Abstract
The C677T mutation in the methylene tetrahydrofolate reductase (MTHFR) gene results in elevated homocysteine levels and, presumably, in increased cardiovascular risk. Moreover, elevated homocysteine levels are reportedly associated with high serum uric acid levels. We evaluated the MTHFR genotype and a panel of biochemical, hematological variables, and lifestyle characteristics in 327 elderly Korean men (age range 40-81 yr; mean, 51.87). This study shows that mutation of the MTHFR gene may be a risk for hyperuricemia. The mean uric acid levels for the C/C, C/T and T/T genotypes were 5.54, 5.91 and 6.33 mg/dL, respectively (p=0.000). The T/T genotype was significantly more frequent in subjects with high uric acid levels (p=0.003). Thus, this mutation of the MTHFR gene is implied by the study results to be a risk factor of hyperuricemia in elderly Korean men. However, the relationship between the MTHFR mutation and uric acid metabolism remains unclear. Therefore, further studies are necessary to explain the associated between the MTHFR mutation and elevated uric acid levels, and to examine potential relationships between it and conventional cardiovascular risk factors.
Methylene tetrahydrofolate reductase (MTHFR) is a cytoplasmic enzyme of which gene located on chromosome 1p36.3 in man. MTHFR catalyze the reduction of 5, 10-methylenetetrahydrofolate to 5-methyltetrahydrofolate, the primary methyl donor for the methylation of homocysteine to methionine. Severe deficiency of MTHFR causes an increase in homocysteine levels and is associated with developmental delay, neurological abnormalities and vascular complications (1-4). The C677T MTHFR mutation involves the substitution of an alanine residue for a valine, which results in a substantial reduction in its thermolabile enzymatic activity. With two copies of the TT variant, serum MTHFR activity is reduced to 30% of that of wild-type (CC), whereas the serum activity of CT heterozygotes is 65% of the wild-type (5). Therefore, the C677T MTHFR mutation is being viewed as a possible genetic contributor to hyper-homocysteinemia.
A direct relation between plasma homocysteine levels and serum uric acid was observed in patients with atherosclerosis and in control subjects (6-10). These findings indicate that the association between the two biochemical variables is indeed strong in the presence of homozygosity for thermolabile MTHFR. This could imply a greater availability of 5, 10-methylenetetrahydrofolate, substrate of the MTHFR reaction, for other metabolic uses, such as the de novo synthesis of purines via 10-formyltetrahydrofolate, with consequent overproduction of uric acid.
Hyperuricemia is commonly associated with other known risk factors for cardiovascular disease, such as obesity, hyperlipidemia, and hypertension, and in large epidemiological surveys, such as the Framingham study, it has been related to the occurrence of myocardial infarction. Yet, these associations are not fully understood.
Therefore, we studied a population of Korean elderly males, in order to investigate the relationships between the C677T MTHFR mutation and serum uric acid, and with other variables traditionally associated with cardiovascular risk.
Three hundred and twenty-seven unrelated men, aged 40 yr or more, were recruited into the study after obtaining informed consent. All subjects underwent clinical examinations at Dong-A University Hospital between September 2002 and June 2003. None of the subjects were diagnosed as having gout or renal failure (>1.5 mg/dL of serum creatinine). The mean age of the subjects was 51.9 yr (range, 40-81 yr). The percentages of subjects with hypertension (systolic blood pressure, 160 mmHg or diastolic blood pressure, ≥95 mmHg), diabetes mellitus or impaired glucose tolerance (hemoglobin A1c (HbA1c), ≥6.5%), hypercholesterolemia (plasma total cholesterol, ≥220 mg/dL), and hyperglyceridemia (triglycerides, ≥150 mg/ dL) were 11.2%, 4.7%, 21.9% and 24.2%, respectively. Body mass index (BMI) was computed as weight (kg) divided by height (m2). Data on alcohol intake and smoking habits were obtained by interview. The subjects were asked to quantify their consumption of alcohol in terms of the kind of alcoholic beverage usually drunk and the minimum consumption per week. Alcohol intakes were then converted into grams of alcohol per day. The number of cigarettes smoked per day was also noted.
A venous blood sample was drawn from each of the participants. DNA was extracted, using a Wizard Genomic DNA Purification Kit (Promega, Madison, U.S.A.), and stored at -20℃ until analyzed. Serum was used for clinical chemistry laboratory examinations at Dong-A University Hospital.
