Abstract
Background
To determine sensitivity and specificity of E wave velocity in patients with severe chronic organic mitral regurgitation (MR) and normal left ventricular ejection fraction (EF) and to evaluate prevalence of A wave dominance in patients with severe MR.
Methods
We compared 35 patients with quantified severe, chronic, quantified, organic MR due to flail/prolapsed leaflets who had reparative surgery with 35 age-matched control subjects. Exclusion criteria: EF < 60%, atrial fibrillation, and more than mild aortic regurgitation.
Results
Mean [standard deviation (SD)] age [70 (8) years vs. 69 (8) years; p = 0.94] and mean (SD) EF [66% (6%) vs. 65% (4%); p = 0.43] were not different between the two groups. Mean (SD) E wave velocity was greater in case patients than control subjects [1.2 (0.3) m/sec vs. 0.7 (0.15) m/sec; p < 0.001]. However, E wave velocity of 1.2 m/sec had a sensitivity of only 57% [95% confidence interval (CI), 41-7 and a specificity of 100% (95% CI, 90-100%) in identifying severe MR. E wave velocity of 0.9 m/sec had a more optimal combined sensitivity (89%; 95% CI, 74-95%) and specificity (86%; 95% CI, 71-94%). A wave dominance was seen in 18% of case patients and 66% of control subjects (p < 0.001).
Conclusion
E wave velocity of 1.2 m/sec is specific not sensitive for severe organic MR; E wave velocity of 0.9 m/sec has better sensitivity and specificity. A wave dominance pattern alone cannot exclude patients with severe organic MR. Our findings highlight the importance of a comprehensive echocardiographic exam rather than relying on a few Doppler parameters in diagnosing MR.
Mitral regurgitation (MR) is commonly found on echocardiography and is usually hemodynamically insignificant. However, severe MR needs immediate attention, especially in patients with organic mitral valve disease with a repairable valve because these patients may benefit from early surgery.1) Although quantitation of all detected MR is ideal, such quantitation is impractical, given the large number of patients with some degree of MR. Therefore, some authors have suggested using mitral E wave velocity and the E wave to A wave ratio (E/A) as the screening tools to rapidly exclude patients without severe MR.2) On the basis of a limited number of studies, American Society of Echocardiography (ASE) guidelines stated that, "In severe MR without stenosis, the mitral E velocity is higher than the velocity during atrial contraction (A velocity) and is usually greater than 1.2 m/sec. A mitral inflow pattern with an A-wave dominance virtually excludes severe MR".3) In addition, the European Association of Echocardiography suggests that "In the absence of mitral stenosis, a peak E wave velocity > 1.5 m/sec suggests severe MR. Conversely, a dominant A wave virtually excludes severe MR".4)
However, the studies evaluating the utility of E wave velocpity have not included many patients with severe MR due to flail mitral valve leaflets and requiring surgery, thereby making the conclusions of the studies less strong.2) In addition to MR, E wave velocity is dependent on several factors, including abnormal relaxation and high left ventricular filling pressures. Not infrequently, patients with severe organic MR due to flail leaflets have lower-than-expected E wave velocity or a dominant A wave pattern, or both, on their mitral inflow in our clinical practice. We hypothesized that the accepted mitral E velocity of 1.2 m/sec has low sensitivity to exclude severe MR and mitral A wave dominance pattern alone cannot exclude severe MR in all patients.
We retrospectively reviewed medical records of patients aged 18 years and older who underwent a transthoracic echocardiogram and subsequent mitral valve surgery for mitral valve disease at Mayo Clinic in Arizona between 1987 and 2010. We included only those patients with normal left ventricular ejection fraction (EF) who underwent surgery because of quantified severe MR due to either mitral valve prolapse or flail mitral valve leaflet. We excluded patients who did not have a transthoracic echocardiogram within 1 year of surgery; did not undergo surgery; had an EF less than 60%; had greater than mild valvular stenosis or regurgitation in the aortic, pulmonic, or tricuspid valves; were paced due to an implanted pacemaker; were in atrial fibrillation; had poor-quality images; and had any congenital abnormality, including atrial septal defect and hypertrophic obstructive cardiomyopathy.
A total of 35 patients were ultimately selected from 300 patients who eventually met the inclusion and exclusion criteria and constituted the final study group. These patients were compared to 35 age-matched control subjects selected sequentially from patients who underwent echocardiographic study at our institution, were in sinus rhythm, and had either no or only mild valvular regurgitation and a normal left ventricular EF.
