Abstract
Homing-associated cell adhesion molecules (H-CAM) on the CD34+ cells play an important role for the engraftment process following hematopoietic stem cell transplantation (HSCT). However, it seems that not only CD34+ cells but also other nucleated cells (NCs) with H-CAM could be implicated in the engraftment process and the proliferation of hematopoietic stem cells. We investigated the differences of H-CAM and cell cycle status on the NCs in cord blood (CB), bone marrow (BM), and mobilized peripheral blood (PB). The proportions of CXCR4+ cells within the NC populations were greater in CB than in PB or BM (p=0.0493), although the proportions of CXCR4+, CD44+, and CD49d+ cells within the CB CD34+ cell populations were same within BM or PB. A lower proportion of CD34+CD49d+ cells within the CD34+ cell populations was more noted in CB than in PB or BM (p=0.0085). There were no differences in cell cycle status between CB and BM or PB. Our results suggest that the migrating potential of CB would be enhanced with increased CXCR4 expression on the NCs, but the adhesion potential of CB CD34+ cells would be less than that of PB and BM. These findings may help explain why the lower cell dose is required and engraftment is delayed in cord blood stem cell transplantation.
Cord blood (CB) stem cells are increasingly being used as a source of hematopoietic stem cells transplantation (HSCT). Although there are several advantages, such as a lower incidence of graft-versus-host disease (GVHD) or viral infections in cord blood stem cell transplantation (CBSCT) as compared to bone marrow transplantation (BMT), slower engraftment speed and the limitation of the cell dose are still obstacles (1-5). Recent studies regarding the homing mechanism following HSCT have revealed that homing-associated cell adhesion molecules (H-CAMs) and chemokine receptors on the CD34+ cells play very important roles for engraftment (6, 7). Until recently, most studies on H-CAMs have been commonly performed by using purified CD34+ cells, and the quantity of these cells is expressed as percentages of positive cells or as the antigen density on the CD34+ cells (8-11).
Although most of the CAMs including CD49d, CD44 and CXCR4, are present on primitive hematopoietic cells, they are also found on another nucleated cells (NCs) including monocytes and lymphocytes (12-15). Therefore, not only CD34+ cells but also the other NCs expressing H-CAMs and chemokine receptors could be implicated in the engraftment and proliferation of hematopoietic stem cells. Furthermore, in CBSCT, the speed of myeloid engraftment was primarily associated with the total nucleated cell (TNC) counts rather than the CD34+ cell counts (2).
Although recent study revealed that trafficking of transplanted cells to the bone marrow is not selective and lodgment of bone marrow-homed cells may be specific (16), engraftment potential of HSCs may be influenced by the distinct phases of cell cycle (17, 18).
A lot of studies showed a significant delay of neutrophil and platelet recovery in the CBSCT group compared with the BMT or peripheral blood stem cell transplantation (PBSCT) groups. The studies have also revealed that the median cell doses for engraftment are significantly lower in the CBSCT group compared with the BMT or PBSCT groups (2, 5, 19, 20). However, to date it is not clear why the engraftment speed is different and the required cell dose for engraftment is different among these groups. In the present study, to determine the engraftment kinetics, we investigated the differences of H-CAMs and chemokine receptors as well as cell cycle status by using the NCs, not the purified CD34+ cells, in the bone marrow (BM), mobilized peripheral blood (PB) and the CB.
Eight BM samples were obtained from normal healthy donor for related BMT, and these cells were cryopreserved after a red cell depletion process by density gradient separtion with 10% pentastarch (Jeil Pharm, Seoul, Korea), and the cells were then analysed after thawing. Ten PB samples were obtained from the apheresed products of acute myelogenous leukemia patients, which were collected after mobilization chemotherapy for the PBSC harvest.
Thirteen CB samples were collected into transfer bags containing acid citrate dextrose (ACD) from the umbilical cord vein immediately after a full-term vaginal delivery, and the red cells were depleted by the same method as was used with the BM.
Dual-color flow cytometry of CD34/CXCR4, CD34/49d, CD34/44 for the isolated nucleated cells was performed using FACSort (Becton Dickinson, San Jose, CA, U.S.A.). The cells were stained with the corresponding monoclonal antibodies for 45 min. After incubation, the cells were then washed three times in phosphate-buffered saline (PBS), fixed in 1% paraformaldehyde, and finally analysed by using Lysys II software (Becton Dickinson, San Jose, CA, U.S.A.).
