Abstract
Patients undergoing total joint arthroplasty frequently develop post-operative complication, such as deep vein thrombosis and pulmonary thromboembolism. However, it is not common coexisting deep vein thrombosis, pulmonary thromboembolisms, right atrial thrombus and acute cerebral infarction raised by thrombus through patent foramen ovale. We reported the patient who had multiple thrombi which were accompanied with a cryptogenic ischemic stroke and associated with patent foramen ovale after operation.
Venous thromboembolism (VTE) occurs to be one of the most serious complications after undergoing total joint arthroplasty.1) Generally, pulmonary thromboembolism is generated as the secondary by-product from deep vein thrombosis (DVT) while its emergence may possibly trigger the chronic thromboembolic pulmonary hypertension as well as post-thrombotic syndrome.2) Patent foramen ovale (PFO), a residue of fetal circulation, is found approximately about 25-30% among adults; and, it is also known that thrombus from the venous circulation rarely causes arterial thromboembolism through right-to-left shunt.3) In this case, the authors experienced a patient with PFO and several thrombotic disease such as pulmonary thromboembolism, DVT, and right atrial thrombus along with cryptogenic ischemic stroke after total knee arthroplasty (TKA).
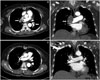
A 64-year-old female presented to the emergency room for the shortness of breath. She underwent a left total knee replacement 3 weeks ago at other hospital. She had been taking antiplatelet drugs (aspirin 100 mg/day, clopidogrel 75 mg/day) for the treatment of the right posterior temporal lobe infarction detected in brain magnetic resonance imaging for the disorientation on the third day after the operation (Fig. 1). Carotid and brain computed tomography (CT) angiography showed no evidence of atherosclerosis. Afterwards, she experienced dyspnea in the second week after the operation and was performed the transthoracic echocardiography (TTE), which showed right atrial thrombi and was treated with the low molecular weight heparin (LMWH). The symptoms, nonetheless, remained so that she had been transferred to our hospital. In the medical history she was being treated with medication for hypertension and diabetes. Preoperative electrocardiogram (ECG) and TTE were normal. At the hospitalization, her blood pressure was 127/79 mm Hg while her heart rate was 89 bpm. On physical, pitting edema in her left lower leg was noted and neurologic examination was unremarkable. The chest X-rays did not show any signs of cardiomegaly as well as pulmonary edema. Both d-dimer and N-terminal pro-brain natriuretic peptide were increased respectively at 2686 ng/mL, and 3310 pg/mL and on the other hand, cardiac enzymes, such as creatinine kinase-MB and troponin-I were within a normal range. TTE demonstrated normal left ventricular systolic function (ejection fraction of 63%), but in the right atrium two highly mobile masses (1.67 × 2.18 cm, 0.69 × 0.80 cm) suggesting possible thrombi were observed. The echocardiogram also revealed right atrium and right ventricle enlargement, severe pulmonary hypertension (pulmonary artery systolic pressure 102 mm Hg), and D-shaped left ventricle (Fig. 2). Her chest CT showed that pulmonary thromboembolism was found in both main pulmonary arteries while DVT was observed in left femoral vein (Fig. 3). 24-hour Holter ECG did not reveal arrhythmia except rare atrial premature complex and ventricle premature complex. The patient was administered to warfarin (target INR 2-3) after using LMWH. In follow-up TTE 3 weeks later, the two previous thrombi in right atrium (RA) disappeared. Along with the improvement in RA, there was also a positive change on the extent of pulmonary hypertension. The follow up CT taken 4 weeks after the hospitalization did not reveal pulmonary thromboembolism and DVT (Fig. 3). Since the cause of the cerebral infarction was unclear, additional evaluation were needed. In order to examine the intracardiac shunt, TTE was performed on the 5th week. The agitated saline test was also conducted along the way. The results confirmed the transference of microbubble from right atrium to left atrium without showing atrial septal defect; and therefore, we diagnosed the patient with PFO (Fig. 4). Currently, the patient is taking warfarin continuously without any signs of abnormalities in outpatient clinic. We recommended further treatment for PFO including device closure but patient refused because of poor general condition.
As VTE is one of the fatal complications after undergoing TKA, DVT, and pulmonary embolism (PE) are known to occur approximately around 13% and 3%, respectively.4) The occurrence period of VTE after TKA is reported to be 3 to 9 days after the operatio5) and, there are mostly cases that accompany DVT and PE and occasionally thrombi observed on several organs. Particularly, it was reported that the patients with PFO even might develop arterial thromboembolism with cryptogenic stroke.3)6)
In the present case, the authors suspected that cryptogenic stroke 3 days after the operation might possibly have been caused by the VTE changed into arterial thromboembolism through PFO.
PFO, one of the congenital heart diseases that can be observed even in adulthood, typically have no symptom. Nonetheless, it can affect as the risk factor for several conditions including ischemic stroke, platypnea-orthodeoxia syndrome, and decompression sickness.7) PFO as the cause of cryptogenic stroke is not uncommon; hence, the occurrence of ischemic stroke with either PE or DVT can be considered as the possible example of paradoxical embolism through right-to-left shunt.8)
Among the treatments on the prevention of frequent strokes within a patient who has PFO, there are medical options and invasive methods.9)
The medical options include the use of antiplatelet agents as well as the prescription of warfarin in the patients with hypercoagulable state or venous thrombosis. In terms of invasive methods, it was used to have an operation in the past while the application of device closure is being used recently.10) In this case, cryptogenic stroke took place within 3 days after TKA while right atrial thrombus, DVT, and PE were present in a way that the passage through right to left shunt was speculated and the result of subsequent echocardiography led to the diagnosis of a positive reaction from the agitated saline test for PFO. The patient was treated with LMWH and then administered warfarin; and the patient discharged with the recovered conditions.
In conclusion, the occurrence of pulmonary thromboembolism or DVT in a patient with PFO can trigger the development of cryptogenic stroke through right to left shunt.
Therefore, further evaluation of cause are essential in patients with the occurrence of cryptogenic stroke who are associated with a high risk of VTE after total joint arthroplasty. Also, anticoagulation treatment is necessary if a patient has a right to left shunt, such as PFO.
Figures and Tables
Fig. 1
An embolic infarction in right posterior temporal lobe is seen in diffusion brain magnetic resonance imaging (arrow).

