Abstract
We tested the hypothesis that angiotensin-converting enzyme (ACE) and angiotensinogen gene polymorphism influence the incidence, development and outcome of preeclampsia. Subjects were recruited from 90 Korean patients with preeclampsia during pregnancy and 98 age-matched controls. After isolation of DNA, polymerase chain reactions (PCR) were carried out to detect polymorphism of the ACE and angiotensinogen. M235T and T174M genotypes of angiotensinogen were determined by digestion with restriction enzyme endonuclease Tth 111-I and NCo I, respectively. The frequency of DD genotype was significantly greater in preeclampsia (0.36) than in controls (0.14) (p<0.05). The frequency of D allele was 0.55 in preeclampsia and 0.40 in controls (p<0.05). There were no differences in the onset of preeclampsia and pregnancy outcomes according to the ACE genotypes. There was no difference in the frequency of a allele of angiotensinogen M235T between the groups (0.79:0.78 in preeclampsia : controls). The frequency of T allele of angiotensinogen T174M gene was slightly increased, but not significantly, in preeclampsia (0.11) than in controls (0.07). In a multivariate analysis, only ACE genotype was associated with the development of preeclampsia (β=0.27, p=0.05). In conclusion, a molecular variant of ACE, but not angiotensinogen, gene is associated with preeclampsia in Korean women.
Preeclampsia, characterized by hypertension, proteinuria or edema after the 20th week of gestation, is a heterogeneous disorder which complicates 5-7% of all pregnancies and remains a leading cause of maternal and fetal mortality (1). Although the etiology is unclear, a strong genetic component has been suggested because it is more common in blood relatives of affected women (2) and in pregnancies fathered by sons of preeclamptic women (3). The renin-angiotensin (RA) system has been implicated to play a role in the pathophysiology of preeclampsia. Data in support of this include 1) lower levels of all circulating components of the RA system, and activation of cellular and tissue RA components at the same time, and 2) pregnancy-associated blunting of angiotensin II (AII) pressor responsiveness which is owing to excessive upregulation of AII receptors in a variety of tissues (4, 5). However, why some women are prone to and others are protected from this disease is unknown. It has been suggested that genetic factors such as gene polymorphisms of the RA system may play an important role in the regulation of blood pressure (BP) in preeclampsia.
Ward et al. (6) and Arngrimsson et al. (7) found that a molecular variant of angiotensinogen (M235T) in Caucasians and Japanese was significantly associated with preeclampsia and in part influenced the development of preeclampsia. Recently in Korean women, familial tendency of hypertension and angiotensinogen AA genotype showed an association with high BP in hypertensive disorder in pregnancy (8). On the contrary, Guo et al. (9) found that there was no significant association of the M235T allele of angiotensinogen with preeclampsia/eclampsia in a population case-control study among Australians and Chinese. An insertion/deletion polymorphism in the angiotensin-converting enzyme (ACE) gene is associated with serum ACE activities, with the DD genotype having the highest activity (10). Although the DD type of ACE gene polymorphism is suggested to be a circulatory maladaptation in hypertension during pregnancy, there was no effect of ACE gene polymorphism on pregnancy outcome, the incidence of pregnancy-induced hypertension (PIH) or changes in BP during pregnancy (11). Differences in ethnic background probably contribute to variable gene frequencies of the RA system, which may manifest as differences in the incidence of these disorders in population groups (12, 13). In the present study, we questioned whether ACE and angiotensinogen gene polymorphisms might be associated with preeclampsia in Korean women.
Ninety consecutive patients with preeclampsia were recruited from the Hypertension Clinic at the Samsung Cheil Hospital, Sungkyunkwan University School of Medicine between May 1996 and January 2000. The system advocated by the U.S. National Institute of Health working group on hypertension in pregnancy was used for the classification of hypertension during pregnancy (14). The definition used for preeclampsia, commonly referred to as severe preeclampsia, is based on hypertension (BP greater than systolic BP 140 mmHg or diastolic BP 90 mmHg) and more than 1 g/L (or 2+ dipstick) of proteinuria in random urine determinations with or without edema after the 20th week of pregnancy. Cases of mild preeclampsia (less than +1 proteinuria by dipstick) were not included in this study. To exclude underlying renal disease, we confirmed the absence of proteinuria more than four weeks after delivery. Other exclusion criteria included overt cardiac disease, serum creatinine >150 µmol/L or the presence of other systemic disease. Ninety-eight normotensive volunteers (age-matched control) were randomly recruited from the Obstetrics clinic at the Samsung Cheil Hospital intermittently between 1996 and 2000. The Ethical Committee of Samsung Cheil Hospital approved the protocol and informed consent was obtained from all participants.