The cells were washed two times with PBS by centrifugation for 3 min at 4℃, then they were fixed with 50% ethanol for 30 min at room temperature. Cells were suspended in PBS containing RNase (1 mg/mL, 20 µL) and propidium iodide (10 mg/mL, 2.5 µL), and they were incubated for 30 min at room temperature. The cell cycle was analysed with Multicycle using Coulter EPICS XL flow cytometer (Beckman Coulter, FL, U.S.A.).
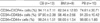
Although the CD34+CXCR4+ and CD34+CD44+ cells within the NC populations in CB were not statistically different from PB or BM, the CD34+CD49d+ cells were significantly lower in CB (0.91±0.49%) than in BM (2.38±1.19%) or PB (4.23±3.14%) (p=0.0085) (Table 2). However, in the CB CD34+ cell populations, the proportions of CD34+CXCR4+, CD34+CD49d+, and CD34+CD44+ cells were not significantly different from BM or PB (Table 3).
Most of NCs of CB (87.83±6.71%), BM (87.62±5.01%), and PB (88.38±32%) were in G0/G1 phase and they were not statistically different. The cell fractions in S/G2/M phase showed no significant differences between those fractions in CB (12.17±6.75%) and BM (12.4±5.07%) or PB (11.6±1.35%) (Fig. 2).
In hematopoietic stem cell transplantations, CB offers substantial advantages when compared to BM or PB. There is the rapid availability of cells and the less stringent requirements for HLA identity between the donor and recipient because of the lower risk of acute and chronic graft versus host disease. The major disadvantage of CBSCT is the delayed recovery of neutrophils and platelets, which could increase the risk of life-threatening infections and bleedings (4, 5). Although the engraftment following CBSCT is strongly correlated with infused nucleated cell numbers (2), very little is known about why the engraftment speed is slower in CBSCT than in BMT or PBSCT.
To rescue the patient's hematopoietic systems after myeloablative chemo- or radiotherapy, the intravenously transplanted hematopoietic stem cells (HSCs) have to migrate to the bone marrow's microenvironment for their ultimate proliferation and differentiation. In this homing process, various adhesion molecules present on both HSC and endothelial cells are involved (6, 7). The CD34+ cells exhibit other adhesion receptors they are involved in the multistep process of HSCT: homing in to the BM, adhesion to the BM microenvironment and finally, the stem cell differentiation. CXCR4 is a dominantly expressed chemokine receptor on primitive human blood cells within all stages of human development (21). Stromal cell-derived factor-1 (SDF-1), which is produced by stromal cells in various organs, is a powerful chemoattractant for its receptor CXCR4. The SDF-1/CXCR-4 interaction is clinically relevant during embryonic development, hematopoiesis and the migration of CD34+ stem cells. We revealed that although the proportions of CD34+CXCR4+ cells within the NC or CD34+ cell populations were not statistically different in BM, PB and CB, the proportions of CXCR4+ cells in NC populations were significantly higher in CB than in BM or PB. These results suggest that NCs, except CD34+ cells expressing CXCR4, were more abundant in CB than in BM or PB.
The integrins, such as VLA-4 or VLA-5, they mediate the adhesion of HSC to extracellular matrix proteins. The mobilization of BM CD34+ cells into the PB is followed by a decrease of VLA-4 and VLA-5 expression (22, 23), and the low frequency of CD49d+ on PB CD34+ cells has been also reported by many authors (24-27). In our study, we observed the same percentage of CD49d+ cells within the CD34+ cell populations in the BM, PB and CB. However, CD34+CD49d+ cells within the NC populations in the CB were significantly lower than in BM or PB.
In conclusion, our results suggest that the migrating potential of CB would be enhanced with increased CXCR4 expression on the NCs. However, the adhesion potential of CB CD34+ cells would be less than that of PB and BM because of the lower expression of CD34+CD49d+ cells within the NC populations. These findings may help explain why the lower CB cell dose is required and engraftment is delayed in CBSCT.
Figures and Tables
 | Fig. 1Representative flow cytometric profile of CXCR4, CD44, CD49d and CD34 expression on the isolated nucleated cells from bone marrow (BM), mobilized peripheral blood (PB) and cord blood (CB). |
 | Fig. 2Representative cell cycle analysis of the isolated nucleated cells from bone marrow (BM), mobilized peripheral blood (PB) and cord blood (CB). |
References
1. Gluckman E, Broxmeyer HA, Auerbach AD, Friedman HS, Douglas GW, Devergie A, Esperou H, Thierry D, Socie G, Lehn P, Cooper S, English D, Kurtzberg J, Bard J, Boyse EA. Hematopoietic reconstitution in a patient with Fanconi's anemia by means of umbilical cord blood from an HLA-identical sibling. N Engl J Med. 1989. 321:1174–1178.
2. Kurtzberg J, Laughlin M, Graham ML, Smith C, Olson JF, Halperin EC, Ciocci G, Carrier C, Stevens CE, Rubinstein P. Placental blood as a source of hematopoietic stem cells for transplantation into unrelated recipients. N Engl J Med. 1996. 335:157–166.

