Abstract
The aim of this study is to characterize the epidemiological features of typhoid fever, categorized as class 1 notifiable disease in Korea and to analyze the recent change of antimicrobial resistance of Salmonella enterica serotype Typhi isolated nationwide. We retrospectively analyzed the 1,692 culture-proven cases from 1992 to 2000, using the data of the Korean National Institute of Health. The overall incidence of culture-proven typhoid fever was 0.41 per 100,000 population. It occurred all over the country, but the southeastern part of Korean peninsula had the higher incidence rate than other areas. There were several outbreaks suspected, of which two outbreaks were confirmed. The resistance rate against chloramphenicol showed mild increase, but the ampicillin, trimethoprim/sulfamethoxazole, kanamycin, or nalidixic acid resistance remained at the similar levels for the past 9 yr. There were 21 (1.3%) multidrug-resistant (MDR) strains isolated since 1992, and the number of those has increased. Two strains resistant to ciprofloxacin were first identified in Korea.
Typhoid fever is an endemic disease in the developing world; an estimated 16 million cases occur each year resulting in 700,000 deaths (1). An appropriate antibiotics is essential for the treatment of typhoid fever. Until the mid-1970s chloramphenicol was the drug of choice for typhoid fever, and resulted in a marked reduction in mortality from 10% to <2% in developed countries. Unfortunately, a few sporadic isolations of chloramphenicol-resistant Salmonella enterica serotype Typhi were reported from Chile and Kuwait before 1970, and multidrug resistant S. enterica Typhi emerged in the Indian subcontinent in 1987 (2). After introduction of ciprofloxacin, it is used extensively for the treatment of typhoid both in the developing and developed countries. Thus, recent emergence of S. enterica Typhi isolates with decreased susceptibility to ciprofloxacin has been gaining worldwide attention (3, 4).
Typhoid fever is one of class 1 notifiable diseases in Korea. It has decreased remarkably since the mid-1970s, but over two hundred cases of typhoid fever have still been reported nationwide each year (5). Ciprofloxacin is recommended as the drug of choice for typhoid fever since the 1990s. The epidemiologic features of typhoid fever and the antimicrobial resistance of the pathogens were expected to change recently with the improvement of hygiene and widespread use of antimicrobials in Korea. Thus, we performed this study to characterize the recent epidemiological features of typhoid fever in Korea, and to analyze the change of antimicrobial susceptibility of S. enterica Typhi isolated nationwide for recent 9 yr.
A retrospective analysis was performed for the culture-proven cases nationwide from 1992 to 2000, using the database of the Korean National Institute of Health (KNIH). Because typhoid fever is categorized as a class 1 notifiable disease in Korea, proved cases by culture or clinically suspected cases of typhoid fever are supposed to be reported from the medical facilities nationwide. Culture-proven cases were defined as the patients in which S. enterica Typhi was isolated from any specimen in a hospital or a public health center or Insitutue of Health & Environment of each province. Clinically suspected cases were the reported patients which showed the clinical manifestations of typhoid fever and were reported to the KNIH, but S. enterica Typhi failed to be isolated from their specimens. The Laboratory of Enteric Pathogens in KNIH has collected the demographic data and isolates of the reported cases. Collected isolates were cultured again and analyzed for microbial characteristics including antibiotic resistance information. Using these data collected from 1992 to 2000, patient's age, gender, place of residence, date of disease occurrence, Vi phage type of the bacteria, and antimicrobial susceptibility were studied.
A total of 1,692 isolates were available for this analysis. Antimicrobial susceptibility tests were available for 1,561 of 1,692 cases. Among 1,561 isolates, 31 strains, all were from 1992, were excluded because of the incomplete data for the analysis. Thus, a total of 1,530 isolates were studied. S. enterica Typhi isolates were tested for susceptibility to antimicrobials by a controlled disk diffusion technique according to the guidelines provided by the National Committee for Clinical Laboratory Standards (6). The antibiotic discs contained ampicillin (10 µg), kanamycin (30 µg), streptomycin (10 µg), tetracycline (30 µg), chloramphenicol (30 µg), trimethoprim/sulfamethoxazole (SXT-TMP) (1.25/23.75 µg), nalidixic acid (30 µg), and ciprofloxacin (5 µg). Phage typing was performed as described previously (7), with the phage set provided by the Central Public Health Laboratory at London, United Kingdom.
Multidrug-resistant (MDR) strains were defined as resistant to ampicillin, chloramphenicol, and SXT-TMP.
Using the population of 1996 as a reference, we estimated the incidence of culture-proven typhoid fever (/100,000 population/year), and described it by the year, region, seasons, and personal characteristics such as age and gender. We also compared the numbers of culture-proven cases with the clinically suspected cases notified to the KNIH. Score test for trend was used to investigate the trends of resistance rate of several antimicrobials for the isolates as time passed (8). The SAS system for Windows (release 6.12, The SAS Institute Inc., Cary, NC, U.S.A.) was used for all statistical analyses.
