progressive disease was defined as 50% or more increase in the sum of the diameters of any measurable lesions or the appearance of a new lesion (12). Toxicity was evaluated and graded according to the National Cancer Institute Common Toxicity Criteria (NCI CTC) version 2.0 grading system.
An optimal, two-stage Simon design was used to determine the exact number of patients to be accrued in the current trial. The hypotheses was that H0: P≤P0 (0.30) versus H1: P≥P1 (0.50) with α=0.05, and β=0.20 (80% power). Therefore, 19 patients were enrolled in the first stage of trial and evaluated for response. If 7 or more patients showed a CR, then the study proceeded to the second stage. Allowing for a follow-up loss rate of 10%, the total sample size was 43 patients with a measurable disease. OS was measured from the study entry until the date of death or last follow-up and progression free survival (PFS) was calculated from the study entry until treatment failure (disease progression, relapse, or death of any cause). DFS was measured from the date of a complete response until the date of the first relapse, death, or last follow-up. The efficacy and toxicity was analyzed by per protocol base. OS curves were plotted using the Kaplan-Meier method and compared using a log-rank test. The statistical data were obtained using the SPSS software package (SPSS 10.0 Inc. Chicago, IL, U.S.A.).
Fifty-one consecutive patients with newly diagnosed aggressive NHL were enrolled in the study from February 2000 to November 2002 at Kyungpook National University Hospital (Daegu, Korea). The patient characteristics are summarized in Table 1. Diffuse large B cell lymphoma (68.8%) was the most common histological subtype, while 13 (25.5%) patients were diagnosed with peripheral T cell lymphomas. Thirty patients (58.8%) had Ann Arbor stage III or IV diseases at diagnosis and 17 (33.3%) patients were classified as high-intermediate or high risk according to the International Prognostic Index (IPI) scoring system. The characteristics including age, stage, bulky disease, and IPI between B cell subtypes and T cell subtypes were not significantly different.
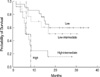
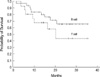
The responses of two patients were not evaluated due to follow-up loss, as such, these patients were withdrawn from the study. Eighteen (85.7%) out of 21 patients with localized disease completed a planned chemotherapy followed by involved field radiotherapy. A CR or unconfirmed complete response was achieved in 31 (63.3%) out of 49 patients (Table 2). With a median follow-up of 16.3 months, 26 events (10 relapses or 16 deaths) were observed. Fifteen out of 16 deaths were due to disease progression, and 1 patient died of febrile neutropenia and pneumonia. Estimated 2-yr survival rate and PFS rate for all patients was 58.9% and 43.8%, respectively (Fig. 1A, B). DFS rate for patients achieving a complete response was 57.1% (Fig. 1C). A statistically significant difference in the PFS rate was observed among the subgroups according to the IPI (estimated 2-yr PFS rate for low, low-intermediate, high-intermediate, and high risk groups was 59.9%, 51.5%, 16.7%, and 0%, respectively, p=0.0043) (Fig. 2). Estimated 2-yr OS rate was not statistically different between for patients with B cell NHL and with T cell NHL (66.0% vs. 58.7%, p=0.1840) (Fig. 3).
A total of 229 courses of chemotherapy were administrated to 49 patients. Thirty-six (73.5%) of the 49 patients completed the planned treatment schedule. Treatment delays were observed in 12 (24.5%) patients due to neutropenia or thrombocytopenia. A dose reduction was required in 10 (20.4%) patients. The median dose intensity for the cyclophosphamide, epirubicin, vincristine, and etoposide over all treatment cycles was 221.8 mg/m2/week, 14.8 mg/m2/week, 6.6 mg/m2/week, and 23.4 mg/m2/week, corresponding to 88.7%, 88.7%, 98.2 %, and 87.6% of the planned dose intensities, respectively.
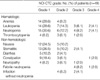
NCI CTC grade III or IV neutropenia occurred in 6 (12.2%) patients, and episodes of grade III or IV febrile neutropenia was observed in 5 (10.2%) patients (Table 3). Nausea and stomatitis were the most common non-hematological toxicities. Grade 1/2 nausea and stomatitis was observed in 34.7% and 36.7% of patients, respectively (Table 3). Transient episodes of ECG abnormality (1st degree AV block) were observed in two patients, yet they showed normal ejection fraction in 2D echocardiography. Secondary leukemia or myelodysplastic syndrome induced by etoposide or other chemotherapeutic agents was not observed.