Polymerase chain reaction (PCR) was carried out using a PCR thermal cycler (TP2000; Takara Biomedicals, Kyoto, Japan). Thirty microliters of reaction mixture contained 200 ng of genomic DNA in 1× Expanded High Fidelity buffer (Boehringer Mannheim, Amsterdam, The Netherland) with 1.5 mM MgCl2, 250 µM dNTPs, 0.5 µM primers, and 0.7 units of Expand High Fidelity PCR System Enzyme Mix (Boehringer Mannheim). The sequences of the primers were as follows: 5'-TGAAGGAGGTGTCTGCGGGA-3' and 5'-AGGACGGTGCGGTGAGAGTG-3'(11). The conditions for PCR included an initial denaturation at 94℃ for 3 min, followed by 30 cycles of denaturation at 94℃ for 1 min, annealing at 55℃ for 2 min, extension at 72℃ for 3 min, and a final extension at 72℃ for 7 min. The amplified products were digested with HinfI (New England Biolabs, Beverly, MA, U.S.A.) at 37℃ for 4 hr. The C-to-T transition creates a new HinfI site. Digested products were electrophoresed in 3% agar gel.
The following clinical chemistry variables were determined in serum by standard enzymatic methods: total cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides, glucose, uric acid, creatinine, urea, total protein, alanine aminotransferase, aspartate aminotransferase, γ-glutamyltranspeptidase, and alkaline phosphatase. A whole blood cell count was taken for each subjects.
For statistical purposes, all variables showing a non-Gaussian distribution were logarithmically transformed. Analysis of variance (ANOVA) and Scheff's F-test were used to compare the means of subjects classified according to MTHFR genotype. The odds ratio (OR) and 95% confidence interval (95% CI) were calculated to estimate the relative risk of hyperuricemia associated with the MTHFR genotype. Study variables were correlated with uric acid levels, using Pearson's correlation coefficient test or Spearman's correlation coefficient by rank test.
To allow for the independent contribution of MTHFR genotype and other variables to serum uric acid, multiple regression analysis were performed, including some of the variables significantly associated with serum uric acid in univariate analysis. In the analysis, MTHFR genotypes were designated as follows: C/C=0, C/T=1, T/T=2 (10). Other variables are presented as continuous form. Analyses were performed using SPSS 10.1 (U.S.A.) and Epi-Info 2002 (WHO).
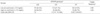
The distribution of physical and biochemical variables, in subjects classified by MTHFR genotype, is shown in Table 1. For all variables, except for uric acid and creatinine, no significant differences were found between the MTHFR genotype subjects groups.
The serum uric acid levels for each genotype are shown in Table 2. The serum uric acid levels differed significantly in subjects with different MTHFR genotypes (F=7.555; p=0.001). Homozygotes for the MTHFR mutation had a significantly higher mean uric acid level (6.33±0.97 mg/dL mean±SD) than those without (5.54±1.26 mg/dL Scheffe's F-test, p=0.005), whereas heterozygotes had an intermediate value (5.91±1.18 mg/dL). Thus, a trend towards an increasing uric acid level was observed as the number of T allele copies increased.
As shown in Table 2, subjects were classified into two groups based on uric acid levels: a low uric acid group (<7.0 mg/dL) and a high uric acid group (≥7.0 mg/dL). The value of 7.0 mg/dL represents the upper limit of the normal range of serum uric acid in all males in our laboratory, and thus was chosen as a cut-off value. The genotype frequencies differed significantly between these two groups (χ2=9.44; df=2; p=0.009). The T allele frequency was also significantly greater in the high uric acid group than in the low uric acid group (χ2=8.76; df=1; p=0.003).
The calculated odds ratios and the 95% CIs for the C/T and the T/T genotypes were 2.10 (1.13-3.95) and 3.33 (1.29-8.61), versus the C/C genotype (Table 3). Both of these effects were significant (p=0.01 and p=0.005), suggesting that the T allele has a codominant effect on the risk of hyperuricemia.
Univariate analysis, serum uric acid is correlated with MTHFR genotype (number of copies of T allele per subject), BMI, diastolic blood pressure, triglycerides, blood glucose, total protein, creatinine, blood urea nitrogen, and hematocrit. No relationship was found between the uric acid level and other factors (age, total cholesterol, HDL-cholesterol, total protein, HbA1c (%), alkaline phosphatase, alcohol, and smoking).
To exclude possible biases caused by the presence of subjects with hypertension, diabetes mellitus or impaired glucose tolerance, hypercholesterolemia, or hyperglyceridemia, subjects with each of these conditions were left out of the list in turn. Leaving out subjects with any of these conditions did not change the results as to MTHFR genotype. The correlation coefficients between MTHFR genotype and uric acid level fluctuated between 0.195 and 0.237, but p values remained below 0.001.