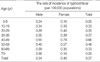
The incidence of culture-proven typhoid fever for recent 9 yr was 0.41 per 100,000 persons per year. Annual rate of incidence varied from 0.23 to 0.80 per 100,000 persons (Table 1). The number of cases in which the pathogens were proved in the KNIH was 55.9% of all clinically suspected cases since 1992 (a total of 2,837 cases). The proportions of culture-proven cases among clinically suspected cases were from 38.7% to 77.2% each year. The incidence, based on the clinically suspected cases, was 0.74 per 100,000 persons per year.
We analyzed the occurrence of culture-proven typhoid fever by age, gender, regions, and seasons. The infection occurred most frequently in the age group of forties, followed by the fifties, thirties, and twenties (Table 2). The incidence of women was slightly higher than that of men (men, 0.34 per 100,000 persons; women, 0.40). The difference of incidence for the gender was prominent in the age group of twenties, forties and fifties.
Table 1 shows the incidence rate of culture-proven typhoid fever by year and residence of patients. The data showed that the infection occurred in all over the country, but the southeastern part of Korean peninsula, such as Gyeongbuk, Gyeongnam, and Busan, had the higher rate of incidence than other areas. The annual incidence rate of the infection from different regions showed certain level of fluctuation; those of Seoul in 1998, Gangwon in 1995, Busan in 1996, Jeonnam in 1993 and 1998, Jeonbuk in 1996, Chungnam in 1999, and Chungbuk in 1994 showed more than 2-fold of overall incidence rate in each region for 9 yr. Among them, the epidemic outbreaks of typhoid fever were confirmed in Busan (9) and Jeonbuk in 1996 (10). This suggests that outbreaks of typhoid fever occurred in many regions although the outbreaks were not noticed.
The incidence of culture-proven typhoid fever showed a clear seasonal clustering. In most years, the incidence rate was low in winter (November to February), increased gradually from March, and reached its peak from April to June (Fig. 1). However, the incidence rate in summer (July to September) was unexpectedly low in most years. A very large peak in summer of 1996 was because of the previously reported outbreak in Busan (9), and the second small peak in 1996 was also because of the known outbreak in Jeonbuk (10).
Among 1,530 strains, 595 (44.3%) were isolated from blood and 724 (54.0%) were isolated from stool. The ratio of the specimen from which the pathogen was isolated was similar each year except 1992 and 1999, in which there were more stool isolates (79.2% and 80.7%, respectively).
Among 1,530 isolates, 617 isolates (40.3%) were resistant to 1 or more antibiotics, and 21 (1.3%) were multidrug-resistant (MDR) strains, defined as resistant to ampicillin, chloramphenicol, and SXT-TMP. The overall resistance rate against chloramphenicol, ampicillin, SXT-TMP, tetracycline, streptomycin, or kanamycin was 5.0%, 3.3%, 1.7%, 8.5%, 34.3%, or 1.1%, respectively. For 8 yr, the resistance to ampicillin, SXT-TMP, or kanamycin remained quite stable and the tetracycline resistance was stable except in 1995 (Table 3). However, the streptomycin resistance showed abrupt drop from 60% before 1997 to 1.4% in 2000. In case of chloramphenicol, the increase of resistance rate was statistically significant as time passed (score test for trend, p<0.05).
The resistance rate of nalidixic acid was 3.1% overall, but showed a fluctuation up to 6% in 1998 (Table 3). However, nalidixic acid resistance did not show the significant increase for recent 8 yr although it had a tendency to increase. It should be observed further for several years to come. In 1999, two strains which showed a resistance to ciprofloxacin were isolated for the first time in Korea. Two isolates showed different antimicrobial resistance patterns; one was resistant to streptomycin and kanamycin, and the other was resistant to SXT-TMP, ampicillin, streptomycin and kanamycin. But both strains were sensitive to chloramphenicol.
MDR strain resistant to ampicillin, SXT-TMP, and chloramphenicol was identified in 1992, and the number of MDR isolates gradually increased thereafter; one in 1992, two in 1995, 8 in 1997, 3 in 1998, and 7 in 1999. The isolates from 1992, 1995, 1997, and 1998 had the same antimicrobial resistance patterns; resistant to ampicillin, chloramphenicol, streptomycin, tetracycline and SXT-TMP. Six of 7 strains in 1999 were resistant to 5 antimicrobials above and kanamycin. The strains were identified to contain the resistance plasmid harboring a novel multidrug resisistance class 1 integron (11). Regional distribution of these strains isolated in 1999 dispersed all over the country; two in Gyeonggi, one in Gangwon, Gyeongnam, Gyeongbuk, and Chungbuk.