Standard comprehensive 2-dimensional Doppler echocardiographic examinations were performed using a commercially available system-Sequoia C512 (Siemens AG, Oceanside, CA, USA) or Vivid 7 (GE Healthcare, Waukesha, WI, USA). The quantification of severe MR was in accordance with the recommendations from the ASE.3)
Briefly, the concept of proximal isovelocity surface area (PISA) is based on flow convergence proximal to the regurgitant orifice.5)6) The blood accelerates as it enters a regurgitant orifice and produces a series of shells. Applying the principle of conservation of mass, the regurgitant flow rate and regurgitant volume can be calculated.7) The following additional standard echocardiographic data were also evaluated in each patient: EF, left ventricular end diastolic and systolic dimensions, E wave velocity, A wave velocity, tissue Doppler on lateral and septal annulus, pulmonary vein velocities, E wave to average annular velocity ratio (E/e'), E/A ratio, right ventricular systolic pressure. Mitral inflow analysis was performed by placing the sample volume at the mitral leaflet tips in the apical four chamber view and obtaining continuous and pulsed wave Doppler.2)
Continuous variables were expressed as mean and standard deviation (SD); categorical variables were expressed as number and percentage. Difference between groups was assessed with the 2-sample t-test or Wilcoxon rank sum test for continuous data. For categorical data, the χ2 test was used. Linear regression was used to determine whether the E/A correlated with the E/e'. Receiver operating curves and optimal sensitivity and specificity cutoff points were chosen using logistic regression models. Corresponding 95% confidence intervals (CI) were derived using standard binomial distribution methods. A p value less than 0.05 was considered statistically significant. All analyses were performed using JMP version 8.0.2 software (SAS Institute Inc., Cary, NC, USA).
Baseline characteristics of the case patients are shown in Table 1. The mean age of the controls was 70 ± 8 years versus mean age in cases was 69 ± 8 years (p = 0.94). Of note, many patients with severe MR were asymptomatic (40%) at surgery, however met the criteria suggested by the American College of Cardiology to undergo surgery.8) All patients had elective surgery and the median duration between the echocardiogram and cardiac surgery was 54 days. Only one patient had an echocardiogram done the day of his elective cardiac surgery and it was done to reconfirm the severity of MR that noted on his echocardiogram 11 months prior. Mean (SD) MR volume was 80 (17) mL and the effective regurgitant orifice was 0.51 (0.14) cm2 in case patients. Table 2 shows no significant difference in age and EF among case patients and control subjects. Left ventricular end-diastolic dimension and left ventricular end-systolic dimension were greater in cases than controls, as expected. Our study population consisted of 71% males and 29% females and the male population had a higher left ventricular end-diastolic dimension (LVEDD) (56 ± 7 mm) (mean ± SD) when compared to females where the mean LVEDD (50 ± 7 mm) (mean ± SD) (p = 0.04). In addition, average E wave velocity was significantly higher in the case patients than control subjects (Table 2), as were the left atrial volume index and right ventricular systolic pressure.
Among patients with severe MR, mitral E wave velocity was less than 1.2 m/sec in 43% (95% CI, 28-59%) (Fig. 1). Echocardiographic images and Doppler findings of a patient who had severe MR due to flail leaflet quantified by PISA method who underwent mitral valve surgery are shown in Fig. 2. Despite severe MR, mitral inflow Doppler showed an E wave velocity of < 1.2 m/sec (Fig. 2D). Receiver operator curve showed that, although E wave velocity of more than 1.2 m/sec is highly specific (100%; 95% CI, 90-100%), it has low sensitivity (57%; 95% CI, 41-72%) to diagnose severe MR (Fig. 3). The optimal cutoff value of the E wave velocity was 0.9 m/sec, which has a sensitivity of 89% (95% CI, 74-95%) and a specificity of 86% (95% CI, 71-94%). An A wave dominant mitral inflow pattern was observed in 18% (95% CI 9-34%) of the case patients with severe MR; although the percentage of control subjects with an A wave dominant mitral inflow pattern was significantly higher (66%; 95% CI, 49-79%) (p < 0.001) (Fig. 4).
We also compared the mitral annular areas (using diameters measured at the onset of atrial contraction from the apical 2 and 4 chambers and assuming that the annulus is an ellipse) in patients with severe MR who had E wave velocities of 1.2 m/sec or greater to those who had E wave velocities of less than 1.2 m/sec. We found no significant difference between the mitral annular areas in these groups [40.0 (7.0) cm2 vs. 40.0 (12.0) cm2; p = 0.98].
When examining mitral regurgitant volume in those patients
with severe MR and an E wave velocity greater than 1.2 m/sec and those who had severe MR and an E wave velocity less than 1.2 m/sec there was no significant difference in the regurgitant volume between the 2 groups: 81 (16) mL vs. 78 (19) mL, respectively (p = 0.61).
Our study, consisting of patients with quantified severe chronic, organic, quantified mitral valve regurgitation due to either flail mitral valve leaflets or mitral valve prolapse requiring surgery, shows that although E wave velocity of 1.2 m/sec is highly specific for severe organic MR, it is not sensitive enough (57%) to exclude severe MR and thus is less likely to be useful as a screening tool. An E wave velocity of 0.9 m/sec may be more useful because of optimal sensitivity (89%) and specificity (86%). In addition, an A wave-dominant pattern alone cannot exclude patients with severe organic MR because 18% of patients with severe MR in our study were found to have an A wave-dominant pattern.