The main objectives of the current study were to improve the response rate with a modified CHOP regimen including etoposide and reduce the toxicity associated with anthracyclines in the treatment of patients with aggressive NHL. As a result, a complete response was observed in 63.3% of the patients, while estimated 2-yr OS and DFS rate was 58.9% and 57.1%, respectively. These results are similar to those recorded in previous trials using a CHOP regimen for patients with aggressive NHL, where the complete response rates ranged from 44-74% and estimated 2 or 3-yr DFS rate ranged from 44-64% (2, 13-15). A subgroup analysis of the current series revealed that patients in the high-intermediate and high-risk groups with respect to the IPI scoring system had an OS rate of 43.2%, whereas patients in the low and low-intermediate risk groups had an OS rate of 67.8% after 2 yr (Fig. 2A). These results are comparable to those of the International NHL Prognostic Factors Project (11) that included 3,273 patients with aggressive NHL.
The current study included a relatively large proportion (25.5%) of peripheral T cell lymphomas, which are known to have a poorer prognosis than B cell lymphomas (16, 17). Nonetheless, the OS rate for patients with peripheral T cell lymphomas was not statistically different from that for patients with B cell lymphomas (Fig. 3). Previous studies on CHOP plus etoposide regimens have also reported on improved treatment results for various subtypes of NHL (5, 6, 18). Karakas et al. (6) found that peripheral T-cell lymphomas responded well to a CHOP plus etoposide regimen with a similar outcome to high-grade B-cell lymphomas. Therefore, given these results, it was postulated that the addition of etoposide to a CEOP regimen could improve the outcome of peripheral T cell lymphomas.
The administration of doxorubicin in the treatment of NHL has occasionally exhibited limitations due to dose-related congestive cardiomyopathy. Haddy et al. (19) reported that left ventricular dysfunction as a significant late toxic event in long-term survivors of high-grade NHL was identified in eight (14.0%) of 57 patients who received more than 200 mg/m2 of doxorubicin. Miller et al. (15) also have observed left ventricular dysfunction in 1.5% of patients treated after eight cycles of CHOP. Cardiac toxicity is more problematic in a relapsed setting, since relapsed patients are mostly exposed to additional anthracyclines or higher doses of other cardiotoxic agents for salvage therapy or high-dose chemotherapy with stem cell support. As such, less cardiotoxic, yet equally efficacious, anthracycline agent is preferred as a frontline drug for NHL. Epirubicin in combination with other chemotherapeutic agents exhibited 58.3-90% of CR rates and 61.8-63.5% of 5-yr DFS rate in the previous studies (20-22), which were similar therapeutic activity to doxorubicin in combination with other agents. However, epirubicin has a more favorable adverse effect profile with lower hematologic toxicity, mucositis, and cardiac toxicity (23). In the current study, febrile neutropenia was observed in 10.2% of patients, while grade III or IV neutropenia was only observed in 12.2% of patients, despite the addition of etoposide to a CEOP regimen. Plus, no clinically significant cardiac event was recorded. Thus, cardiac morbidity due to salvage regimens or high-dose chemotherapy with stem cell support may be minimized in relapsing patients who have been treated with a regimen including epirubicin.
In Coiffier et al.'s study (24) on the addition of rituximab to a CHOP regimen, which improved survival in elderly patients with diffuse large B cell lymphomas, grade III or IV cardiac toxicity was observed in 8% of patients. Therefore, especially for elderly patients with NHL, epirubicin may be more appropriate than doxorubicin as the anthracycline component of the first-line regimen. Furthermore, clinical trials using rituximab plus a CEOP or CEOP+E regimen to reduce the toxicities in elderly patients can be planned.
In conclusion, the CEOP-E regimen was found to be comparable to other regimens, including CHOP, in terms of the response rate and overall survival, and seemed to apparently minimize the cardiac toxicity due to an accumulated dose of anthracycline in the treatment of aggressive NHL.
Figures and Tables
Fig. 1
Survival curves. (A) Estimated 2-yr overall survival rate and (B) DFS rate for all patients was 58.9% and 43.8%, respectively. (C) Disease-free survival rate for patients that achieved complete response was 57.1%.

