Abstract
Pillows are known to contain significant levels of indoor allergens and endotoxin, that are of importance to house dust mite sensitized asthmatics. Buckwheat pillows are commonly used in Korea. We studied the levels of the house dust mite allergen, Der f 1, and endotoxin on new synthetic and buckwheat pillows and their accumulation over three months. Endotoxin levels were significantly higher on new buckwheat pillows compared to synthetic pillows; geometric mean levels (95% CI) were 60,950 EU/g (30,270-122,700) and 4,887 EU/g (2,570-9,311) respectively (p<0.001). No Der f 1 was detected on the new pillows. After three months Der f 1 levels were similar on buckwheat and synthetic pillows, geometric mean levels (95% CI) were 1.16 µg/g (0.02-8.13) and 1.08 µg/g (0.19-1.68) respectively. These results indicate that buckwheat pillows are a source of very high endotoxin levels that may be of relevance to asthma severity of atopic asthmatics.
Sensitization to major allergens of the house dust mite (HDM) species, Dermatophagoides, is a known risk factor for asthma severity (1). Bedding, including pillows, are a significant source of HDM allergens. Furthermore, differences in HDM allergen levels exist between pillows with synthetic or feather filling (2-4), most likely due to differences in pore size of coverings of the different pillows (5). These differences in bedding allergen levels have become of importance lately as various cross-sectional studies have consistently shown that feather bedding is negatively associated with reported atopic diseases, or conversely a positive association with synthetic bedding (reviewed in Ref. 6). Recently, a longitudinal prospective infant cohort study demonstrated that risk for asthma at age four was negatively associated with use of feather bedding from birth (7). Endotoxin, a pro-inflammatory compound from cell walls of Gram-negative bacteria, exacerbates asthma in HDM-sensitized asthmatics, even with low levels in air in domestic dwellings (8). Significant levels of endotoxin are found in bedding, including pillows (9).
Buckwheat pillows are commonly used in Asian countries, including Korea. Although buckwheat pillows have been implicated in IgE sensitization to buckwheat (10), and one report of infestation of buckwheat pillows with Dermatophagoides farinae (11); to our knowledge, levels or accumulation of HDM allergen or endotoxin from buckwheat pillows has not previously been reported. In this study we report on HDM allergen and endotoxin levels on new synthetic and buckwheat pillows, and their accumulation over a three month period in the domestic setting. An unusual finding of our study was the more than 10-fold higher levels of endotoxin on buckwheat pillows, compared to synthetic pillows.
Thirteen pairs of pillows, each pair consisting of a new synthetic pillow (Sungwoosa) and new buckwheat pillow (Jangmisa), were placed on beds of 13 volunteers. Thus, identical pillows were provided to the volunteers. Before placement dust samples were collected by vacuuming each pillow for 30 sec on each side (total 1 min). Dust was also collected from the corresponding mattresses by vacuuming 1 m2 for 1 min. After three months, dust was again collected from all pillows as described above. Dust samples were stored at -20℃ before dust extraction and analysis.
Dust weights were recorded (to 0.1 mg). Dust samples were extracted initially with endotoxin-free water containing 0.05% Tween-20 (1 mL for pillow dust samples and 5 mL for mattress dust samples). The extracts were shaken for 60 min at room temperature and then centrifuged for 15 min at 1,000 g. One-tenth of the supernatant volume was placed in endotoxin-free glass tubes and stored at -20℃ for endotoxin activity analysis. An equal volume (equivalent to the above removed supernatant) of 10× concentrated phosphate-buffered saline (pH 7.4) was added to the extraction tube, shaken for 30 min at room temperature and then centrifuged for 10 min at 3,000 g. A portion of the supernatant was removed and stored at -20℃ for HDM allergens analysis.
We also analysed the filling of one buckwheat pillow for endotoxin content by extracting a small amount of the buckwheat husks (0.1118 g) with 5 mL of endotoxin-free water, as detailed above.
The HDM allergens, Der p 1 and Der f 1 in the dust extracts were determined by double monoclonal antibody ELISA methodology with commercial kit sets (Indoor Biotechnologies, Cardiff, U.K.) in duplicate at 1:20, 1:80 and 1:320 dilutions (12).
Endotoxin in the dust extracts were determined by the kinetic chromogenic Limulus amoebocyte lysate method with a commercial kit set (BioWhittaker, Walkersville, MD, U.S.A.) at a 1:500 dilution (13).
As endotoxin and HDM allergen data were not normally distributed, results were log transformed before data analysis. Endotoxin and HDM allergens results are reported as geometric means with 95% confidence interval (CI). Endotoxin results are expressed as endotoxin units per gram of dust (EU/g), HDM allergens as micrograms per gram of dust (µg/g).
Comparison of log transformed endotoxin and HDM allergen results between synthetic and buckwheat pillows was by paired t-test, while correlations were by least square linear regression analysis. Statistical significance was set at the p 0.05 level.
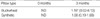