DNA was isolated from peripheral leukocytes using commercially available kit (Takara Co., Ltd., Japan). All polymerase chain reactions to detect polymorphism of the ACEand angiotensinogen (M235T and T174M) genes were carried out with 100 ng of genomic DNA as a template, using a DNA Thermal Cycler PJ2000 (Perkin Elmer Co., Norwalk, CT, U.S.A.). To identify I/D polymorphism of the ACE gene, the protocol of Rigat et al. (15) was used. Because of some reports of false negative results for the insertion, nested PCR was performed in all cases of II genotype (16). The PCR products of two alleles of 490 and 190 bp were electrophoresed in 2% agarose gels, and visualized by ethidium bromide staining. The protocols of genotyping of angiotensinogen, T174M an M235T, were taken from those of Morise et al. (17) and Bennett et al. (18), respectively. To identify the genotype of angiotensinogen (M235T), PCR products were digested with restriction endonuclease Tth 111-1, electrophoresed in 2% agarose gels, and visualized by ethidium bromide staining. The genotype of angiotensinogen (T174M) was determined by digestion of 303 bp amplified product with an exiting NCo I cutting site and electrophoresed in 2.5% agarose gel.
To determine whether the proportions of the genotype observed in our data were those to be expected in a random mating equilibrium population, they were explored using the χ2 method under the Hardy-Weinberg law. The clinical characteristics of the two or three groups were expressed as mean±SD and were compared by using the Student's t-test or ANOVA. Allele frequencies were deducted from genotype frequencies, and differences in the distribution of genotypes between preeclampsia and control group were determined by the chi-square test. p value <0.05 was considered to be significant.
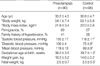
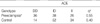
There were no differences in maternal age, body weight and body mass index before pregnancy between preeclampsia and control. The gestational age at birth and birth weight were significantly lower in preeclampsia (Table 1). The peak systolic/diastolic BP during pregnancy was 155±17/100±14 mmHg in the preeclampsia and 118±11/75±8 mmHg in the control (both, p<0.01). The genotypic distribution of the ACE and angiotensinogen gene was compatible with the population in the Hardy-Weinberg equilibrium. The frequency of DD genotype was significantly greater in preeclampsia (0.36) than in controls (0.14) (p<0.05). The frequency of D allele was 0.55 in preeclampsia, and 0.40 in controls (p<0.05) (Table 2). In regard to the disease onset, there was no difference in the onset of proteinuria according to ACE genotypes: 33.1 weeks in DD and 34.7 weeks in II (p>0.05). The onset of hypertension (more than 140/90 mmHg) in preeclampsia was 33.7 in DD, 35.3 in ID, and 33.7 weeks in II (p>0.05) (Table 3). In preeclampsia, there was no significant association of pregnancy outcome according to the ACE genotypes: no difference in the gestational age at birth and the birth weight among the three genotypes (Table 3). The number of intrauterine fetal death was 2 in DD, 3 in ID, and 2 II according to the ACE genotype in patients with preeclampsia (p>0.05). In a multivariate analysis including age, prepregnancy body weight and body mass index, weight gain, primigravida, and genotypes of ACE and angiotensinogen, the ACE genotype was the only marker associated with the development of preeclampsia (β=0.27, p=0.05).
We could not find significant association of the molecular variant of angiotensinogen (M235T) in preeclampsia and controls; aa:Aa was 0.56:0.42 in preeclampsia and aa:Aa:AA was 0.61:0.33:0.06 in controls. There were no differences in the frequency of a allele of angiotensinogen M235T in the two groups (0.79:0.78 in preeclampsia : controls, respectively p> 0.05) (Table 4). The genotype of angiotensinogen T174M showed CC:CT:TT was 0.85:0.14:0.01 in controls (p>0.05). The frequency of T allele was slightly increased, but not significantly, in preeclampsia (0.11) than controls (0.07) (p>0.05).
ACE and angiotensinogen are key components of the RA system, which is a powerful regulatory system with a major influence on salt and water metabolism and blood pressure. In this study, we found that ACE gene polymorphism has a significant impact on the development of preeclampsia without affecting the outcome of pregnancy in Korean women. To our knowledge, this is the first positive result on the association of preeclampsia and ACE gene polymorphism.
There are conflicting results on the relationship of ACE activities with pregnancy-induced hypertension or preeclampsia and chronic hypertension superimposed on pregnancy-induced hypertension (19, 20). Plasma ACE level has been associated with the insertion/deletion (I/D) polymorphism in intron 16 of the ACE gene (15). The ACE I/D polymorphism accounted for half of total phenotypic variance of serum ACE, contributing much to the variability of ACE level (15). The DD genotype is associated with higher tissue and plasma ACE levels, whereas the II genotype is associated with lower levels and the ID genotype with intermediate levels. The reason for the higher ACE levels in the D allele has been assumed that the I allele has a sequence similar to a silencer sequence (21). In other studies, however, ACE activity and ACE I/D polymorphism were not found to be associated with preeclampsia (22-24). Rasmussen et al. (25) found that serum ACE activities were lower in patients with preeclampsia than women with normal pregnancy, and proposed that this phenomenon reflects a decreased placental synthesis of ACE in preeclampsia. In the present study, we did not measure ACE activities.
