Abstract
In this report, we present a case of 35-year-old lady who had presented with atypical chest pain and exertional breathlessness for past six months. Transthoracic and transesophageal echocardiograms showed a well-circumscribed, echo-dense mass in the right atrium, attached to the interatrial septum at the level of atrioventricular junction and in the vicinity of coronary sinus ostium. She underwent successful resection of the cardiac mass. Histopathology revealed paraganglioma, which was reconfirmed by immunohistochemistry study. This represents an extremely rare presentation as primary cardiac tumors are 20-times less common than metastatic tumors and paraganglioma is one of the rarest primary cardiac tumors, accounting for < 1% of all cases.
Intracardiac masses are commonly encountered clinical entity and include thrombi, vegetations, tumors, inflammatory granuloma, etc. Among cardiac tumors, most are metastatic tumors as primary cardiac tumors are 20-times less common. Although the definite diagnosis of a cardiac tumor can be established only after surgical resection, certain epidemiological and morphological features can help in differential diagnosis of primary cardiac tumors. Myxomas are easiest to diagnose pre-operatively due to their much higher prevalence and characteristic echocardiographic appearance. However, rarely, some other cardiac tumors can present in a similar manner resulting in misdiagnosis. We hereby describe a case of a young lady who presented with a right atrial paraganglioma, an extremely rare primary cardiac tumor,1) masquerading as a myxoma.
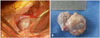
A 35-year-old lady presented to the hospital with atypical chest pain and exertional breathlessness for past six months. Physical examination revealed a pulse rate of 90 bpm, and respiratory rate of 24 breaths/min; other physical findings were normal. Electrocardiography revealed normal sinus rhythm with T-wave inversion in leads III and aVF. The chest radiograph was unremarkable. Transthoracic echocardiogram revealed a 1.9 × 2.4 cm well-circumscribed, sessile, echo-dense mass in the right atrium, attached to the interatrial septum (Fig. 1A, Supplementary movie 1). The mass was located near the atrioventricular junction. The mass did not cause any obstruction to right ventricular inflow. There was no tricuspid regurgitation or any other major abnormality. Transesophageal echocardiography was performed to better delineate the mass. It showed a larger mass (2.4 × 3.7 cm) than seen with transthoracic echocardiography (Fig. 1B). The mass was attached near the coronary sinus ostium without causing obstruction to coronary sinus flow. Multiple views of the mass showed hyperechoic tissue density, except for a small area of central echolucency (Supplementary movie 2). Her inferior vena cava was clear. Computed tomography of abdomen was also normal. Although the homogeneous echodensity of the mass was suggestive of a solid tumor, a presumptive diagnosis of right atrial myxoma was made due to its characteristic location of interatrial septum, high prevalence of atrial myxomas and the patient's clinical profile.
After detailed preoperative analysis and planning, open-heart surgery for tumor resection was performed on the 3rd day of hospitalization. Intraoperatively, a 2.5 × 3.5 cm sized, firm, encapsulated, smooth tumor was seen arising from the area between the annulus of the septal leaflet of tricuspid valve and the posterior margin of coronary sinus ostium (Fig. 2). Complete resection of the mass was achieved.
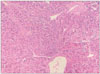
Histopathology of the excised mass using conventional hematoxylin and eosin staining revealed homogeneous polygonal cells with moderately pleomorphic nucleoli and moderate eosinophilic cytoplasm. There was scant mitosis with no necrosis. The cell nests were separated by hyalinised fibrous stroma which was rich in vasculature. These features were highly suggestive of a paraganglioma (Fig. 3). The histopathology findings were confirmed by immunohistochemistry using several special stains. The tumor tissue was diffusely positive for chromogranin (Fig. 4A) and synaptophysin (Fig. 4B) with patchy focal positivity for CD56.
The patient was discharged in stable condition with no recurrence of the tumor 4 months later.
