Abstract
Both acquired bilateral nevus of Ota-like macules (ABNOM) and nevus of Ota are characterized by the presence of dermal melanocytes. There are no differences in the method of treatment, however, postinflammatory hyperpigmentation (PIH) develops more often in ABNOM than in nevus of Ota following treatment. We investigated the differences in the development of PIH after treatment between ABNOM and nevus of Ota, and the histopathologic differences in the PIH. A total of 82 patients with ABNOM (n=47) and nevus of Ota (n=35) were treated with Q-switched alexandrite laser and followed up 2 weeks and 3 months later. Biopsies were performed on lesional skin before treatment. The distribution and the amount of melanin pigments were visualized with Fontana-Masson stain, and the distribution and the depth of melanocytes were measured by GP-100 (NK1-beteb) stain. Clinically, there was more erythema and PIH in ABNOM than in nevus of Ota. Histopathologically, intradermal melanocytes were clustered in groups and dispersed perivascularly in ABNOM, while melanocytes were scattered evenly throughout the dermis in nevus of Ota. Both groups show that when there is a statistically significant number of melanocytes in the perivascular area, erythema and PIH occur after laser therapy. In conclusion, indirect vessel injury in addition to perivascular clustering melanocytes might be considered the cause of increased PIH after treatment in ABNOM.
Dermal melanocytosis include the mongolian spot, blue nevus, nevus of Ota, nevus of Ito, and acquired bilateral nevus of Ota-like macules (ABNOM). Among these, nevus of Ota and ABNOM are clinically similar and both diseases cause aesthetic problems as they develop on the face and are not self-limited. Nevus of Ota is mostly unilateral and located around the oral mucosa and mucous of the eye. ABNOM is characterized by its bilateral manifestation on the forehead, temples, eyelids, cheeks, and/or nose (1). While the age of onset of nevus of Ota is young, ABNOM is known to develop after 15 yr of age (mean age: 36) in about 94% of the cases.
For the treatment of dermal pigmentation, topical depigmentary agents and chemical peels fail to achieve a significant degree of lightening. Dermabrasion results in an excellent outcome, but it is invasive with a potential risk of scarring (2). The development of lasers revolutionized the treatment of dermal melanocytic lesions with their theory of selective photothermolysis (3). Q-switched (QS) lasers including QS ruby, QS alexandrite, and QS Nd:YAG lasers have been effective in the treatment of nevus of Ota and ABNOM (4-9). However, the treatment of ABNOM is more difficult than that of nevus of Ota. It has been reported that postinflammatory hyperpigmention (PIH) occurred after treatment in 16-50% of patients with nevus of Ota (4, 6, 10-13), and in 50-73% of patients with ABNOM (7, 9, 14). Although the mechanism of the development of PIH is unknown, it was reported to be associated with the severity of inflammation, individual chromotic tendency, and the color of each individual (15).
After the treatment of ABNOM with the Q-switched Nd-YAG laser, a series of changes are observed in the skin. Erythema increases for up to four weeks after treatment and then starts to decrease, while angiogenesis increases for up to 2-3 weeks after treatment and then becomes normalized (19). Angiogenesis is thought to be involved in various inflammatory responses during the wound healing stage, and a group of authors deal with angiogenesis and erythema in the same context (17). Looking at the relationship between ultraviolet B (UVB)-induced inflammation and hyperpigmentation, it was shown that the relationship between the two indices, erythema and melanin, was linear. Therefore, clinical manifestation of erythema may be a sign of active inflammation and thus, there may be a correlation between the degree of erythema after laser treatment and the severity of PIH. We intended to find out if the laser therapy was effective on ABNOM and nevus of Ota, and to also see if the difference in histologic findings was related to post-therapeutic PIH by comparing the two histologic findings.
A total of 82 patients who visited Ajou University Medical Center from January 1998 to March 2003, with clinically and histopathologically proven ABNOM (n=47) and nevus of Ota (n=35) were adopted for this study. The age of the patients ranged from 4 to 63 yr (mean age; ABNOM=41.5 yr, nevus of Ota=35.5 yr). The mean duration of disease is 8.7 yr for ABNOM and 13 yr for nevus of Ota. Skin phototypes IV (ABNOM=10, nevus of Ota=3) and V (ABNOM=37, nevus of Ota=32) were represented. The sex ratio (M:F) is 1:46 in ABNOM and 4:31 in nevus of Ota. The patients have no history of previous treatment. We used a Q-switched alexandrite laser specified with 100 nsec pulse length, emitting at 755 nm and with a 3 mm diameter spot-size (Tattoo laser®, Candela Laser Co., Wayland, MA, U.S.A.). The lesional skin was irradiated with fluences of 7.5 J/cm2. All 82 patients were followed up at 2 weeks and 3 months after treatment, respectively.
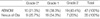
Histopathologic examination was performed in all of the patients. Tissue specimens were obtained by 2 mm punch biopsies from the lesional skin and the perilesional normal skin before Q-switched alexandrite laser treatment. The specimens were fixed in 4% buffered formaldehyde, embedded in paraffin sectioned, and stained with hematoxylin and eosin for light microscope examination. Melanin pigments were visualized with the Fontana-Masson stain, and melanocytes were detected by the GP-100 (NK1-beteb) stain. The results of the Fontana-Masson stain and GP-100 stain were observed by light microscope. In order to see the differences in distribution of melanocytes in the diseases, the following scoring methods were applied: 0, melanocytes are interspersed only between dermal collagenous fibril; 1, melanocytes are distributed around collagenous fibril and the perivascular region; 2, melanocytes are distributed mainly around the perivascular region. The depth was assessed by measuring from the top of the granular layer of the epidermis to the deepest dermal melanocytes.