Data from animal studies have shown that the hypertension gene is close to the ACE gene locus (26, 27). Based on this, it could be postulated that the D allele of ACE gene is more common in preeclampsia than normotensive controls. Our data here support this notion as with other study (28). The frequency of ACE gene polymorphism in the general population of Korea is that DD:ID:II was 0.16:0.49:0.35, respectively, and D:I allele frequency was 0.41:0.59 (12). The frequency of the DD genotype in patients with preeclampsia was about 2.5 times higher compared to general population and normotensive women during pregnancy in Korea. However, there were other studies showing no association or opposite result on the ACE genotype and preeclampsia (29, 30). In a relative small study in Korean women, the I allele of the ACE gene was associated with preeclampsia (30). In each ACE genotype, there was no significant association between the genotypes and the onset of proteinuria and hypertension in our study. Also we could not find any association of pregnancy outcome with ACE genotype. This is in agreement with that of Tamura et al. (11). It is unclear to explain this mismatched ACE genetic influence on the incidence of preeclampsia without affecting on the outcome of pregnancy, but the multifactorial pathogenesis on the development and complication in preeclampsia and also physician's intervention may contribute to the pregnancy outcome. One interesting study on the ACE genetic polymorphism and obstetric complication showed that the D genotype had higher recurrence of an adverse pregnancy outcome in women with a history of preeclampsia by affecting uteroplacental and umbilical flows (28).
Jeunemaitre et al. (31) have proposed that increased concentration of plasma or tissue angiotensinogen in individuals carrying variants of angiotensinogen, such as M235T, could lead to increased baseline or reactive production of angiotensin II, the final effector hormone of the RA system. This long-standing over-stimulation could activate autoregulatory mechanisms, resulting in increased vascular tone and hypertrophy. This could trigger an imbalance between vasodilatory and vasoconstrictory mechanisms: increased sensitivity to angiotensin II concurrent with the reduced plasma levels of most components of this system (32). At first in 1993, Ward et al. (6) and Arngrimsson et al. (7) observed a significant association of preeclampsia with a molecular variant of angiotensinogen, M235T, in Caucasians and Japanese, and this higher plasma concentration of angiotensinogen observed in carriers of the M235T variants may cause a greater circulatory maladaptation of the RA system during pregnancy. In contrast, Guo et al. (9) found that there was no significant difference in the genotypes frequencies of the M235T allele between preeclampsia/eclampsia cases and controls in Australian and Chinese populations, but this may be attributable to the criteria used to diagnose preeclampsia. In our results, the frequencies of the M235T allele were very similar to those of preeclampsia/eclampsia and control groups in Chinese subjects. Because different diagnostic criteria for preeclampsia may influence experimental and control groups, we recruited true severe preeclampsia: pregnancy-specific complication with hypertension and more than 1 g/L of proteinuria with/without edema, which occurred later than the 20th weeks of pregnancy. Patients who were hypertensive without proteinuria were classified as pregnancy-induced hypertension. Racial differences in an association study could lead to spurious differences in allele frequencies. Therefore, only Korean women were recruited in our study.
Preeclampsia is a multisystem and multifactorial complication of pregnancy. The precise cause of preeclampsia has not been determined, but maladaptation to the RA system may play a role. The products of genes involving the components of this system may be potential candidates for preeclampsia and hypertension related to pregnancy. In conclusion, our study showed that I/D polymorphism of the ACE gene, rather than angiotensinogen gene, T174M and M235T, is associated with incidence, but not with the outcome, of preeclampsia in Korean women. Different gene polymorphism of the components of the RA system may contribute to the heterogeneity of preeclampsia in different ethnic groups. In Korean woman, the molecular variant of the ACE gene seems to be important.
Figures and Tables
ACKNOWLEDGMENTS
The authors are deeply indebted to Dr. Rhian M. Touyz for her invaluable review and comments on this article.
References
1. Roberts JM, Pearson G, Cutler J, Lindheimer M. NHLBI Working Group on Research on Hypertension During Pregnancy. Summary of the NHLBI Working Group on Research on Hypertension During Pregnancy. Hypertension. 2003. 41:437–445.