3. Wagner JE, Rosenthal J, Sweetman R, Shu XO, Davies SM, Ramsay NK, McGlave PB, Sender J, Cairo MS. Successful transplantation of HLA-matched and HLA-mismatched umbilical cord blood from unrelated donors: Analysis of engraftment and acute graft versus host disease. Blood. 1996. 88:795–802.
4. Rubinstein P, Carrier C, Scaradavou A, Kurtzberg J, Adamson J, Migliaccio AR, Berkowitz RL, Cabbad M, Dobrila NL, Taylor PE, Rosenfield RE, Stevens CE. Outcomes among 562 recipients of placental blood transplants from unrelated donors. N Engl J Med. 1998. 339:1565–1577.
5. Rocha V, Wagner JE Jr, Sobocinski KA, Klein JP, Zhang MJ, Horowitz MM, Gluckman E. Graft-versus-host disease in children who have received a cord blood or bone marrow transplant from an HLA-identical sibling. Eurocord and International Bone Marrow Transplant Registry Working Committee on Alternative Donor and Stem Cell Sources. N Engl J Med. 2000. 342:1846–1854.
6. Whetton AD, Graham GJ. Homing and mobilization in the stem cell niche. Trends Cell Biol. 1999. 9:233–238.

7. Kronenwett R, Martin S, Haas R. The role of cytokines and adhesion molecules for mobilization of peripheral blood stem cells. Stem Cells. 2000. 18:320–330.

8. Watanabe T, Dave B, Heiman DG, Lethaby E, Kessinger A, Talmadge JE. GM-CSF-mobilized peripheral blood CD34+ cells differ from steady-state bone marrow CD34+ cells in adhesion molecule expression. Bone Marrow Transplant. 1997. 19:1175–1181.

9. Barbosa IL, De Sausa ME, Godinho MI, Teixeira AM, Carvalhais A. Analysis of surface markers on CD34+ cells, isolated from cord blood and G-CSF primed peripheral blood. Bone Marrow Transplant. 1998. 22:S56.
10. Kroger N, Zeller W, Hassan HT, Dierlamm J, Zander AR. Difference between expression of adhesion molecules on CD34+ cells from bone marrow and G-CSF-stimulated peripheral blood. Stem Cells. 1998. 16:49–53.
11. Bellucci R, De Propris MS, Buccisano F, Lisci A, Leone G, Tabilio A, De Fabritiis P. Modulation of VLA-4 and L-selectin expression on normal CD34+ cells during mobilization with G-CSF. Bone Marrow Transplant. 1999. 23:1–8.

12. Voermans C, Van Hennik PB, Van der Schoot CE. Homing of human hematopoietic stem and progenitor cells: New insights, New challenges? J Hematother Stem Cell Res. 2001. 10:725–738.