Fig. 2
Survival curves according to International Prognostic Index. Estimated 2-yr PFS rate for low, low-intermediate, high-intermediate, and high risk groups was 59.9%, 51.5%, 16.7%, and 0%, respectively (p=0.0043).
References
1. Gordon LI, Harrington D, Andersen J, Colgan J, Glick J, Neiman R, Mann R, Resnick GD, Barcos M, Gottlieb A. Comparison of a second generation combination chemotherapeutic regimen (m-BACOD) with a standard regimen (CHOP) for advanced diffuse non-Hodgkin's lymphoma. N Engl J Med. 1992. 327:1342–1349.
2. Fisher RI, Gaynor ER, Dahlberg S, Oken MM, Grogan TM, Mize EM, Glick JH, Coltman CA Jr, Miller TP. Comparison of a standard regimen (CHOP) with three intensive chemotherapy regimens for advanced non-Hodgkin's lymphoma. N Engl J Med. 1993. 328:1002–1006.

3. Longo DL, DeVita VT Jr, Duffey PL, Wesley MN, Ihde DC, Hubbard SM, Gilliom M, Jaffe ES, Cossman J, Fisher RI. Superiority of ProMACE-CytaBOM over ProMACE-MOPP in the treatment of advanced diffuse aggressive lymphoma: results of a prospective randomized trial. J Clin Oncol. 1991. 9:25–38.

4. Shipp MA, Yeap BY, Harrington DP, Klatt MM, Pinkus GS, Jochelson MS, Rosenthal OS, Skarin AT, Canellos GP. The m-BACOD combination chemotherapy regimen in large-cell lymphoma: analysis of the completed trial and comparison with M-BACOD regimen. J Clin Oncol. 1990. 8:84–93.
5. Koppler H, Pfluger KH, Eschenbach I, Pfab R, Lennert K, Wellens W, Schmidt M, Gassel WD, Kolb T, Hassler R. CHOP-VP16 chemotherapy and involved field irradiation for high grade non-Hodgkin's lymphomas: a phase II multicentre study. Br J Cancer. 1989. 60:79–82.

6. Karakas T, Bergmann L, Stutte HJ, Jager E, Knuth A, Weidmann E, Mitrou PS, Hoelzer D. Peripheral T-cell lymphomas respond well to vincristine, adriamycin, cyclophosphamide, prednisone and etoposide (VACPE) and have a similar outcome as high-grade B-cell lymphomas. Leuk lymphoma. 1996. 24:121–129.

7. Lambertenghi Deliliers G, Butti C, Baldini L, Ceriani A, Lombardi F, Luoni M, Montalbetti L, Pavia G, Pinotti G, Pogliani E, Cassi E, Pisoni GB. A cooperative study of epirubicin with cyclophosphamide, vincristine and prednisone (CEOP) in non-Hodgkin's lymphoma. Haematologica. 1995. 80:318–324.
8. De Lena M, Maiello E, Lorusso V, Brandi M, Calabrese P, Romito S, Mazzei A, Marzullo F. Comparison of CHOP-B vs CEOP-B in poor prognosis non-Hodgkin's lymphomas. A randomized trial. Med Oncol Tumor Pharmacother. 1989. 6:163–169.

9. Chim CS, Kwong YL, Lie AK, Lee CK, Liang R. CEOP treatment results and validity of the international prognostic index in Chinese patients with aggressive non-Hodgkin's lymphoma. Hematol Oncol. 1998. 16:117–123.

10. Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, Delsol G, De Wolf-Peeters C, Falini B, Gatter KC. A revised European-American classification of lymphoid neoplasms: a proposal from the international lymphoma study group. Blood. 1994. 84:1361–1392.
11. The International Non-Hodgkin's Lymphoma Prognostic Factor Project. A predictive model for aggressive non-Hodgkin's lymphoma. N Engl J Med. 1993. 329:987–994.
12. Cheson BD, Horning SJ, Coiffier B, Shipp MA, Fisher RI, Connors JM, Lister TA, Vose J, Grillo-Lopez A, Hagenbeek A, Cabanillas F, Klippensten D, Hiddemann W, Castellino R, Harris NL, Armitage JO, Carter W, Hoppe R, Canellos GP. Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. J Clin Oncol. 1999. 17:1244.