To assess the independent contribution of the variables to serum uric acid levels, multiple regression analysis was performed, which included all variables significantly associated with serum uric acid by univariate analyses. As shown in Table 3, MTHFR, BMI, diastolic blood pressure, log-triglycerides, and creatinine were found to be independently associated with serum uric acid levels, whereas, systolic blood pressure, blood glucose, total protein and hematocrit did not.
Frosst et al. proposed the C677T MTHFR mutation as a candidate for cardiovascular disease risk (11). However, the majority of studies and a recent meta-analysis of more than 6000 genotyped patients and controls have failed to confirm this (14). We presumed that the C677T MTHFR mutation could exert its atherogenic role at least partially by association with other recognized risk factors.
Motti et al. found a relationship between the C677T MTHFR mutation and serum uric acid (10). Their data shows that, increases in homocysteine in subjects with the C677T MTHFR mutation are paralleled by increases in serum uric acid levels. However, their subjects were an inseparable mixture of genders and ages; though higher uric acid levels were found in men (18).
In our study of Korean elderly men, a dose-dependent relationship was found between the number of copies of the T allele of the MTHFR gene and serum uric acid concentration (Table 1). Compared with the low uric acid group, the prevalence of the T/T genotype and the frequency of the T allele were higher in the group with elevated uric acid levels. The calculated odds ratio and 95% CI of hyperuricemia showed an increased risk of the C/T and T/T genotypes, rather than the C/C genotype (Table 2). Multivariate analysis also demonstrated that the C677T MTHFR mutation is an independent predictor of hyperuricemia (Table 3).
Serum uric acid is usually considered a marker of renal dysfunction, and a risk factor of renal disease progression. In addition, more recent studies suggest that elevated serum uric acid predict cardiovascular disease and cerebrovascular accidents (15-21). Although uric acid was thought to be an inert endproduct of purine metabolism, and without physiological significance, except in gouty diathesis.
Possible mechanisms underlying these associations may be presented. First, adenosine originating from S-adenosyl-homocysteine, and preferentially incorporated into a precursor pool for uric acid, would link the syntheses of homocysteine and uric acid (9). Second, in subjects with the T/T genotype, renovascular atherosclerosis or the complications of systemic vascular disease may reduce the renal clearance of uric acid, resulting in elevated serum uric acid (10). Therefore, the MTHFR mutation may be a risk factor that is involved in multiple metabolic pathways related to vascular diseases.
However, it remains a matter of debate as to whether uric acid is an independent predictor of mortality in patients with cardiovascular disease, or whether it represents only an indirect marker of adverse outcome by reflecting the association between uric acid and other cardiovascular risk factors
In this study, by comparing serum uric acid levels with the C677T MTHFR mutation, and with other variables by univariate analysis and multiple regression analysis. Five factors were found to be associated with hyperuricemia: the C677T MTHFR mutation, diastolic blood pressure, creatinine, triglycerides, and BMI. Compared with these factors, itself, may contribute less to hyperuricemia, because it showed a lower standard partial regression coefficient to serum uric acid.
To prevent cardiovascular disorders in those who carry the C677T MTHFR mutation, supplementation with folate, vitamin B6 and vitamin B12 has been recommended (22), because inter-individual variation in homocysteine levels are related to other biological traits. The regulation of homocyteine is an example of a nutritional/genetic interaction, in which dietary habits (i.e. the intake of folic acid) play an important role, in addition, to strategies aimed at lowering serum uric acid levels, such as weight control and reducing the intake of foods containing purines.
The present study shows that mutation of the MTHFR gene may be a risk factor for hyperuricemia in the Korean elderly population. In addition, the study identifies four other factors associated with hyperuricemia. Thus, we propose the probable need for a medical management strategy for those who are homozygous for the C677T MTHFR mutation, and the need for additional longitudinal study to determine the mechanism and role of uric acid as a risk factor of cardiovascular disease.
Figures and Tables
References
1. Mudd SH, Levy HL, Skovby F. Scriver CR, Beaudet AL, Sly WS, Valle D, editors. Disorders of transsulphuration. The metabolic basis of inherited disease. 1989. 1:6th ed. New York, NY: McGraw Hill International Book Co;693–734.
2. Wu AH, Tsongalis GJ. Correlation of polymorphisms to coagulation and biochemical risk factors for cardiovascular diseases. Am J Cardiol. 2001. 87:1361–1366.

