Abstract
The aim of this study was to establish a multi-center birth defects monitoring system to evaluate the prevalence and the serial occurrence of birth defects in Korea. Ten medical centers participated in this program. A trained nurse collected relevant records from delivery units and pediatric clinics in participating hospitals on a monthly basis. We observed 1,537 cases of birth defects among 86,622 deliveries, which included live births and stillbirths. The prevalence of birth defects was 1.8%, and the sex distribution of the birth defect cases was 55.2% male and 41.6% female. The highest proportion of birth defects was in the cardiovascular system (17.5%), followed by birth defects involving in the genitourinary system (15.6%). Chromosomal anomalies were detected 30.0 per 10,000 births. Of these chromosomal anomalies, Down syndrome was most frequently observed. This study led to an establishment of a multi-center active monitoring system for birth defects. To better understand the serial occurrence of birth defects in Korea, it is necessary to increase the number of participating hospitals and to launch on a nation-wide multi-center study.
Birth defects are an important contributor to infant mortality among all racial/ethnic groups. Major congenital anomalies are defined as those that threaten life, require major surgery, or lead to a significant disability. Between 2% and 3% of all infants have a major congenital anomaly identified at birth and approximately 6% to 10% of such infants die within the first year of life (1). In more than 60% of such cases, the etiology of the congenital birth defect is unknown and primary prevention is impossible. In approximately 20% of congenital cases, the causes are monogeneous defects, 50% are caused by chromosome aberrations and 20% by virus infections, such as rubella, cytomegalovirus, and herpes virus (2, 3). Many environmental factors have been suspected to play an etiologic role in the formation of congenital anomalies. Chemical pollutants, dietary imbalances, ionizing radiation, pharmaceutical substances, and infections provide examples of known or suspected agents (4). Unlike animal studies, molecular and biochemical studies in pregnant women are impossible. Therefore, epidemiological data about congenital malformations is of vital importance to scientific research on pathomorphogenesis, aimed at prevention and public health education (3).
Currently, no nationwide birth defect monitoring system exists in Korea. Only a small number of reports on birth defect monitoring are available from general hospitals (5-7). Thus, our aim is to establish a multi-center birth defects monitoring system for the evaluation of the prevalence and serial occurrence of birth defects in Korea.
The study materials were all recorded deliveries at 10 medical centers in Korea, between May 1999 and October 2002. The ten medical center were: the Samsung Cheil Hospital, Samsung Medical Center, Asan Medical Center, Cheil Women's Clinic, Ilsan Cheil Hospital, Bombit Women's Hospital, Ewha Women's University Mokdong Hospital, Kangnam St. Mary's Hospital, Sanggye Baik Hospital, and Seoul National University Hospital.
Records were obtained monthly, from delivery units and pediatric clinics by a visiting nurse. Trained staff from each center provided the medical records that included delivery files, stillborn files and newborn files. The entire medical record of each case was reviewed for followings: hospital stay, prenatal diagnostic test results, birth certificate work sheet, labor and delivery records, progress notes, pathology/autopsy findings, physical examination findings, and a discharge summary. The collected database was checked by trained medical doctor monthly.
All live births, stillbirths, and spontaneous abortions after the 16th week of gestation were included. All neonates born at one of the 10 centers were examined by a pediatrician within the first week of life. In addition to the clinical examination, information from the prenatal and postnatal ultrasound examinations of the heart, brain and other organs were recorded. Chromosome analysis was available for a number of birth defects that were coded according to the EUROCAT (European Registration of Congenital Anomalies and Twins, an European Union Registry) (4) and the International Clearing-house for Birth Defects Monitoring System (ICBDMS) (8).
The nineteen groups of malformations as described by the ICBDMS (8) were 1) anencephaly, 2) spina bifida, 3) encephalocele, 4) hydrocephaly, 5) microtia, 6) cleft palate, 7) total cleft lip, 8) esophageal atresia or stenosis, 9) anorectal atresia or stenosis, 10) hypospadias, 11) renal agenesis/dysgenesis, 12) limb reduction defects, 13) omphalocele, 14) gastroschisis, 15) abdominal wall defects, 16) diaphragmatic hernia, 17) transposition of the great vessels, 18) hypoplastic left heart syndrome, and 19) Down syndrome.
