Abstract
"Hyalinizing spindle cell tumor with giant rosettes" (HSCTGR) is a recently described tumor, which is regarded as an unusual variant of low-grade fibromyxoid sarcoma. Proof of a metastatic potential was lacking. The patient in the report was a 35-yr-old woman who showed multiple bilateral pulmonary nodules with massive pleural effusion in the right side. She had a history of a mass excision in the right thigh 11 yrs ago at another hospital, which was reported as a "leiomyoma". Two years before this presentation, the patient received a routine chest radiograph which demonstrated bilateral multiple pulmonary nodules. A lobectomy of the left upper lung was performed. The histological findings revealed a well-circumscribed nodule that was characterized by a spindle-shaped fibrous to hyalinized stroma with criss-crossing short fascicles and giant collagen rosettes surrounded by a rim of spindle-shaped cells. Electron microscopy confirmed the fibroblastic nature of the tumor. This case, in addition to at least two other cases reported in the literature, demonstrates that the HSCTGR is a malignant neoplasm with the capacity to metastasize after a long hiatus.
"Hyalinizing spindle cell tumor with giant rosettes" (HSCTGR) is an unusual fibrous tumor in the deep soft tissue. It was first described by Lane et al. in 1997, and was reported to represent a form of low-grade fibromyxoid sarcoma (1). They reported that this tumor is found in the deep soft tissues of proximal extremities in young to middle-aged adults, and it behaves in a benign fashion after a short follow-up period (1, 2). Based on 19 examined cases, they reported that none of the 19 tumors metastasized (1). However, since the initial report, two patients with pulmonary metastases (3, 4) as well as another patient with multiple pulmonary nodules in the absence of an identifiable primary tumor (5) have been reported. We recently observed an unusual case of a lung lesion that was histologically similar to a HSCTGR of soft tissues.
This article reports a metastatic HSCTGR in the lung in a 35-yr-old woman after a previous mass excision in the right thigh 11 yr ago along with ultrastructural and immunohistochemical findings.
The patient was a 35-yr-old woman who showed multiple bilateral pulmonary nodules on a routine chest radiograph. Because she had no specific symptoms related to the lung nodules, no treatment was received. Two years later, she was admitted complaining of coughing and dyspnea due to massive pleurisy. A chest computed tomographic examination showed several variable-sized bilateral pulmonary nodules (up to 8 cm in the greatest diameter) with a massive pleural effusion in the right side causing collapse of the right lung, and displacing the mediastinum to the left (Fig. 1). Several irregular nodular opacities along the right pleural surface were noted. A total body CT examination confirmed there were no pathologic findings in the other sites. A tumor marker study revealed an alpha-fetoprotein (AFP) level of 1.51 IU/L (0-15 IU/L), a carcinoembryonic antigen (CEA) level of 1.66 ng/mL (0-5 ng/mL), a cancer antigen (CA) 125 level of 4.6 U/mL (0-33 U/mL), and a CA 19-9 level of 8.1 U/mL (0-33 U/mL), all of which were within the normal ranges. A lobectomy of the left upper lung was performed. She received a single regimen chemotherapy with adriamycin three times after surgery. However, the dyspnea was more aggressive with an uncontrolled right pleural effusion. Although she received pleurocentesis every second weeks, the treatment was unsuccessful and she was discharged and later died. She had a past history of a local excision for an egg-sized, painless, movable mass in the right thigh at another hospital, 11 yrs ago. The thigh mass was removed completely by surgery, which was diagnosed as a leiomyoma at that time, and no adjuvant therapy was given.
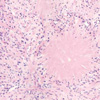
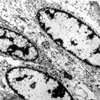
Grossly, the resected lung showed a 4×3×3 cm, well demarcated, pale brown, solid, nodular mass. The tumor had a pushing margin against the surrounding normal tissue. Histologically, the cellularity varied in different areas. In most areas, it was composed of oval to spindle-shaped cells arranged in a variety of patterns and deposited in a densely hyalinized stroma with a paucity of tumor cells punctuated by large collagen rosettes (Fig. 2). The tumor cells had irregular wavy nuclei with a moderate degree of nuclear atypia. There were 1-2 mitoses per high-power field in the more cellular areas. Areas of moderate hypercellularity, nuclear enlargement, and hyperchromatism were found (Fig. 3). The rosettes were clustered together and composed of a central core of brightly eosinophilic collagen, which was arranged centrifugally from the center surrounded by round to ovoid cells (Fig. 4). The microscopic slides of the thigh tumor, which had been resected 11 yrs prior, were reviewed (Fig. 5). The histologic features of the thigh tumor was similar to those of the lung tumor, but exhibited less cellular, and showed vague nodular patterns. There were areas of a moderate degree of cytologic atypia, and abnormal mitoses were also found. However, a few collagenous rosettes-like structures were noted. Occasional cells showed intranuclear cytoplasmic inclusions. Immunohistochemical staining showed that the tumor cells, both spindle-shaped cells and cells that formed the rosettes, were positive for vimentin, S-100 protein, and neuron-specific enolase, but negative for synaptophysin, GFAP, and smooth muscle actin. CD34 was positive in the cells comprising the rosettes, but negative in the spindle-shaped cells. Electron microscopy revealed that the cytoplasm of the tumor cells contained intermediate filaments and often markedly dilated rough endoplasmic reticula (Fig. 6). The cells were surrounded by an abundant extracellular matrix consisting of banded collagen fibers. The center of the rosettes-like structures was composed of banded collagen fibers and the cells at the periphery of the rosettes showed ultrastructural features similar to the neoplastic spindle cells located elsewhere in the tumor.