Endotoxin was readily detectable in both types of new pillows and increased non-significantly after three months (Table 1). At both time points buckwheat pillows contained significantly higher endotoxin levels compared to synthetic pillows. Mean ratios buckwheat: synthetic (95% CI) were 12.5 (4.7-32.7) and 12.7 (5.7-28.3) respectively for new pillows and after three months. Geometric mean endotoxin from mattresses was 7,798 EU/g (95% CI: 5,070-11,910). There were no significant correlations between mattress and buckwheat or synthetic pillow endotoxin levels.
No Der p 1 was detected in any of the dust samples. Der f 1 was undetectable in dust samples from the new pillows, but after three months placement on mattresses detectable levels were observed. No significant difference in Der f 1 levels between synthetic and buckwheat pillows were apparent at three months. These results are shown in Table 2.
All mattresses had detectable Der f 1 levels, geometric mean: 1.18 µg/g (95% CI: 0.39-3.62). There were positive correlations between mattress Der f 1 levels and both buckwheat and synthetic pillow Der f 1 levels (r=0.524, p=0.066; and r=0.511, p=0.075 respectively).
The main finding of our study was significantly higher levels of endotoxin on buckwheat pillows, compared to synthetic pillows. A previous study showed that geometric mean endotoxin levels from synthetic and feather pillows were 23,158 EU/g and 35,269 EU/g respectively (9). Results of that study cannot be directly compared to those of the present study as pillows from that study were at least six months on beds and possibly some for many years. However, results from our present study have shown that new buckwheat pillows had much higher endotoxin levels than previously reported in other pillows. To our knowledge, pillow endotoxin levels have previously been described in only one study (9).
Given that we spend about a third of our life in bed and the close proximity of pillows to the airway, levels of endotoxin on pillows could be of relevance to atopic asthmatics. Michel and colleagues showed that exposure to endotoxin is a determinant of asthma severity in HDM sensitized asthmatics (14), and recently Boehlecke and colleagues showed that air endotoxin, at levels commonly found within the domestic environment, exacerbates asthma in atopic asthmatics (8). The very high endotoxin levels from buckwheat pillows most likely results from their filling. As shown in the results, total endotoxin content from one buckwheat pillow was nearly 22 million EU. The endotoxin from the buckwheat husks most likely comes from buckwheat flour residue given that in buckwheat pillow manufacturing in Korea, the husks are not normally cleaned. Buckwheat pillow manufacturers in Korea do not use detergents nor wash the husks, they just remove the fine dust from the husks and pack the pillows (personal communications). In the U.S.A., unlike Korea, buckwheat husks used for filling buckwheat pillows are normally extensively cleaned. It would be of interest to see whether this extensive cleaning process significantly reduces their endotoxin levels.
A limitation of our study is that we tested buckwheat pillows from one manufacturer only. It is possible that differences in endotoxin levels may excist between different brands of buckwheat pillows due to differences in buckwheat husk storage, pillow production processes, or buckwheat cultivation. However, the endotoxin levels in the buckwheat pillows tested in our study were extremely high, most likely due to the very high endotoxin contamination of the buckwheat husks, and were more than 10-fold higher compared to synthetic pillows.
We were unable to detect Der p 1 in either mattresses or pillows, only Der f 1. It has previously been shown that both Dermatophagoides pteronyssinus and Dermatophagoides farinae are the predominant HDM species found in Korea, with Dermatophagoides farinae dominant (15). That study also showed regional variation in HDM species. We presume that Dermatophagoides farinae is dominant in Cheonan, although this must be treated with caution as we only studies 13 domestic locations and we may by chance have failed to detect the HDM allergen Der p 1 produced by Dermatophagoides pteronyssinus.
Der f 1 accumulation on both types of pillows over three months was governed by the mattress Der f 1 levels. This has also previously been demonstrated for synthetic and feather pillows (3). Synthetic pillow coverings have a pore size of greater than 20 µm allowing live HDM to penetrate the coverings, colonise within the pillow and contribute towards allergen production within the pillow, while feather pillow coverings do not due to their lower pore size (5). Although we did not measure pore size of the buckwheat pillow coverings, given their similar Der f 1 accumulation to synthetic pillows we reasonably assume their pore size to be similar to synthetic pillows.
In conclusion, in Korea new buckwheat pillows contain very high levels of endotoxin. Atopic asthmatics should perhaps avoid use of such pillows given the exacerbative effect of endotoxin on asthma in these patients. Future research should determine whether the use of buckwheat pillows by atopic asthmatics contributes towards increased asthma symptoms and bronchial hyperresponsiveness.
References
1. Tunnicliffe WS, Fletcher TJ, Hammond K, Roberts K, Custovic A, Simpson A, Woodcock A, Ayres JG. Sensitivity and exposure to indoor allergens in adults with differing asthma severity. Eur Respir J. 1999. 13:654–659.