Fig. 2
Transthoracic echocardiographic finding. A: D-shaped left ventricle is seen in the short axis view. B: Two thrombi (arrows) are present in the right atrium; and, the size of right atrium and right ventricle is enlarged (in four chamber view). C: Tricuspid regurgitation and severe pulmonary hypertension (pulmonary artery systolic pressure 102 mm Hg) are shown in the Doppler echocardiogram. D: Inferior vena cava is dilated (in subcostal view).

References
1. Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, Colwell CW. American College of Chest Physicians. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133:6 Suppl. 381S–453S.
2. Goldhaber SZ, Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet. 2012; 379:1835–1846.

4. Watanabe H, Sekiya H, Kariya Y, Hoshino Y, Sugimoto H, Hayasaka S. The incidence of venous thromboembolism before and after total knee arthroplasty using 16-row multidetector computed tomography. J Arthroplasty. 2011; 26:1488–1493.

5. Warwick D, Friedman RJ, Agnelli G, Gil-Garay E, Johnson K, FitzGerald G, Turibio FM. Insufficient duration of venous thromboembolism prophylaxis after total hip or knee replacement when compared with the time course of thromboembolic events: findings from the Global Orthopaedic Registry. J Bone Joint Surg Br. 2007; 89:799–807.
6. Park MS, Park JP, Yun SH, Lee JU, Kim JK, Lee NE, Song JE, Lee SE, John SH, Lim JH, Rhew JY. A case of cryptogenic stroke associated with patent foramen ovale coexisting with pulmonary embolisms, deep vein thromboses, and renal artery infarctions. Korean Circ J. 2012; 42:853–856.

7. Drighil A, El Mosalami H, Elbadaoui N, Chraibi S, Bennis A. Patent foramen ovale: a new disease? Int J Cardiol. 2007; 122:1–9.

9. Sacco RL, Adams R, Albers G, Alberts MJ, Benavente O, Furie K, Goldstein LB, Gorelick P, Halperin J, Harbaugh R, Johnston SC, Katzan I, Kelly-Hayes M, Kenton EJ, Marks M, Schwamm LH, Tomsick T. American Heart Association. American Stroke Association Council on Stroke. Council on Cardiovascular Radiology and Intervention. American Academy of Neurology. Guidelines for prevention of stroke in patients with ischemic stroke or transient ischemic attack: a statement for healthcare professionals from the American Heart Association/American Stroke Association Council on Stroke: co-sponsored by the Council on Cardiovascular Radiology and Intervention: the American Academy of Neurology affirms the value of this guideline. Stroke. 2006; 37:577–617.

10. Windecker S, Wahl A, Nedeltchev K, Arnold M, Schwerzmann M, Seiler C, Mattle HP, Meier B. Comparison of medical treatment with percutaneous closure of patent foramen ovale in patients with cryptogenic stroke. J Am Coll Cardiol. 2004; 44:750–758.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download