The HSCTGR was first reported in a series of 19 cases culled from a large soft tissue consultation service by Lane et al. in 1997 (1). Clinically, HSCTGR can develop at almost any age (average age, 38 yr) in the deep soft tissues of the extremities, particularly the thigh (1, 6). Other sites of involvement are the chest wall, the axilla, the buttock, and the neck (1). The most common symptom is a painless, deep-seated, slowly enlarging mass (1, 6). Grossly, the tumor is an oval, multilobulated mass, ranging from 5 to 10 cm in the greatest diameter. The lesion is well circumscribed and surrounded by a thin, fibrous pseudocapsule (6). The cut surface has a whorled white-tan appearance. Despite the gross circumscription, most tumors extensively infiltrate the surrounding soft tissues (6). Histologically, the tumor cells have a deceptively bland appearance, consisting of short, ill-defined fascicles of fusiform to spindled cells with minimal atypia and barely perceptible levels of mitotic activity (6). In a small number of cases there may be foci that are more cellular and atypical, which would mimic an intermediate grade fibrosarcoma (6, 7). Although the cytologic features were usually bland, significant cytologic atypia and mitoses were observed in the primary tumor of our patient. In some areas, hypercellularity and nuclear enlargement and hyperchromatism were identified in both the primary thigh and metastatic lung tumors. The mitotic figures were difficult to identify, usually with fewer than one mitosis per 50 high-power fields (6), but the mitotic rate ranged from 0 and 20 mitotic figures per 10 high-power fields in both tumors of the current case. The most characteristic feature was the presence of a variable number of large rosetteslike structures. These structures either occupy only a small portion of the lesion or are so prominent as to obscure the other features of the neoplasm (1, 6). The rosettes, which tended to cluster, were made up of a central collagenous core flanked by an irregular rim of rounded neoplastic cells. These rounded neoplastic cells had a different immunophenotype compared to the spindled neoplastic cells (8). The spindled cells expressed vimentin only, but the cells comprising the collagen rosettes expressed S-100 protein, leu 7, NSE (6, 8), and occasionally CD34 at various levels (8). The spindle-shaped cells were tested negative to CD34. Despite this unusual phenotype they had the ultrastructural features of fibroblasts (8). Electron microscopy revealed that the cytoplasm contained intermediate filaments and numerous, often markedly dilated rough endoplasmic reticula (8). An abundant extracellular matrix consisting of banded collagen fibers surrounded the cells. The center of the rosettes-like structures was composed of banded collagen fibers and the cells at the periphery of the rosettes had ultrastructural features that were similar to the neoplastic spindle cells located elsewhere in the tumor.
The significance of the rosettes is unclear. However, cells forming rosettes have the ultrastructural features of fibroblasts (8-10). Moreover, they appear to be part of the neoplasm rather than a necrobiotic granuloma-like response within the tumor (8). Similar appearing giant collagen-containing rosettes may be seen in other mesenchymal tumors, including a neuroblastoma-like neurilemmoma, in which the rosettes are comprised of a core of collagen flanked by small, round, differentiated Schwann cells (8, 10).