Thirty specimens (15 specimens of ABNOM, 15 specimens of nevus of Ota) were chosen. The number of melanocytes as well as the amount of melanin pigment per unit area in the epidermis and dermis of both normal and lesional skin were evaluated using pigment image analysis. For the measurement of melanin pigment, the image of pigment in a certain area of the epidermis and dermis was analyzed on Fontana-Masson stain at 100 times magnification. The amount of melanin was then divided by the area, "the amount of melanin per unit area (Melanin Index; MI)". To measure the number of melanocytes, the number of melanocytes in a certain area of the epidermis and dermis was measured on GP-100 stain at 100 times magnification, and this number was divided by the area (Number of melanocyte/mm2, Mel/mm2). The differences in the number of melanocytes per unit among each cluster were evaluated (Fig. 1).
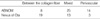
The responses to laser treatment were objectively assessed by two independent observers using side-by-side comparisons of clinical photographs taken before the first laser treatment and 2 weeks and 3 months after the laser treatment for all of the patients using a Nikon FM camera, ASA 100 negative film, and a standard flash. All the films were processed by the same laboratory. A visual analog scale of both erythema and PIH consisted of three levels. Erythema was scored by the redness in the laser-treated area on the clinical photographs taken before the first laser treatment and those taken after 2 weeks. The erythema was graded as grade 0 (no redness), grade 1 (mild redness), and grade 2 (moderate to severe redness). PIH was scored by the hyperpigmentation on the clinical photographs taken before the first laser treatment and after 3 months. The PIH was graded as grade 0 (no hyperpigmentation), grade 1 (mild hyperpigmentation), and grade 2 (moderate to severe hyperpigmentation).
Statistical analysis was performed with SPSS (Statistical Package for Social Science, SPSS V10.0 Inc.) software on PC. The data of individual groups were evaluated with the linear regression conducted or paired t test; a p value of less than 0.05 indicated a statistically significant value.
In ABNOM, there were elongated, slender pigment-bearing cells dispersed in the upper dermis (Fig. 2). Melanocytes were distributed more frequently in the perivascular area (Table 1). However, in nevus of Ota, pigment-bearing cells were numerous and distributed diffusely throughout the upper and lower dermis. There were elongated, slender pigment-bearing cells dispersed in between the collagen fibers of the dermis, and the long axis of pigment-bearing cells were along the collagen fibers (Fig. 3). Melanocytes were diffusely distributed in the dermis rather than in the perivascular area (Table 1).
The epidermis was normal and there was no differences in the number of melanocytes or in the degree of melanin pigment between ABNOM and nevus of Ota.
In the dermis, the number of melanocytes per unit area in nevus of Ota increased up to 4.75 times more than ABNOM. Melanin pigment in nevus of Ota increased up to 2.27 times that of ABNOM (Fig. 4).
After treatment, there was erythema in 37 patients (78.72%) with ABNOM and in 26 patients (74.28%) with nevus of Ota. In terms of the degree of erythema, the incidence of mild erythema was 48.6% for ABNOM and 73.1% for nevus of Ota, and the incidence of moderate or worse erythema was 51.4% for ABNOM and 26.9% for nevus of Ota (Table 2). There was no significant difference in the incidental rate between the two group of disorders, but as far as the grade of erythema is concerned, more intense erythema developed in patients with ABNOM than in patients with nevus of Ota. PIH developed in 30 patients with ABNOM (63.8%) and 11 patients with nevus of Ota (31.4%). The incidence of PIH was significantly higher in ABNOM than in nevus of Ota (p value<0.0001). In terms of the degree of pigmentation, 15 out of 30 patients with ABNOM (50%) showed mild pigmentation and 15 (50%) patients showed moderate to severe pigmentation. In contrast, all of the 11 patients with nevus of Ota showed mild pigmentation and none showed moderate to severe grade pigmentation (Table 3). The development of erythema or pigmentation had no statistically significant relationship with the age of onset, duration of disease, or skin type. However, there was a statistically significant relationship between the development of erythema and pigmentation. Erythema and pigmentation show a correlation slope of 0.64 in ABNOM and 0.52 in nevus of Ota, demonstrating that when there is severe erythema, there is severe pigmentation. The slope difference between the two disorders show that for a similar level of erythema, ABNOM appears to have a more severe pigmentation outcome than that of nevus of Ota. Both group of diseases show that when there is statistically significant number of melanocytes in the perivascular area, erythema and PIH occur immensely after laser therapy (Table 4).