We analyzed the antimicrobial resistance by the specimen from which the pathogen was isolated and by the region of occurrence. There was no significant difference of antimicrobial resistance according to the specimen. When looking at the resistance against each antimicrobial by the region of occurrence, there was no clear clustering (no data shown). But 8 isolates of MDR S. enterica Typhi were isolated in Gyeonggi area in 1997 with the same antimicrobial resistance patterns (resistant to ampicillin, chloramphenicol, streptomycin, SXT-TMP, and tetracycline) and two bacteriophage types, A or E1.
Predominant Vi phage types were E1 (23.7%), M1 (18.8%), untypable (20.8%), and degraded (15.1%). There was considerable diversity in proportion of each phage type year by year (Fig. 2A). For example, common phage types were degraded type (37.6%), M1 (24.8%), and E1 (22.7%) in 1995 but E1 (33.5%), untypable (30.6%) and D1 (16.33%) in 1996. Regional distribution of each phage type was also very diverse (Fig. 2B). Isolates from Jeonbuk were nearly all D1 (90.6 %). E1 (39.8%) and untypable (22.8%) were common in isolates from Busan. However, the proportion of phage type A has a tendency to increase steadily.
The antimicrobial susceptibility by the phage type was similar in most of Vi phage types. It was noted, however, that the resistance rates against ampicillin (7.9%), chloramphenicol (19.1%), and nalidixic acid (9.0%) were higher in isolates with phage type A than overall resistance rates. Among 21 MDR strains, E1 was most common (9 strains), then phage type A (4 strains), M1 (3 strains), and untypable (2 strains).
Our study provides comprehensive information on the incidence of typhoid fever and antimicrobial resistance of S. enterica Typhi isolates in Korea. The incidence rate of clinically suspected typhoid fever has been greatly decreased from 10 per 100,000 persons in the 1970s to below 1 per 100,000 persons in the 1990s as results of improved sanitation and hygiene, vaccines, and effective antimicrobial chemotherapy in Korea (12). However, the annual rate of incidence has not been stable from 0.23 per 100,000 persons to 0.80 in our study based on the culture-proven cases. If the estimated reporting rate of class I notifiable disease (71.0%) is applied to total culture-proven cases (13), the actual incidence rate of typhoid would be 0.58 per 100,000 persons per year in the 1990s.
The southeastern provinces in Korea had a higher incidence rate of this disease in most years of study. The reason might be related with contamination of drinking water or the distribution of chronic carriers. According to the epidemiological investigation for a large outbreak in Busan, in 1996, the source of infection was the tap water supplied through local pumping station (9). Further investigation is needed to explain this geographic distribution of typhoid fever.
The analyses of annual incidence rate in a region suggested that the infection occurred sporadically in most regions and years. However, although the large outbreaks in Busan and Jeonbuk were confirmed, smaller-sized outbreaks might be passed unnoticed. In 1997, 8 MDR strains isolated in Gyeonggi area had the same antimicrobial resistance patterns and two bacteriophage types. This also suggests the spread of the MDR strains in that area. Thus, the early detection system should be set up in Korea in order to find out such outbreaks as early as possible.
The increase of MDR S. enterica Typhi is a great problem in developing countries. The incidence rates of MDR strains were 26% in U.K. and 17% in U.S.A., but most infections have been in patients with a recent history of travel to India or Pakistan (14, 15). In India, 64.5% of S. enterica Typhi was MDR in 1993 (16). Recently, S. enterica Typhi with decreased susceptibility to ciprofloxacin has been increasing worldwide (15, 17). In 1999, 23% of the strains in U.K. exhibited decreased susceptibility to ciprofloxacin, and 60% of the isolates in India had MIC of 2 µg/mL or greater for ciprofloxacin (15, 17). Our data show that MDR S. enterica Typhi strains are not popular yet in Korea, and the isolates resistant to nalidixic acid do not seem to be increasing. However, the recent increase of the number of MDR isolates and emergence of ciprofloxacin resistance should be concerned.
Multidrug-resistance was known to be mediated by a large-sized conjugable plasmids (18-20), and several reports suggested the international transfer of R-plasmids (19, 20). The previous pulsed-field gel electrophoresis (PFGE)-based studies of S. enterica Typhi from southeast Asia demonstrated considerable genetic diversities associated with sporadic cases and outbreaks, which suggested the movement of MDR strains within endemic regions (18-22). These findings implicated that MDR pathogens spread both by clonal spread or transfer of R-plasmid in a society. Further genotypic studies are needed to analyze the spread of MDR strain in Korea.
In conclusion, although overall incidence of typhoid fever has not increased significantly since 1992, we noticed the appearance of S. enterica Typhi resistant to all first-line drugs used for treatment of typhoid in Korea. Since strains resistant to ciprofloxacin were also identified, surveillance for resistance to first-line antibiotics and quinolones should be performed.
Figures and Tables
Fig. 1
Monthly occurrence of culture-proven typhoid fever for recent 9 yr in Korea. The incidence reached its peak from April to June every year, and there were two outbreaks confirmed in 1996.