In the original report by Lane et al., follow-up information was available for 12 of the 19 patients, with a mean follow-up period of 39 months (1). Of the 12 patients, 7 were treated with a simple local excision and 5 by a wide excision. Although one of the patients treated by simple excision developed a local recurrence 20 months after the initial surgery, none of the remaining patients had a recurrent or metastatic disease within the follow-up period. Therefore, this lesion was considered to be a low-grade sarcoma, and a wide surgical excision is the treatment of choice (1, 2). The tumor closely resembled the lesions described by Evans as a "low grade fibromyxoid sarcoma" (1, 2). Based on the histological findings between a low grade fibromyxoid sarcoma and a hyalinizing spindle cell tumor, these lesions were quite similar, if not identical, the latter characterized by the presence of the distinctive rosettes (2). Folpe et al. (7) reported only three metastatic lesions out of 73 cases of low grade fibromyxoid sarcoma and HSCTGR, giving an overall metastatic rate of 5.7%. However, they reported that a small subset of both tumors displayed areas of increased cellularity and atypia which qualify as intermediate- to high-grade sarcoma (7). A significant number of low grade fibromyxoid sarcomas possess inconspicuous collagen rosettes, which are characteristic of HSCTGR, indicating that these two tumors represent the ends of a common spectrum rather than distinct entities (7). Recently, Woodruff et al. reported a case of HSCTGR with pulmonary metastasis following a 4-yr hiatus (3), and this paper reports a similar case following an 11-yr interval. Farinha et al. (11) reported a patient with prolonged survival following the detection of pulmonary metastases from an 11 cm thigh mass. In addition, there was another case of a primary hyalinizing spindle cell tumor of the lung reported (5). However, without complete clinical information it is difficult to exclude the possibility that this represents a pulmonary metastasis from an unknown primary tumor of soft tissue (4). Since the follow-up information in these cases is limited, their long-term behavior has not been demonstrated (4). There have been no other cases of this neoplasm reported in Korea.
The differential diagnosis of HSCTGR includes fibromatosis and fibrosarcoma (7). Fibromatosis is composed of well-formed long fascicles, which are distinct from the irregular fascicles observed in our case. It does not contain an appreciable myxoid or collagenous component. Although the majority of conventional fibrosarcomas have a greater level of cellularity and mitotic activity than a HSCTGR, there is some overlap between fibrosarcoma and a low grade fibromyxoid sarcoma with extensive hyalinization.
In conlusion, we report the first case of HSCTGR with pulmonary metastasis in Korea, and suggest that HSCTGR is a malignant neoplasm with the capacity to metastasize after a long hiatus. Therefore, an accurate tissue diagnosis with wide surgical excision and a close follow-up are essential.
Figures and Tables
Fig. 1
Computerized tomography of the chest reveals bilateral multiple pulmonary nodules with right massive pleurisy causing collpase of the right lung.
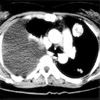
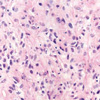
Fig. 2
A fibrous area composed of bland-looking spindle-shaped cells with a fascicular and vague storiform growth pattern. Several rosette-like structures are separated by spindle areas (H&E, ×40).
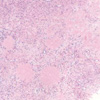
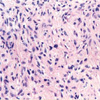
Fig. 3
The tumor cells in the more cellular areas shows irregular wavy nuclei with a moderate degree of nuclear atypia (H&E, ×200).
References
1. Lane KL, Shannon RJ, Weiss SW. Hyalinizing spindle cell tumor with giant rosettes. A distinctive tumor closely resembling low-grade fibromyxoid sarcoma. Am J Surg Pathol. 1997. 21:1481–1488.
2. Evans HL. Low grade fibromyxoid sarcoma. A report of 12 cases. Am J Surg Pathol. 1993. 17:595–600.
3. Woodruff JM, Antonescu CR, Erlandson RA, Boland PJ. Low grade fibrosarcoma with palisaded granuloma-like bodies (giant rosettes). Report of a case that metastasized. Am J Surg Pathol. 1999. 23:1423–1428.
4. O'Sullivan MJ, Sirgi KE, Dehner LP. Low-grade fibrosarcoma (hyalinizing spindle cell tumor with giant rosettes) with pulmonary metastases at presentation: case report and review of the literature. Int J Surg Pathol. 2002. 10:211–216.
5. Magro G, Fraggetta F, Manusia M, Mingrino A. Hyalinizing spindle cell tumor with giant rosettes. A previously undescribed lesion of the lung. Am J Surg Pathol. 1998. 22:1431–1433.

6. Weiss SW, Goldblum JR. Enzinger and Weiss's soft tissue tumors. 2001. 4th ed. St. Louis: Mosby;431–435.
7. Folpe AL, Lane KL, Paull G, Weiss SW. Low-grade fibromyxoid sarcoma and hyalinizing spindle cell tumor with giant rosettes. Am J Surg Pathol. 2000. 24:1353–1360.

8. Nielsen GP, Selig MK, O'Connell JX, Keel SB, Dickersin GR, Rosenberg AE. Hyalinizing spindle cell tumor with giant rosettes. A report of three cases with ultrastructural analysis. Am J Surg Pathol. 1999. 23:1227–1232.
9. Scolyer RA, McCarthy SW, Wills EJ, Palmer AA. Hyalinising spindle cell tumor with giant rosettes: report of a case with unusual features including original histological and ultrastructural observations. Pathology. 2001. 33:101–107.
10. Ludvikova M, Michal M, Zamecnik M. Hyalinizing spindle cell tumors with giant rosette-like structures. Pathol Res Pract. 1998. 194:577–581.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download