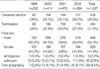
During the 4-yr period (May 1999-October 2002), we observed 1,537 cases of birth defects among 86,622 births, including live births and stillbirths, the prevalence rate being 1.8%. The mean maternal age was 29.9 (±4.1, 95% CI) yr, with a range 19-45 yr. Nineteen percent (291 cases) of the birth defects were associated with an elderly mother (≥35 yr). Primipara birth and multipara birth accounted for 55.1% and 44.9%, respectively. Table 1 shows the changes in the prevalence of birth defects over time.
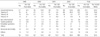
The general characteristics of the birth defects are summarized in Table 2. The mean gestational age at delivery was 32.5±8.6 weeks, ranging from 11 weeks to 43 weeks. The mean birth weight was 2,198±1,319.5 g, with a range from 5 g to 5,060 g. Non-living births (termination or intra-uterine fetal death) accounted for 31.5% of deliveries, and 438 babies (28.5%) were born via Cesarean section. The sex distribution of the birth defect cases was 55.2% male and 41.6% female. Five cases had (0.3%) ambiguous genitalia, and in 45 cases (2.9%), the gender of the fetus could not be determined. Twin pregnancies accounted for 4.5% of cases.
Table 3 shows the comparison of incidences of 19 congenital anomalies in Korea as defined by ICBDMS (5) with those in Japan and China and with Atlanta, U.S.A. as determined by the Metropolitan Atlanta Congenital Defects Program (MACDP) (9).
Among 1,537 birth defect cases, 260 cases (16.9%) had chromosomal abnormalities (Table 4). Among these, Down syndrome was most common (137 cases), followed by Edwards syndrome (57 cases).
Table 5 shows the birth defects according to the involved organs. The highest proportion of birth defects (17.5%) involved the cardiovascular system, followed by the genitourinary system (15.6%). Multiple anomalies accounted for 16% of all birth defect cases.
Thirty-four cases had polydactyly of the hand (4.0 per 10,000 fetuses) and 20 cases had polydactyly of the foot (2.4 per 10,000 fetuses). Syndactyly of the hand and foot occurred in 9 cases (1.2 per 10,000 fetuses) and 7 cases (0.8 per 10,000 fetuses), respectively.
The concept of congenital malformation is not strictly defined, and includes functional and metabolic disorders that, although present, may not necessarily be recognizable at birth (10, 11). Different classifications of congenital anomalies are used in different countries. The two most commonly used classification systems are: (1) the International Classification of Diseases system (12, 13), and (2) the International Clearinghouse for Birth Defects Monitoring System (ICBDMS) (14). In our study, the classification of birth defects was performed according to the European Registration of Congenital Anomalies and Twins (EUROCAT) and the ICBDMS (1994) system.
The EUROCAT program was initiated in 1979. This surveillance system details 900,000 births per annum in 17 countries. The International Clearing-house for Birth Defects Monitoring System (ICBDMS) is a WHO-related non-governmental organization, and more than 25 countries including the United States, England, France, Australia, Japan, and China participate in the program. These monitoring systems are based on registration. The Japanese Association of Obstetricians and Gynecologists (JAOG) program started in 1972. This system is a nationwide hospital-based monitoring system that covers about 10% of all births in Japan. In our study, the 10 medical centers (six tertiary centers, one secondary center, and three large local obstetric clinics) covered only about 3% of births in Korea.
During the 4-yr study period, the overall incidence of birth defects from the 10 medical centers in Korea was 1.8%. This is lower than the incidence of 2.4% provided by the EUROCAT registration system, which tends to produce lower figures than other passive registries (15). Moreover, it has been reported that active monitoring systems detect 50% more congenital malformations than passive monitoring systems (16). Therefore, the prevalence of birth defects in this study would be lower than the actual incidence.