PIH is a frequently encountered problem and represents the sequelae of various cutaneous disorders and therapeutic interventions including laser treatment. QS laser systems such as QS ruby (4), QS alexandrite, and QS Nd:YAG (5, 6) can now be used to completely clear dermal melanocytic lesions including ABNOM and nevus of Ota. However, such laser therapy can induce PIH. Clinically, while the patients with the nevus of Ota were comparatively satisfied with the therapy, ABNOM patients were less satisfied because the hyperpigmentation led to more cosmetic problems than had existed before the therapy. Several causes for the increased prevalence of PIH in ABNOM after laser treatment are considered. First, though the exact etiology of ABNOM is yet to be found, several hypotheses have been postulated to explain the pathogenesis. It may be attributed to the dropping off of epidermal melanocytes, or to the manifestation of latent dermal melanocytosis in some areas of the face, that are triggered by extrinsic stimulants such as hormones, sunlight, trauma, etc (1). But melanocytes of nevus of Ota are of neuroectodermal origin. During the early phases of embryonic life the cutis contains numerous melanocytes, that gradually diminish (in number or melanogenic activity or both) during fetal life. A plausible explanation for the occurrence of nevus of Ota is that it develops due to the failure of dermal melanocytes. In ABNOM, melanocytes develop due to extrinsic stimulants such as hormone, UV light, trauma, laser therapy, and the stimuli may induce even more pigmentation after the inflammatory reaction. However, such differences in pathogenesis alone do not explain well the differences in PIH that occur after laser therapy. Therefore, the differences in histopathologic findings were evaluated in this study.
Second, in the treatment of QSAL, melanin acts as a chromophore, therefore melanin in the epidermis allows laser to be selectively absorbed so that the epidermal tissue becomes vacuolized due to the heat. The melanocytes and melanin pigment of the vacuolated epidermis are dropped into the dermis, and are presumed to induce PIH. When there is a lot of epidermal melanin, heat has an effect mainly on the epidermis. Therefore, when there exists an abundance of melanin in the epidermis, PIH after laser is apt to occur more commonly (19). To see if this mechanism shows a big difference between the two diseases, epidermal melanocytes and melanin pigment were measured. However, there was no difference in the number of melanocytes and in the degree of melanin pigment between the diseases. Hence, the differences in the epidermis between ABNOM and nevus of Ota seem to have no relationship with PIH after laser treatment. This is probably because the laser wavelength does not have a significant effect on the epidermis but does on the dermis. Also, clinically the skin phototype did not affect the PIH. The reason why skin phototype was of no concern was because most of the patients' skin phototypes were limited to IV or V, thus showing a similar tendency.
Last, melanocytes were located in the superficial dermis in ABNOM rather than in nevus of Ota. In ABNOM, elongated, slender pigment-bearing cells were distributed more frequently in the perivascular area. Nevus of Ota had pigment-bearing melanocytes in between collagen fibers throughout the dermal layer evenly distributed. Melanin-laden dermal cells function as chromophores, therefore the postulated mechanism of injury to melanized cells is a photothermal and photoacoustic effect that results in shock waves or cavitation and resulting in secondary alteration in cellular organelles. Therefore, the energy exposure may directly stimulate melanocytes and indirectly cause vascular injury due to pressure waves generated by the interaction of the laser with melanin-laden dermal cells near blood vessels. Indirect vascular injury induces an inflammatory response, releasing proinflammatory cytokines such as interleukin-1, TNF-α etc. (16). These chemical mediators are capable of altering the pigmentary and the inflammatory responses simultaneously. Takiwaki H et al. (17) investigated the relationship between UVB-induced erythema and subsequent pigmentation quantitatively. The relationship between the two indices was linear in each subject, and the correlation coefficient was 0.83 when evaluated using the data. Both erythema and hyperpigmentation were suppressed significantly in a parallel manner by corticosteroids and indomethacin applied topically immediately after UVB irradiation. These results imply that PIH correlates closely with the severity of prior inflammation and that chemical mediators released in the inflammatory process have considerable influence on melanogenesis (18). Also, following laser treatment, erythema increases up to 4 weeks after treatment and then starts to decrease while angiogenesis increases up to 2 to 3 weeks after treatment and then normalizes. This means erythema reflects angiogenesis. Angiogenesis is thought to be involved in various inflammatory responses during wound healing and a group of authors deal with angiogenesis and erythema in the same context (17). This implies that a more severe inflammatory response occurred in ABNOM than in nevus of Ota because the degree of erythema is more severe in ABNOM. Therefore, one can presume that PIH occurred more as well. Clinical manifestations were checked to see if erythema and pigmentation were more significant in ABNOM. Compared to nevus of Ota, ABNOM developed erythema in a similar fashion, but the degree of erythema was much more severe. Also erythema of the same degree was shown to cause much more hyperpigmentation. PIH occurred in ABNOM twice as much as in nevus of Ota.
In summary, after laser treatment, ABNOM showed a higher degree of erythema as well as a higher incidence and degree of PIH compared to that of nevus of Ota. Histopathologically, the lesion in ABNOM was located in the superficial dermal layer and there were few epidermal melanocytes and melanin pigment. Melanocytes were especially clustered in the perivascular area in ABNOM, whereas melanocytes were evenly distributed throughout the dermal layer in nevus of Ota. From the above results, epidermal melanocytes and melanin pigment are not associated with PIH in these two diseases. The presence of many melanocytes in the perivascular area may lead to indirect vascular damage, thus increasing melanogenesis which is also induced by many types of inflammatory responses and chemical substances. More detailed studies of the correlation between vascular injury, inflammatory mediator, and PIH are necessary.
Figures and Tables
Fig. 1
An example of the image analysis method of the histopathologic findings. Green lines (A, B) indicate the border of the fixed area, (A) red spots indicate melanin pigment in the epidermis and (B) red spots indicate melanin pigment in the dermis.