3. Andreassi MG, Botto N, Cocci F, Battaglia D, Antonioli E, Masetti S, Manfredi S, Colombo MG, Biagini A, Clerico A. Methylenetetrahydrofolate reductase gene C677T polymorphism, homocysteine, vitamin B12, and DNA damage in coronary artery disease. Hum Genet. 2003. 112:171–177.

4. Grillo LB, Acacio GL, Barini R, Pinto W Jr, Bertuzzo CS. [Mutations in the methylene-tetrahydrofolate reductase gene and Down syndrome]. Cad Saude Publica. 2002. 18:1795–1797.
6. Kang SS, Wong PW, Cook HY, Norusis M, Messer JV. Protein-bound homocysteine. A possible risk factor for coronary artery disease. J Clin Invest. 1986. 77:1482–1486.

7. Coull BM, Malinow MR, Beamer N, Sexton G, Nordt F, de Garmo P. Elevated plasma homocysteine concentration as a possible independent risk factor for stroke. Stroke. 1990. 21:572–576.

8. Evers S, Koch HG, Grotemeyer KH, Lange B, Deufel T, Ringelstein EB. Features, symptoms, and neurophysiological findings in stroke associated with hyperhomocysteinemia. Arch Neurol. 1997. 54:1276–1282.

9. Malinow MR, Levenson J, Giral P, Nieto FJ, Razavian M, Segond P, Simon A. Role of blood pressure, uric acid, and hemorheological parameters on plasma homocyst(e)ine concentration. Atherosclerosis. 1995. 114:175–183.

10. Motti C, Gnasso A, Bernardini S, Massoud R, Pastore A, Rampa P, Federici G, Cortese C. Common mutation in methylenetetrahydrofolate reductase. Correlation with homocysteine and other risk factors for vascular disease. Atherosclerosis. 1998. 139:377–383.

11. Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, Boers GJ, den Heijer M, Kluijtmans LA, van den Heuvel LP, Rozen R. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet. 1995. 10:111–113.

12. Park KS, Podskarbi T, Yoo EA, Shin YS. The C677T mutation in the methylenetetrahydrofolate reductase gene in Koreans. Korean J Genet. 1998. 20:23–28.
13. Kim NK, Kang GD, Kim HJ, Kim SH, Nam YS, Lee SM, Chung HM, Kang SH, Ahn JY, Choi BO, Hwang SG, Oh DY. Genetic polymorphisms of 5,10-methylene-tetrahydrofolate reductase (MTHFR C677T and A1298C) in healthy Korean. Korean J Genet. 2002. 24:227–234.
14. Brattstrom L, Wilcken DE, Ohrvik J, Brudin L. Common methylenetetrahydrofolate reductase gene mutation leads to hyperhomocysteinemia but not to vascular disease: the result of a meta-analysis. Circulation. 1998. 98:2520–2526.
15. Persky VW, Dyer AR, Stamier J, Idris-soven E, Shekelle RB, Schoenberger JA, Berkson DM, Lindberg HA. Uric acid: a risk factor for coronary heart disease. Circulation. 1979. 59:969–977.

16. Okada M, Ueda K, Omae T, Takeshita M, Hirota Y. The relationship of serum uric acid to hypertension and ischemic heart disease in Hisayama population. J Chronic Dis. 1982. 35:173–178.
17. Brand FN, McGee DL, Kannel WB, Stokes J III, Castelli WP. Hyperuricemia as a risk factor of coronary heart disease: the Framingham study. Am J Epidemiol. 1985. 121:11–18.

18. Freedman DS, Williamson DF, Gunter EW, Byers T. Relation of serum uric acid to mortality and ischemic heart disease. The NHANES I Epidemiologic Follow-up Study. Am J Epidemiol. 1995. 141:637–644.
19. Wannamethee SG, Shaper AG, Whincup PH. Serum urate and the risk of major coronary heart disease events. Heart. 1997. 78:147–153.

20. Lehto S, Niskanen L, Ronnemaa T, Laakso M. Serum uric acid is a strong predictor of stroke in patients with non-insulin-dependent diabetes mellitus. Stroke. 1998. 29:635–639.

21. Culleton BF, Larson MG, Kannel WB, Levy D. Serum uric acid and risk for cardiovascular disease and death: the Framingham Heart Study. Ann Intern Med. 1999. 131:7–13.

22. Malinow MR. Homocyst(e)ine and arterial occlusive disease. J Intern Med. 1994. 236:603–617.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download