The incidence of total chromosomal abnormalities was 0.3% and the incidence of the trisomy 21 was 9.2 per 10,000 births, which is slightly lower than the incidence in Glasgow (12.4 per 10,000 births) (17), in Atlanta, U.S.A. (11.3 per 10,000 births), and in Japan (10.4 per 10,000 births) (15).
In the present study, the most frequent abnormality was a cleft lip with or without a cleft palate with a prevalence of 10.3 per 10,000 births, which is higher than in the Atlanta (U.S.A.) study (9.9 per 10,000 births), but lower than in Japan (15.9 per 10,000 births) or China (13.6 per 10,000 births) (15). The incidence of cleft palate without cleft lip in Korea was found to be 1.4 per 10,000 births, which is lower than in other countries; Japan: 4.8 per 10,000 births, China: 2.4 per 10,000 births, and U.S.A.: 6.0 per 10,000 births. And the incidence of renal agenesis/dysgenesis in Korea was 7.6 per 10,000 births, which is higher than in Japan (4.3 per 10,000 births) and in the U.S.A. (5.3 per 10,000 births). The incidence of anencephaly and microtia in Korea (3.3 per 10,000 births and 2.7 per 10,000 births) were also higher than in Japan (1.9 per 10,000 births and 1.6 per 10,000 births) and in the U.S.A. (1.8 per 10,000 births and 0.9 per 10,000 births). The incidence of hypospadia (1.2 per 10,000 births) and spina bifida (0.2 per 10,000) in Korea were lower than in Japan (3.5/3.2 per 10,000 births) and in the U.S.A. (7.7/3.8 per 10,000 births). The incidences of hydrocephalus (3.6 per 10,000 births) and limb reduction defect (1.3 per 10,000 births) in Korea were lower than in Japan (7.5/3.8 per 10,000 births) and in the U.S.A. (7.1/4.9 per 10,000 births). Also, the incidence of gastroschisis (1.6 per 10,000 births) and abdominal wall defect (1.4 per 10,000 births) were lower than in Japan (2.3/7.1 per 10,000 births) and in the U.S.A. (2.0/4.0 per 10,000 births). The incidence of omphalocele (3.0 per 10,000 births) was lower than in Japan (4.6 per 10,000 births) but higher than in the U.S.A. (2.0 per 10,000 births).
The frequency of birth defects varies markedly between countries and depends on the observation time after birth, the types of malformations included, and on differences in the reporting and statistical procedures used (18). On the other hand, this difference in the frequency of birth defects within countries would be affected by ethnicity, eating habits, and environmental factors, or combined. More studies are needed to elucidate the underlying causes for the different incidences.
The highest proportion of birth defects involved the cardiovascular system (17.5%) followed by the genitourinary system (15.6%). Recently, it was proposed that poor semen quality, cryptorchidism, hypospadias and testicular cancer are symptoms of one underlying entity, testicular dysgenesis syndrome (TDS) (19). TDS may be caused by genetic or environmental factors, or both. Even though the clinical symptoms appear postnatally, TDS can cause an irreversible testicular dysgenesis during early fetal development. In addition, there are many recent reports that environmental factors, especially endocrine disrupting chemicals (EDCs), can be the cause of congenital malformation (20). These EDCs may cause a variety of defects in the endocrine and reproductive systems (21, 22). However, little is known about the underlying biochemical and molecular mechanisms, or the determinants of teratologic susceptibility, particularly in humans (20).
Possible explanations for the lower incidence of birth defects in the present study than in the EUROCAT program are: (1) we included neonates only within the first week of life, so that the defects recognizable thereafter might have been lost; (2) in stillbirth cases, autopsy is carried out less frequently than in the EUROCAT program. The lower frequency of autopsy in our study might have resulted in a lower derection rate of defects in the internal organs.