Fig. 2
Light microscopic findings of ABNOM (A) GP-100 stain ×200, (B) Fontana-Masson stain ×200. It shows that pigment bearing melanocytes are scattered in the perivascular area in ABNOM. There are elongated pigment-bearing melanocytes scattered in the upper dermis and some dispersed in the perivascular area.

Fig. 3
Light microscopic findings of nevus of Ota. (A) GP-100 stain ×200, (B) Fontana-Masson stain ×200. Melanocytes were numerous and distributed diffusely throughout the upper and lower dermis. There were elongated, slender melanocytes dispersed between the collagen fibers of the dermis, the long axis of the melanocyte was along the collagen fibers.

Fig. 4
Comparison of the number of melanocytes and degree of melanin pigment in ABNOM and nevus of Ota. We compared the number of melanocytes in the dermis of ABNOM with that of nevus of Ota and the number of melanocytes in nevus of Ota is 4.75 times greater than in ABNOM (p<0.01). The degree of melanin pigment in the dermis of nevus of Ota is 2.27 times greater than in ABNOM (p<0.01).
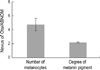
Table 2
The distribution in the grade of erythema in ABNOM and nevus of Ota after two weeks of QSAL treatment
References
1. Hori Y, Kawashima M, Oohara K, Kukita A. Acquired, bilateral nevus of Ota-like macules. J Am Acad Dermatol. 1984. 10:961–964.