2. Cooper DW, Hill JA, Chesley LC, Bryans CI. Genetic control of susceptibility to eclampsia and miscarriage. Br J Obstet Gynaecol. 1988. 95:644–653.

3. Esplin MS, Fausett MB, Fraser A, Kerber R, Mineau G, Carrillo J, Varner MW. Paternal and maternal components of the predisposition to preeclampsia. N Engl J Med. 2001. 344:867–872.

5. Roberts JM, Lain KY. Recent Insights into the pathogenesis of preeclampsia. Placenta. 2002. 23:359–372.

6. Ward K, Hata A, Jeunemaitre X, Helin C, Nelson L, Namikawa C, Farrington PF, Ogasawara M, Suzumori K, Tomoda S, Berrebi S, Sasaki M, Corvol P, Lifton RP, Lalouel JM. A molecular variant of angiotensinogen associated with preeclampsia. Nat Genet. 1993. 4:59–61.

7. Arngrimsson R, Purandare S, Connor M, Walker JJ, Bjornsson S, Soubrier F, Kotelevtsev YV, Geirsson RT, Bjornsson H. Angiotensinogen: a candidate gene involved in preeclampsia? (letter). Nat Genet. 1993. 4:114–115.
8. Shim SS, Shim JY, Lim JH, Park JS, Jun JK, Bai KB, Yoon BH, Syn HC. Molecular biological approach to find out the etiology of hypertensive disorder in pregnancy: analysis of the polymorphism in the promoter of human angiotensinogen gene in Korean population. Korean J Obstet Gynecol. 2003. 46:1486–1492.
9. Guo G, Wilton AN, Fu Y, Qiu H, Brennecke SP, Cooper DW. Angiotensinogen gene variation in a population case-control study of preeclampsia/ eclampsia in Australians and Chinese. Electrophoresis. 1997. 18:1646–1649.
10. Nakai K, Itoh C, Miura Y, Hotta K, Musha T, Itoh T, Miyakawa T, Iwasaki R, Hiramori K. Deletion polymorphism of the angiotensin I-converting enzyme gene is associated with serum ACE concentration and increased risk for CAD in the Japanese. Circulation. 1994. 90:2199–2202.

11. Tamura T, Johanning GL, Goldenberg RL, Johnston KE, DuBard MB. Effect of angiotensin-converting enzyme gene polymorphism on pregnancy outcome, enzyme activity, and zinc concentration. Obstet Gynecol. 1996. 88:497–502.

12. Kim DK, Kim JW, Kim S, Gwon HC, Ryu JC, Huh JE, Choo JA, Choi Y, Rhee CH, Lee WR. Polymorphism of angiotensin converting enzyme gene is associated with circulating levels of plasminogen activator inhibitor-1. Arterioscler Thromb Vasc Biol. 1997. 17:3242–3247.

13. Johanning GL, Johnston KE, Tamura T, Goldenberg RL. Ethnic differences in angiotensin converting enzyme gene polymorphism. J Hypertens. 1995. 13:710–711.

14. Report of the National High Blood Pressure Education Program Working Group on high blood pressure in pregnancy. Am J Obstet Gynecol. 2000. 183:S1–S22.
15. Rigat B, Hubert C, Alhenc-Gelas F, Cambien F, Corvol P, Soubrier F. An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J Clin Invest. 1990. 86:1343–1346.

16. Marre M, Jeunemaitre X, Gallois Y, Rodier M, Chatellier G, Sert C, Dusselier L, Kahal Z, Chaillous L, Halimi S, Muller A, Sackmann H, Bauduceau B, Bled F, Passa P, Alhenc-Gelas F. Contribution of genetic polymorphism in the renin-angiotensin system to the development of renal complications in insulin-dependent diabetes: Genetique de la Nephropathie Diabetique (GENEDIAB) study group. J Clin Invest. 1997. 99:1585–1595.

17. Morise T, Takeuchi Y, Takeda R. Rapid detection and prevalence of the variants of the angiotensinogen gene in patients with essential hypertension. J Intern Med. 1995. 237:175–180.