13. Armitage JO, Fyfe MA, Lewis J. Long-term remission durability and functional status of patients treated for diffuse histiocytic lymphoma with the CHOP regimen. J Clin Oncol. 1984. 2:898–902.

14. Gams RA, Rainey M, Dandy M, Bartolucci AA, Silberman H, Omura G. Phase III study of BCOP versus CHOP in unfavorable categories of malignant lymphoma: a Southeastern Cancer Study Group trial. J Clin Oncol. 1985. 3:1188–1195.
15. Miller TP, Dahlberg S, Cassady JR, Adelstein DJ, Spier CM, Grogan TM, LeBlanc M, Carlin S, Chase E, Fisher RI. Chemotherapy alone compared with chemotherapy plus radiotherapy for localized intermediate- and high-grade non-Hodgkin's lymphoma. N Engl J Med. 1998. 339:21–26.

16. Melnyk A, Rodriguez A, Pugh WC, Cabannillas F. Evaluation of the Revised European-American Lymphoma Classification confirms the clinical relevance of immunophenotype in 560 cases of aggressive non-Hodgkin's lymphoma. Blood. 1997. 89:4514–4520.

17. Gisselbrecht C, Gaulard P, Lepage E, Coiffier B, Briere J, Haioun C, Cazals-Hatem D, Bosly A, Xerri L, Tilly H, Berger F, Bouhabdallah R, Diebold J. Prognostic significance of T-cell phenotype in aggressive non-Hodgkin's lymphomas. Blood. 1998. 92:76–82.
18. Pfreundschuh M, Trumper L, Kloess M, Schmits R, Feller AC, Rudolph C, Reiser M, Hossfeld DK, Metzner B, Hasenclever D, Schmitz N, Glass B, Rube C, Loeffler M. 2-weekly vs. 3-weekly CHOP with and without etoposide in young patients with low-risk (low LDH) aggressive non-Hodgkin's lymphoma: Results of the Completed NHL-B-1 Trial of the DSHNHL. Blood. 2002. 100:92a. [abstract].
19. Haddy TB, Adde MA, McCalla J, Domanski MJ, Datiles M 3rd, Meehan SC, Pikus A, Shad AT, Valdez I, Lopez Vivino L, Magrath IT. Late effects in long term survivors of high grade non-Hodgkin's lymphomas. J Clin Oncol. 1998. 16:2070–2079.
20. Basaran M, Bavbek ES, Sakar B, Eralp Y, Alici S, Tas F, Yaman F, Dogan O, Camlica H, Onat H. Treatment of aggressive non-Hodgkin's lymphoma with dose-intensified epirubicin in combination of cyclophosphamide, vincristine, and prednisone (CEOP-100); A phase II study. Am J Clin Oncol. 2001. 24:570–575.
21. Mugitani A, Tatsumi Y, Tanaka K, Yasui Y, Inoue T. Cyclophosphamide, epirubicin, vincristine, prednisone, bleomycin, etoposide (CEOP-BE) therapy for intermediate- and high grade non-Hodgkin's lymphomas. Anticancer Res. 1999. 19:3393–3397.
22. Nair R, Ramakrishnan G, Nair NN, Saikia TK, Parikh PM, Joshi SR, Soman CS, Mukhadan M, Dinshaw KT, Advani SH. A randomized comparison of the efficacy and toxicity of epirubicin and doxorubicin in the treatment of patients with non-Hodgkin's lymphoma. Cancer. 1998. 82:2282–2288.

23. Case DC, Gams R, Ervin TJ, Boyd MA, Oldham FB. Phase I-II trial of high-dose epirubicin in patients with lymphoma. Cancer Res. 1987. 47:6393–6396.
24. Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, Morel P, Van Den Neste E, Salles G, Gaulard P, Reyes F, Lederlin P, Gisselbrecht C. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med. 2002. 346:235–242.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download