Our aim is to establish a multi-center birth defects monitoring system to evaluate the prevalence and serial occurrence of birth defects in Korea. Birth defect registries that acquire data through active rather than passive reporting can provide additional important data on birth defects (21). Such a multicenter birth defects monitoring system can provide high-quality information on birth defects in Korea. To check the serial occurrence of birth defects, it is necessary to increase the number of participating hospitals and to launch a nation-wide multi-center study.
Figures and Tables
References
1. Liu S, Joseph KS, Wen SW. Trends in fetal and infant deaths caused by congenital anomalies. Semin Perinatol. 2002. 26:268–276.

2. Kalter H, Warkany J. Medical progress. Congenital malformations: etiologic factors and their role in prevention (first of two parts). N Engl J Med. 1983. 308:424–431.
3. Queisser-Luft A, Stolz G, Wiesel A, Schlaefer K, Spranger J. Malformations in newborn: results based on 30,940 infants and fetuses from the Mainz congenital birth defect monitoring system (1990-1998). Arch Gynecol Obstet. 2002. 266:163–167.
4. Lechat MF, Dolk H. Registries of congenital anomalies: EUROCAT. Environ Health Perspect. 1993. 101:Suppl 2. 153–157.

5. Kim YW, Kim SJ, Hur SY, Lee GS, Lee Y, Kim EJ, Song SK, Kim SP. The clinical study of congenital anomalies. Korean J Obstet Gynecol. 1998. 41:1698–1703.
6. Park HK, Lee CH, Nam KH, Lee KH, Cho TH. The clinical epidemiologic study of congenital anomalies in the newborn infants. Korean J Obstet Gynecol. 1993. 36:1383–1390.
7. Park HK, Nam KH, Lee KH, Cho TH. The clinical epidemiologic study of congenital anomalies in the newborn infants. Korean J Perinatol. 1991. 2:58–67.
8. International Clearinghouse for Birth Defects Monitoring Systems, Annual Report 1992. Rome: International Center for Birth Defects.
9. Metropolitan Atlanta Congenital Defect Program: Congenital malformations surveillance. 1988. Atlanta: Centers for Disease Control.
10. Epstein CJ. Rudolph AM, Hoffman JIE, Rudolph CD, editors. Genetic disorders and birth defects. Rudolph's pediatrics. 1991. 19th ed. Norwalk, CT: Appleton & Lange;265–269.
11. Shi LM, Chia SE, Chan OY, Chew SK, Foong BH. Prevalence of birth defects and parental work in Singapore live births from 1994 to 1998: a population-based study. Occup Med (Lond). 2002. 52:325–331.

12. WHO. ICD-9. International Classification of Diseases. 9th revision. Geneva: WHO.
13. WHO. ICD-10. International Classification of Diseases. 10th revision. Geneva: WHO.
14. BPA. Classification of Diseases. 1987. Vols 1&2:2nd ed. British Pediatric Association.
15. International Clearinghouse for Birth Defects Monitoring Systems, Annual Report 2000. Rome: International Center for Birth Defects.
16. Lindberg MC, Edmons LD. Halperin W, Baker EL, editors. Surveillance of birth defects. Public health surveillance. 1992. 12. New York: Van Nostrand Reinhold;157–177.
17. Iliyasu Z, Gilmour WH, Stone D. Prevalence of Down syndrome in Glasgow, 1980-96; the growing impact of prenatal diagnosis on younger mothers. Health Bull (Edinb). 2002. 60:20–26.
18. Taskinen HK. Effects of parental occupational exposures on spontaneous abortion and congenital malformation. Scand J Work Environ Health. 1990. 16:297–314.

19. Weber RF, Pierik FH, Dohle GR, Burdorf A. Environmental influences on male reproduction. BJU Int. 2002. 89:143–148.

20. Wells PG, Winn LM. Biochemical toxicology of chemical teratogenesis. Crit Rev Biochem Mol Biol. 1996. 31:1–40.

21. Solomon GM, Schettler T. Environment and health: 6. Endocrine disruption and potential human health implications. CMAJ. 2000. 163:1471–1476.
22. Wilson JG. Environmental and birth defects. 1973. New York: Academic Press.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download