ACKNOWLEDGEMENT
This study was supported by a grant of the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (01-PJ1-PG3-20500-0064).
References
1. Hart CA, Kariuki S. Antimicrobial resistance in developing countries. Br Med J. 1998. 317:647–650.

2. Rowe B, Ward LR, Threlfall EJ. Multidrug-resistant Salmonella typhi: a worldwide epidemic. Clin Infect Dis. 1997. 24:Suppl 1. S106–S109.

3. Herikstad H, Hayes P, Mokhtar M, Fracaro ML, Threlfall EJ, Angulo FJ. Emerging quinolone-resistant Salmonella in the United States. Emerg Infect Dis. 1997. 3:371–372.

4. Threlfall EJ, Ward LR, Skinner JA, Smith HR, Lacey S. Ciprofloxacin-resistant Salmonella typhi and treatment failure. Lancet. 1999. 353:1590–1591.

5. Communicable Dieases Monthly Report. 1990. Seoul: The Korean National Institute of Health;28–29.
6. Performance standards for antimicrobial disk susceptibility test. Standards NCfCL. 1984. Vol. 4:369–406.
7. Kim HH, Park MS, Kim SH, Yu JY, Chung BK, Lee BK. Epidemiological characteristics of Salmonella strains isolated in Korea in 1997. Korean J Vet Public Health. 1998. 22:253–260.
8. Armitage P, Berry G. Statistical methods in medical research. 1994. Oxford; Boston: Blackwell Scientific Publications.
9. Shin HR, Suh BS, Song JB, Lee DH, Lee MB, Park JH, Kim MS, Shin YH, Lee SW, Ohrr HC. An epidemiological investigation of typhoid fever outbreak in Pusan, 1996. Korean J Epidemiol. 1997. 19:122–130.
10. Lee DS, Oh HT, Han DH, Ann BY, Kim SH, Kim KW, Kim YS, Park MS. A clinical and epidemiological analysis on an outbreak of typhoid fever during 1996 summer through autumn in Chunju area. Korean J Infect Dis. 1998. 30:54–60.
11. Pai H, Byeon JH, Yu S, Lee BK, Kim S. Salmonella enterica Serovar Typhi strains isolated in Korea containing a multidrug resistance class 1 integron. Antimicrob Agents Chemother. 2003. 47:2006–2008.

12. Kim J. Health and Diseases of Korean People. 2001. Seoul, Korea: SinGwang Publishing Co..
13. Shin E. Estimation of reporting rate of notifiable acute communicable diseases and characteristics related to reporting in Korea. J Catholic Medical College. 1996. 49:1197–1209.
14. Ackers ML, Puhr ND, Tauxe RV, Mintz ED. Laboratory-based surveillance of Salmonella serotype Typhi infections in the United States: antimicrobial resistance on the rise. JAMA. 2000. 283:2668–2673.
15. Threlfall EJ, Ward LR. Decreased susceptibility to ciprofloxacin in Salmonella enterica serotype typhi, United Kingdom. Emerg Infect Dis. 2001. 7:448–450.
16. Pillai PK, Prakash K. Current status of drug resistance & phage types of Salmonella typhi in India. Indian J Med Res. 1993. 97:154–158.
17. Chitnis V, Chitnis D, Verma S, Hemvani N. Multidrug-resistant Salmonella typhi in India. Lancet. 1999. 354:514–515.

18. Hampton MD, Ward LR, Rowe B, Threlfall EJ. Molecular fingerprinting of multidrug-resistant Salmonella enterica serotype Typhi. Emerg Infect Dis. 1998. 4:317–320.

19. Mirza S, Kariuki S, Mamun KZ, Beeching NJ, Hart CA. Analysis of plasmid and chromosomal DNA of multidrug-resistant Salmonella enterica serovar Typhi from Asia. J Clin Microbiol. 2000. 38:1449–1452.

20. Shanahan PM, Jesudason MV, Thomson CJ, Amyes SG. Molecular analysis of and identification of antibiotic resistance genes in clinical isolates of Salmonella typhi from India. J Clin Microbiol. 1998. 36:1595–1600.

21. Connerton P, Wain J, Hien TT, Ali T, Parry C, Chinh NT, Vinh H, Ho VA, Diep TS, Day NP, White NJ, Dougan G, Farrar JJ. Epidemic typhoid in Vietnam: molecular typing of multiple-antibiotic-resistant Salmonella enterica serotype Typhi from four outbreaks. J Clin Microbiol. 2000. 38:895–897.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download