2. Kunachak S, Kunachakr S, Sirikulchayanonta V, Leelaudomlipi P. Dermabrasion is an effective treatment for acquired bilateral nevus of Ota-like macules. Dermatol Surg. 1996. 22:559–562.

3. Anderson RR, Parrish JA. Selective photothermolysis precise microsurgery by selective absorption of pulsed radiation. Science. 1983. 220:524–527.

5. Chan HH, King WW, Chan ES, Mok CO, Ho WS, Van Krevel C, Lau WY. In vivo trial comparing patients' tolerance of Q-switched Alexandrite and Q-switched Neodymium: Yttrium-aluminum-Garnet lasers in the treatment of nevus of Ota. Lasers Surg Med. 1999. 24:24–28.
6. Chan HH, Ying SY, Ho WS, Kono T, King WW. An in vivo trial comparing the clinical efficacy and complications of Q-switched 755 nm alexandrite and Q-switched 1064 nm Nd:YAG lasers in the treatment of nevus of Ota. Dermatol Surg. 2000. 26:919–922.

7. Kunachak S, Leelaudomlipi P, Sirikulchayanonta V. Q-switched ruby laser therapy of acquired bilateral nevus of Ota-like macules. Dermatol Surg. 1999. 25:938–941.

8. Kunachak S, Leelaudomlipi P. Q-switched Nd:YAG laser treatment for acquired bilateral nevus of Ota-like maculae: a long-term follow-up. Lasers Surg Med. 2000. 26:376–379.

9. Polnikorn N, Tanrattanakorn S, Goldberg DJ. Treatment of Hori's nevus with the Q-switched Nd:YAG laser. Dermatol Surg. 2000. 26:477–480.

10. Kang W, Lee E, Choi GS. Treatment of Ota's nevus by Q-switched alexandrite laser: therapeutic outcome in relation to clinical and histopathological findings. Eur J Dermatol. 1999. 9:639–643.
11. Watanabe S, Takahashi H. Treatment of nevus of Ota with the Q-switched ruby laser. N Engl J Med. 1994. 331:1745–1750.

12. Kono T, Nozaki M, Chan HH, Mikashima Y. A retrospective study looking at the long-term complications of Q-switched ruby laser in the treatment of nevus of Ota. Lasers Surg Med. 2001. 29:156–159.

13. Suh DH, Hwang JH, Lee HS, Youn JI, Kim PM. Clinical features of Ota's naevus in Koreans and its treatment with Q-switched alexandrite laser. Clin Exp Dermatol. 2000. 25:269–273.

14. Lam AY, Wong DS, Lam LK, Ho WS, Chan HH. A retrospective study on the efficacy and complications of Q-switched alexandrite laser in the treatment of acquired bilateral nevus of Ota-like macules. Dermatol Surg. 2001. 27:937–941.

15. Ruiz-Maldonado R, Orozco-Covarrubias ML. Postinflammatory hypopigmentation and hyperpigmentation. Semin Cutan Med Surg. 1997. 16:36–43.

16. Kim SD, Kim SW, Huh CH, Suh DH, Eun HC. Changes of biophysical properties of the skin measured by non-invasive techniques after Q-switched Nd-YAG laser therapy in patients with nevus of Ota. Skin Res Technol. 2001. 7:262–271.

17. Takiwaki H, Shirai S, Kohno H, Soh H, Arase S. The degrees of UVB-induced erythema and pigmentation correlate linearly and are reduced in a parallel manner by topical anti-inflammatory agents. J Invest Dermatol. 1994. 103:642–646.

18. Lu Z, Chen J, Wang X, Fang L, Jiao S, Huang W. Effect of Q-switched alexandrite laser irradiation on dermal melanocytes of nevus of Ota. Chin Med J (Engl). 2000. 113:49–52.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download