A 72-year-old man with hypertension was referred to our hospital for severe aortic regurgitation probably associated with quadricuspid aortic valve on transthoracic echocardiography. He felt general fatigue on effort. On physical examination, blood pressure was 166/54 mm Hg and cardiac auscultation indicated a systolic murmur at the aortic area together with a diastolic murmur at the left parasternal border. Value of brain natriuretic peptide was 258.5 pg/mL, and values of cardiac enzymes were within normal limits. An electrocardiogram showed left ventricular high voltage in addition to ST-segment depression in II, III, aVF, and V6 leads. Subsequent transthoracic echocardiography revealed decreased motion in the inferoposterior wall of the dilated left ventricle (end-diastolic and end-systolic diameters of 6.3 and 4.6 cm, respectively; ejection fraction 49 %, Simpson's method) and severe aortic regurgitation (vena contracta 6.7 mm, pressure half time 279 msec, regurgitant volume 77 mL on the proximal isovelocity surface area method, and effective regurgitant orifice area 0.38 cm2) with probable quadricuspid aortic valve. Two- and three-dimensional transesophageal echocardiography clearly depicted a quadricuspid asymmetric aortic valve with a large right coronary cusp, two intermediate cusps including left coronary cusp and non-coronary cusp, and a smaller accessory cusp (Hurwitz and Roberts' classification, type D), and a severe aortic regurgitation due to the central coaptation defect (Fig. 1A, B, and C, Supplementary movie 1, 2, and 3). Pre-operative cardiac catheterization was performed (Fig. 2). Coronary angiography showed a severe stenosis in the distal segment of the right coronary artery (Fig. 2A). Left coronary artery was normal (Fig. 2B). On aortography, aortic regurgitation of Sellers grade 3, left ventricular end-diastolic volume of 263 mL, end-systolic volume of 142 mL, ejection fraction of 46%, and hypokinesis in inferior were observed (Fig. 2C and D). During right heart catheterization, course of Swan-Ganz catheter suggested a presence of left-sided inferior vena cava (IVC). Hemodynamics study showed left ventricular end-diastolic pressure of 14 mm Hg, mean pulmonary capillary wedge pressure of 15 mm Hg, mean pulmonary artery pressure of 19 mm Hg, and cardiac index of 2.38 L/min/m2. Computed tomography (CT) prior to the surgery confirmed a left-sided IVC (Fig. 3). Based on the diagnosis of severe aortic regurgitation with quadricuspid aortic valve and coronary artery disease, the patient underwent an aortic valve replacement using a bioprosthetic valve (Carpentier-Edwards PERIMOUNT Magna Ease 23 mm; Edwards Lifesciences, Irvine, CA, USA) and coronary artery bypass grafting surgery (aorta-saphenous vein graft-posterolateral branch) on the 4th hospital day. The right coronary cusp occupied approximately one-third of the aortic valve annulus area, and the accessory cusp was located between the left and non-coronary cusps, consistent with the transesophageal echocardiographic findings (Fig. 1D and E). Degenerative changes of the aortic valve leaflets were mild. After rehabilitation, he was discharged without complications on the 16th hospital day and has since been free of symptoms.
Quadricuspid aortic valve is an extremely rare appearance of congenital valvular malformation with an estimated incidence of < 0.05% of all congenital heart disease,1)2) and according to the recent report from Mayo Clinic, 26% of the patients with quadricuspid aortic valve had moderate or severe aortic regurgitation.2) Accumulating case reports have demonstrated usefulness of 2- and 3-dimensional transesophageal echocardiography in the diagnosis and the exact delineation of the mechanism of the regurgitation.3) This aortic valvular malformation is commonly associated with other congenital cardiovascular disorders, such as coronary artery anomalies, atrial septal defect, ventricular septal defect, patent ductus arteriosus, or anomalous systemic venous connections.2)4) On the other hand, most of cases with left-sided IVC are asymptomatic and incidentally depicted on ultrasound or CT imaging; however, clinical significance of left-sided IVC includes increased risks of bleeding during abdominal surgery, particularly right-sided deep vein thrombosis, complications associated with IVC filter implantation, nutcracker phenomenon leading to renal venous hypertension, and misdiagnosis as lymphadenopathy on imaging modalities.5) To the best of our knowledge this is the first report to document a unique case of quadricuspid aortic valve with left-sided IVC. It is of great importance to depict any systemic vascular anomalies associated with quadricuspid aortic valve preoperatively to prevent critical complications.
Figures and Tables
 | Fig. 1Quadricuspid aortic valve with severe aortic regurgitation. A and B: Two-dimensional transesophageal echocardiography images during diastolic phase (A, short-axis view; B, long-axis view). C: Three-dimensional transesophageal echocardiography images (left, diastolic; right, systolic). D: Intraoperative photograph showing quadricuspid aortic valve and left main ostium (white arrow). The accessory cusp was located between the left coronary cusp and the non-coronary cusp. E: Surgically resected leaflets of the quadricuspid aortic valve showing 1 larger cusp (R), 2 intermediate cusps (L and N), and 1 smaller cusp (Ac), corresponding to type D based on the Hurwitz and Roberts' classification. Ac: accessory cusp, L: left coronary cusp, N: non-coronary cusp, R: right coronary cusp. |
 | Fig. 2Pre-operative cardiac catheterization. Coronary angiography (CAG) (A, right CAG; B, left CAG) and aortography (C, end-diastolic; D, end-systolic) depicted a significant stenosis in the distal segment of right coronary artery and aortic regurgitation of Sellers grade 3, respectively. |
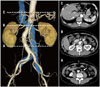 | Fig. 3Pre-operative computed tomography images indicating the left-sided inferior vena cava (IVC) (left: reconstructed 3-dimensional image, right: transverse image). The IVC (white arrows) ran upward along the left side of the aorta (A), crossed the aorta anteriorly through the meso-aortic angle (B), and communicated with a normally positioned infra-hepatic IVC (C). |
References
1. Feldman BJ, Khandheria BK, Warnes CA, Seward JB, Taylor CL, Tajik AJ. Incidence, description and functional assessment of isolated quadricuspid aortic valves. Am J Cardiol. 1990; 65:937–938.
2. Tsang MY, Abudiab MM, Ammash NM, Naqvi TZ, Edwards WD, Nkomo VT, Pellikka PA. Quadricuspid aortic valve: characteristics, associated structural cardiovascular abnormalities, and clinical outcomes. Circulation. 2016; 133:312–319.
3. D'Aloia A, Vizzardi E, Bugatti S, Chiari E, Repossini A, Muneretto C, Dei Cas L. A quadricuspid aortic valve associated with severe aortic regurgitation and left ventricular systolic dysfunction. Eur J Echocardiogr. 2009; 10:724–725.
4. Brugts JJ, Cuypers JA, Polak P, Ouhlous M, van de Woestijne P, Wessels M, Roos-Hesselink J. Quadricuspid aortic valve and anomalous systemic venous connection in a patient with cat-eye syndrome. Circulation. 2015; 131:1225–1227.
5. Ang WC, Doyle T, Stringer MD. Left-sided and duplicate inferior vena cava: a case series and review. Clin Anat. 2013; 26:990–1001.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download