Abstract
The optimal treatment for free-floating massive right heart thrombi remains uncertain. However, they appear to increase the risk of mortality compared to the existence of a solitary pulmonary thromboembolism. Thrombolytic therapy has been shown to be effective in most patients, resulting in complete resolution of the massive thrombus and clinical improvement. We report the echocardiographic disappearance of a free-floating right heart thrombus after thrombolysis, however, the thrombus migrated and resulted in pulmonary thromboembolism. It was successfully removed with surgery.
Massive free-floating thrombi in the right heart (FFTRH) are uncommon and incidentally diagnosed when image studies are performed in patients with suspected or proven pulmonary thromboembolism (PTE), and they increase the risk of mortality compared to the presence of PTE alone.1)2) A massive FFTRH is relatively unstable, and migration toward the pulmonary trunk is often fatal.3)4) However, there is no clear consensus regarding the optimal management of FFTRH. We herein present the case of a patient with the echocardiographic disappearance of a FFTRH after thrombolysis. However, the FFTRH migrated, resulting in massive PTE, and was successfully removed surgically.
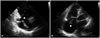
A 74-year-old woman presented at our emergency room with sudden-onset dyspnea. Her blood pressure was 70/50 mmHg, and her heart rate was 140 beats/min at that time. The electrocardiogram showed sinus tachycardia and ST-T wave depression in leads V1 to V3. Chest computed tomography showed filling defects in the right ventricle (RV) and both pulmonary arteries (Fig. 1). Echocardiography was then performed immediately and showed a D-shaped left ventricular cavity with enlargement of the right atrium (RA) and RV. In addition, a free-floating and thread-like echogenic material attached to the tricuspid valve was observed (Fig. 2A, Supplementary movie 1). Laboratory data showed normal white blood cell and platelet counts, the aspartate aminotransferase level was elevated to 210 IU/L (normal values: 13-33 IU/L), and the lactate dehydrogenase level was increased to 469 IU/L (normal values: 119-229 IU/L). In addition, both D-dimer (56 µg/mL, normal values: less than 0.5 µg/mL) and B-type natriuretic peptide (230 pg/mL, normal values: less than 99 pg/mL) were also elevated. Immediately, the recombinant tissue plasminogen activator (Actylase®, Boehringer Ingelheim, Ingelheim, Germany) 100 mg was intravenously received and followed by 18000 U per day unfractionated heparin infusion. After the administration of thrombolytic agents, no free-floating, rod-shaped materials were observed within the RA and RV, and only the thread-like echogenic material attached to the tricuspid valve was found to be improved (Fig. 2B, Supplementary movie 2), but RV dysfunction persisted. However, the patient's blood pressure was not restored with inotropic agents, and cardiac arrest occurred. An emergency cardiopulmonary bypass was performed, including a right atriotomy; no FFTRH was identified in the RA or RV cavity, including the tricuspid valve (Fig. 3A). However, the massive thrombus and FFTRH were extracted from the bilateral pulmonary arteries under direct vision using forceps inserted through a longitudinal incision in the main pulmonary artery (Fig. 3B). The postoperative course of this patient was stable without recurred PTE.
The optimal management of life-threatening FFTRH remains uncertain despite the availability of several different treatment modalities.1)5)6) Previous reports have demonstrated that thrombolytic therapy can be administered quickly and results in a good prognosis, and it is therefore advocated as an initial treatment.7)8) However, thrombolytic therapy may lead to thrombus fragmentation.9) In addition, a small, single-center, nonrandomized trial did not show any advantage of thrombolysis over surgical embolectomy.6) We report a case of migrated PTE with a large, entrapped FFTRH. Based on the follow-up echocardiography after thrombolysis, the FFTRH was considered to be resolved. However, thrombolysed thrombi that were not observed had migrated, and a fragmented thromboembolism was detected in the pulmonary arteries in the surgical field. When compared to conservative treatment including the thrombolysis of a massive FFTRH, particularly in the past few decades, surgical embolectomy was rarely reported to have lower mortality rates, a lower number of hemorrhagic events or recurrent thrombosis.10) Recently, surgical embolectomy was also strictly recommended to those in whom thrombolytic treatment has not improved hemodynamic status.11) In our case, we successfully performed surgical embolectomy in a patient with a FFTRH and an acute massive migrated PTE with hemodynamic collapse and RV dysfunction. Poor result after thrombolysis in our case may be due to massive preexisting thrombus. However, surgical embolectomy may be the more preferred therapeutic option for FFTRH due to the potential of massive thrombus fragmentation and migration.
Figures and Tables
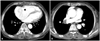
Fig. 1
The initial chest CT showed the free-floating thrombi (arrow) in the right heart (A) and in the pulmonary arteries (B). CT: computed tomography.
References
1. Chartier L, Béra J, Delomez M, Asseman P, Beregi JP, Bauchart JJ, Warembourg H, Théry C. Free-floating thrombi in the right heart: diagnosis, management, and prognostic indexes in 38 consecutive patients. Circulation. 1999. 99:2779–2783.
2. Casazza F, Bongarzoni A, Centonze F, Morpurgo M. Prevalence and prognostic significance of right-sided cardiac mobile thrombi in acute massive pulmonary embolism. Am J Cardiol. 1997. 79:1433–1435.

3. Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet. 1999. 353:1386–1389.

4. Sokmen G, Sokmen A, Altun B. Free floating right atrial thrombus leading to acute pulmonary embolism. Int J Cardiol. 2008. 129:e12–e14.

5. Rose PS, Punjabi NM, Pearse DB. Treatment of right heart thromboemboli. Chest. 2002. 121:806–814.

6. Pierre-Justin G, Pierard LA. Management of mobile right heart thrombi: a prospective series. Int J Cardiol. 2005. 99:381–388.

7. Goldhaber SZ. Optimal strategy for diagnosis and treatment of pulmonary embolism due to right atrial thrombus. Mayo Clin Proc. 1988. 63:1261–1264.

8. Cuccia C, Campana M, Franzoni P, Faggiano P, Volterrani M, Musmeci G, Visioli O. Effectiveness of intravenous rTPA in the treatment of massive pulmonary embolism and right heart thromboembolism. Am Heart J. 1993. 126:468–472.

9. Armstrong WF, Feigenbaum H, Dillon JC. Echocardiographic detection of right atrial thromboembolism. Chest. 1985. 87:801–806.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download