13. Cavers M, Khoshkbijari BA, Macey M, McCarthy DA, Irshad S, Brown KA. Differential expression of β1 and β2 integrins and L-selectin on CD4+ and CD8+ T lymphocytes in human blood: comparative analysis between isolated cells, whole blood samples and cryopreserved preparations. Clin Exp Immunol. 2002. 127:60–65.

14. Hemler ME. VLA proteins in the integrin family. Structures, functions and their roles on leukocytes. Annu Rev Immunol. 1990. 8:365–400.
15. Kishimoto TK, Larson RS, Corbi AL, Dustin ML, Staunton DE, Springer TA. The leukocyte integrins. Adv Immunol. 1989. 46:149–182.

16. Jetmore A, Plett PA, Tong X, Wolber FM, Breese R, Abonour R, Orschell-Traycoff CM, Srour EF. Homing efficiency, cell cycle kinetics, and survival of quiescent and cycling human CD34+ cells transplanted into conditioned NOD/SCID recipients. Blood. 2002. 99:1585–1593.

17. Nilsson SK, Dooner MS, Quesenberry PJ. Synchronized cell-cycle induction of engrafting long-term repopulating stem cells. Blood. 1997. 90:4646–4650.

18. Gothot A, van der Loo JC, Clapp DW, Srour EF. Cell cycle-related changes in repopulating capacity of human mobilized peripheral blood CD34+ cells in non-obese diabetic/severe combined immunedeficient mice. Blood. 1998. 92:2641–2649.

19. Barker JN, Davies SM, DeFor T, Ramsay NK, Weisdorf DJ, Wagner JE. Survival after transplantation of unrelated donor umbilical cord blood is comparable to that of human leukocyte antigen-matched unrelated donor bone marrow: results of a matched-pair analysis. Blood. 2001. 97:2957–2961.

20. Ooi J, Iseki T, Takahashi S, Tomonari A, Nagayama H, Ishii K, Ito K, Sato H, Takahashi T, Shindo M, Sekine R, Ohno N, Uchimaru K, Nagamura F, Shirafuji N, Tojo A, Tani K, Asano S. A clinical comparison of unrelated cord blood transplantation and unrelated bone marrow transplantation for adult patients with acute leukemia in complete remission. Br J Haematol. 2002. 118:140–143.
21. Rosu-Myles M, Khandaker M, Wu DM, Keeney M, Foley SR, Howson-Jan K, Yee IC, Fellows F, Kelvin D, Bhatia M. Characterization of chemokine receptors expressed in primitive blood cells during human hematopoietic ontogeny. Stem cells. 2000. 18:374–381.

22. To LB, Haylock DN, Simmons PJ, Juttner CA. The biology and clinical uses of blood stem cells. Blood. 1997. 89:2233–2258.

23. Prosper F, Stroncek D, McCarthy JB, Verfaillie CM. Mobilization and homing of peripheral blood progenitors is related to reversible downregulation of α4 β1 integrin expression and function. J Clin Invest. 1998. 101:2456–2467.
24. Mohle R, Moore MA, Nachman RL, Rafii S. Transendothelial migration of CD34+ and mature hematopoietic cells: an in vitro study using a human bone marrow endothelial cell line. Blood. 1997. 89:72–80.
25. Dercksen MW, Gerritsen WR, Rodenhuis S, Dirkson MK, Slaper-Cortenbach IC, Schaasberg WP, Pinedo HM, von dem Borne A, Van der Schoot CE. Expression of adhesion molecules on CD34+ cells: CD34+ L-selectin+ cells predict a rapid platelet recovery after peripheral blood stem cell transplantation. Blood. 1995. 85:3313–3319.

26. Watanabe T, Dave B, Heimann DG, Lethaby E, Kessinger A, Talmadge JE. GM-CSF-mobilized peripheral blood CD34 cells differ from steady state bone marrow CD34 cells in adhesion molecule expression. Bone Marrow Transplant. 1997. 19:1175–1181.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download