2. Kemp TJ, Siebers RW, Fishwick D, O'Grady GB, Fitzharris P, Crane J. House dust mite allergen in pillows. Br Med J. 1996. 313:916.

3. Rains N, Siebers R, Crane J, Fitzharris P. House dust mite allergen (Der p 1) accumulation on new synthetic and feather pillows. Clin Exp Allergy. 1999. 29:182–185.

4. Mills S, Siebers R, Wickens K, Crane J, Purdie G, Fitzharris P. House dust mite allergen levels in individual bedding components in New Zealand. N Z Med J. 2002. 115:151–153.
5. Siebers R, Nam HS, Crane J. Permeability of synthetic and feather pillows to live house dust mites and house dust. Clin Exp Allergy. 2004. 34:888–890.

6. Siebers R, Fitzharris P, Crane J. Feather bedding and allergic disease in children: a cover story? Clin Exp Allergy. 2002. 32:1119–1123.

7. Nafstad P, Nystad W, Jaakkola JJ. The use of feather quilt, childhood asthma and allergic rhinitis. A prospective cohort study. Clin Exp Allergy. 2002. 32:1150–1154.
8. Boehlecke B, Hazucha M, Alexis NE, Jacobs R, Reist P, Bromberg PA, Peden DB. Low-dose airborne endotoxin exposure enhances bronchial responsiveness to inhaled allergen in atopic asthmatics. J Allergy Clin Immunol. 2003. 112:1241–1243.

9. Hall K, Crane J, Siebers R. Endotoxin from synthetic and feather pillows. J Allergy Clin Immunol. 2002. 110:811.

10. Lee SY, Lee KS, Hong CH, Lee KY. Three cases of childhood nocturnal asthma due to buckwheat allergy. Allergy. 2001. 56:763–766.

11. Hong CS, Park HS, Oh SH. Dermatophagoides farinae, an important allergenic substance in buckwheat-husk pillows. Yonsei Med J. 1987. 28:274–281.

12. Luczynska CM, Arruda LK, Platts-Mills TA, Miller JD, Lopez M, Chapman MD. A two-site monoclonal antibody ELISA for the quantification of the major Dermatophagoides spp allergens Der p 1 and Der f 1. J Immunol Meth. 1989. 118:227–235.
13. Nam HS, Crane J, Siebers R. Clothing-potentially a significant source of endotoxin exposure. J Allergy Clin Immunol. 2003. 112:624–625.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download