Most cardiac tumors are metastatic tumors and only < 5% are primary cardiac neoplasms. Myxomas are the most common primary cardiac tumors whereas paragangliomas are amongst the rarest, accounting for <1% of all cases.1)2)
Paraganglioma is a tumor of neural crest origin and is similar to a pheochromocytoma. For this reason, paragangliomas are also known as ‘extra-adrenal pheochromocytoma’. Mediastinal paragangliomas can be either intracardiac or extracardiac and arise from autonomic neural tissue in these organs. Intracardiac paragangliomas have been found mostly in the left atrium and less commonly in the interatrial septum, left ventricle, anterior surface of the heart, right ventricular outflow tract, or very rarely, right atrium.3) To our knowledge, only few cases of right atrial paraganglioma have been described in the world medical literature so far.1)4)5)6)7)8)9)
Clinically, cardiac paragangliomas can present either with symptoms of adrenergic excess or with mass effect.4)7)9) Mass effect depends on the location and the size of the tumor in relation to cardiac structures. Thus, the patients can present with acute coronary syndrome (compression of coronary ostium), heart failure (valvular obstruction), syncope (valvular obstruction, compression of great vessels), etc.4)5) Rarely, these tumors may also remain completely asymptomatic.
Diagnosis of paragangliomas is most often established after surgical resection only as there are no specific echocardiographic features. However, in catecholamine secreting tumors, preoperative diagnosis is important because surgical resection of such tumors without prior pharmacological conditioning can lead to disastrous consequences during the immediate postoperative period. Measurement of plasma metanephrine levels may help in preoperative diagnosis of such tumors.
Surgical resection is the primary therapeutic approach for paragangliomas. Surgery can be quite challenging in these cases due to vascularity of these tumors and their proximity with vital structures. For obvious reasons, mediastinal and cardiac paragangliomas are among the most technically demanding to resect.10) After surgical resection, long-term follow-up is essential, as paragangliomas can recur many years after initial surgery.10)
Our patient did not have any significant mass effect due to the tumor. Further, she probably had a non-secreting tumor because she was not complaining of any symptoms suggestive of catecholamine excess such as hot flush, sweating, headache or intermittent palpitation. Unfortunately, as we did not suspect paraganglioma in this case, we did not check for urine and serum metanephrine levels. However, in hindsight, we realized that measurement of urine and serum catecholamines should be performed in all primary cardiac tumors, particularly when tumor presents with atypical features and the diagnosis is not readily apparent.
Figures and Tables
Fig. 1
Echocardiographic images of the right atrial mass. Transthoracic echocardiogram (A) and transesophageal echocardiogram (B).

References
1. Tahir M, Noor SJ, Herle A, Downing S. Right atrial paraganglioma: a rare primary cardiac neoplasm as a cause of chest pain. Tex Heart Inst J. 2009; 36:594–597.
2. Maxey TS, Grow P, Morris CD, Patton KT, Guyton RA. Biatrial primary cardiac paraganglioma: a rare finding. Cardiovasc Pathol. 2007; 16:179–182.
3. Jeevanandam V, Oz MC, Shapiro B, Barr ML, Marboe C, Rose EA. Surgical management of cardiac pheochromocytoma. Resection versus transplantation. Ann Surg. 1995; 221:415–419.
4. Okum EJ, Henry D, Kasirajan V, Deanda A. Cardiac pheochromocytoma. J Thorac Cardiovasc Surg. 2005; 129:674–675.
5. Kennelly R, Aziz R, Toner M, Young V. Right atrial paraganglioma: an unusual primary cardiac tumour. Eur J Cardiothorac Surg. 2008; 33:1150–1152.
6. Hayek ER, Hughes MM, Speakman ED, Miller HJ, Stocker PJ. Cardiac paraganglioma presenting with acute myocardial infarction and stroke. Ann Thorac Surg. 2007; 83:1882–1884.
7. Brown IE, Milshteyn M, Kleinman B, Bakhos M, Roizen MF, Jeevanandam V. Case 3--2002. Pheochromocytoma presenting as a right intra-atrial mass. J Cardiothorac Vasc Anesth. 2002; 16:370–373.
8. Palubinskas AJ, Roizen MF, Conte FA. Localization of functioning pheochromocytomas by venous sampling and radioenzymatic analysis. Radiology. 1980; 136:495–496.
9. Kawasuji M, Matsunaga Y, Iwa T. Cardiac phaeochromocytoma of the interatrial septum. Eur J Cardiothorac Surg. 1989; 3:175–177.
10. Joynt KE, Moslehi JJ, Baughman KL. Paragangliomas: etiology, presentation, and management. Cardiol Rev. 2009; 17:159–164.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download