18. Bennett CL, Schrader AP, Morris BJ. Cross-sectional analysis of Met235-->Thr variant of angiotensinogen gene in severe, familial hypertension. Biochem Biophys Res Commun. 1993. 197:833–839.
19. Cugini P, Letizia C, Di Palma L, Battisti P, Caserta D, Moscarini M, Scavo D. Serum angiotensin-converting enzyme activity in pre-eclamptic pregnancy: evidence for a relative hypermesorACEemia. Enzyme. 1990. 43:113–121.
20. Dux S, Yaron A, Carmel A, Rosenfeld JB. Renin, aldosterone, and serum-converting enzyme activity during normal and hypertensive pregnancy. Gynecol Obstet Invest. 1984. 17:252–257.

21. Jackson A, Brown K, Langdown J, Luddington R, Baglin T. Effect of the angiotensin-converting enzyme gene deletion polymorphism on the risk of venous thromboembolism. Br J Haematol. 2000. 111:562–564.

22. Langer B, Grima M, Coquard C, Bader AM, Schlaeder G, Imbs JL. Plasma active renin, angiotensin I, and angiotensin II during pregnancy and in preeclampsia. Obstet Gynecol. 1998. 91:196–202.

23. Morgan L, Foster F, Hayman R, Crawshaw S, Baker PN, Pipkin FB, Kalsheker N. Angiotensin converting enzyme insertion-deletion polymorphism in normotensive and preeclamptic pregnancies. J Hypertens. 1999. 17:765–768.
24. Heiskanen JTM, Pirskanen MM, Hiltunen MJ, Mannermaa AJ, Punnonem KRA, Heinonen ST. Insertion-deletion polymorphism in the gene for angiotensin-converting enzyme is associated with obstetric cholestasis but not with preeclampsia. Am J Obstet Gynecol. 2001. 185:600–603.

25. Rasmussen AB, Pedersen EB, Romer FK, Johannesen P, Kristensen S, Lauritsen JG, Wohlert M. The influence of normotensive pregnancy and pre-eclampsia on angiotensin-converting enzyme. Acta Obstet Gynecol Scand. 1983. 62:341–344.

26. Jacob HJ, Lindpaintner K, Lincoln SE, Kusumi K, Bunker RK, Mao YP, Ganten D, Dzau VJ, Lander ES. Genetic mapping of a gene causing hypertension in the stroke-prone spontaneously hypertensive rat. Cell. 1991. 67:213–224.

27. Hilbert P, Lindpaintner K, Beckmann JS, Serikawa T, Soubrier F, Dubay C, Cartwright P, De Gouyon B, Julier C, Takahasi S, Vincent M, Ganten D, Georges M, Lathrop GM. Chromosomal mapping of two genetic loci associated with blood-pressure regulation in hereditary hypertensive rats. Nature. 1991. 353:521–529.

28. Mello G, Parretti E, Gensini F, Sticchi E, Mecacci F, Scarselli G, Genuardi M, Abbate R, Fatini C. Maternal-fetal flow, negative events, and preeclampsia: role of ACE I/D polymorphism. Hypertension. 2003. 41:932–937.
29. Fatini C, Gensini F, Battaglini B, Prisco D, Cellai AP, Fedi S, Marcucci R, Brunelli T, Mello G, Parretti E, Pepe G, Abbate R. Angiotensin converting enzyme DD genotype, angiotensin type 1 receptor CC genotype, and hyperhomocysteinemia increase first-trimester fetalloss susceptibility. Blood Coagul Fibrinolysis. 2000. 11:657–662.
30. Roh CR, Kim DK, Yoon BK, Yang SH, Chung JH, Bae DS, Lee JH. A common genetic variant of the angiotensin converting enzyme (ACE) gene and pregnancy induced hypertensive disorders. Korean J Obstet Gynecol. 1997. 40:1189–1199.
31. Jeunemaitre X, Soubrier F, Kotelevtsev YV, Lifton RP, Williams CS, Charru A, Hunt SC, Hopkins PN, Williams RR, Lalouel JM, Corvol P. Molecular basis of human hypertension: role of angiotensinogen. Cell. 1992. 71:169–180.

32. August P, Sealey JE. Lahagh JH, Brenner BM, editors. The renin-angiotensin system in normal and hypertensive pregnancy and in ovarian function. Hypertension: Pathophysiology, Diagnosis, and Management. 1990. New York: Raven Press;1761–1778.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download