MR is a progressive disease and the timing of surgery is crucial since delaying mitral valve surgery can lead to left ventricular dysfunction and decreased long-term survival.9-11) In fact, the American College of Cardiology states that surgery should be considered even in asymptomatic patients who meet certain criteria.8) Similarly the European Society of Cardiology guidelines suggest that the management of asymptomatic patients with mitral valve regurgitation is controversial, however these patients require careful serial follow-up and surgery should be considered early once certain parameters are met.12) Thus, a reliable, yet efficient, method is crucial for quantifying the severity of MR.
Several qualitative measures have been proposed, including continuous wave Doppler jet density and pulmonary vein flow patterns.3) Quantitative methods include calculation of regurgitant volume and effective regurgitant orifice area.3) Although these methods are well validated in several studies, they are time consuming and may not be the ideal screening method for excluding patients with severe MR.
Early mitral inflow velocity reflects the instantaneous pressure difference between the left atrium and the left ventricle.13) In severe MR, the pressure gradient between the left atrium and left ventricle increases and leads to a higher peak E wave velocity. However, several other factors also affect E wave velocity, such as preload, blood pressure, rate of relaxation of the left ventricle, compliance of both the left atrium and the left ventricle, and the left ventricular end-systolic volume.14-16) The clinician cannot truly rely on E wave velocity in excluding those with severe MR.
In a similar manner, the left atrium of young, healthy patients can contribute as much as 30% to left ventricular filling during diastole.16) On pulsed wave Doppler, the A wave (associated with atrial contraction) has been shown to increase with aging, including a decrease in E/A ratio due to impaired left ventricular relaxation.17) However, it also has been proposed that A wave dominance virtually excludes severe MR.2)
A study by Thomas et al.2) found that a peak mitral inflow velocity of more than 1.2 m/sec identified patients who had severe MR with a sensitivity of 85% and a specificity of 86%. This study also found that no patient with severe MR had an A wave-dominant mitral inflow pattern. However, their study did not specifically include many patients with severe MR due to flail mitral valve leaflets or mitral valve prolapse requiring surgery (n = 8). In contrast, our study included only patients with quantified severe MR due to flail mitral valve leaflet or mitral valve prolapse (as seen during surgery) (n = 35). Our analysis showed that E wave velocity of 1.2 m/sec has good specificity, yet poor sensitivity, in predicting severe MR. In fact, our study showed that an E wave velocity of 0.9 m/sec has better sensitivity and specificity overall in predicting severe MR.
To understand why severe MR results in an E wave velocity less than 1.2 m/sec and to determine if perhaps an enlarged annulus could contribute to these findings, we compared the mitral annular areas (using diameters measured at the onset of atrial contraction from the apical 2 and 4 chambers and assuming that the annulus is an ellipse) in patients with severe MR who had E wave velocities of 1.2 m/sec or greater to those who had E wave velocities of less than 1.2 m/sec. We found no significant difference between the mitral annular areas in these groups.
We also examined the mitral regurgitant volume in those patients with severe MR and an E wave velocity greater than 1.2 m/sec and those who had severe MR and an E wave velocity less than 1.2 m/sec. It may be that both E wave velocity and mitral inflow pattern (E/A) are affected by other factors, such as diastolic function and age so that in some patients, E wave velocity of 1.2 m/sec and a mitral A wave dominant pattern cannot be used as the sole factors to exclude severe MR. From a clinical standpoint, physicians should not be using an absolute value of 1.2 m/sec for the mitral E wave velocity and the A wave dominant mitral inflow pattern alone to exclude severe MR. It is prudent to not only look at the valve anatomy but to also perform comprehensive quantitation in patients with moderate or greater MR.
Our study sample was relatively small; it consisted of 35 patients with severe MR because we wanted to include only patients with severe MR due to flail mitral valve leaflets or mitral valve prolapse requiring surgery. Also we wanted to include only those patients with EF greater than 60%, those who were not paced and in normal sinus rhythm, and exclude patients who had MR from causes other than pure organic reasons (flail or prolapse), and those who did not have any other valvular diseases. This reduced our sample size down from the initial 300 patients that were screened. Thus, larger scale studies are needed to confirm our findings. However this study highlights the importance of not relying on a few parameters to evaluate severe MR and emphasizes the fact that patients should be comprehensively evaluated for severity of MR to determine timing of surgery.
In conclusion, although E wave velocity of 1.2 m/sec is highly specific for severe organic MR, it is not sensitive enough. Thus, E wave velocity of 0.9 m/sec may be more useful because of optimal sensitivity and specificity. An A wave-dominant pattern alone cannot exclude patients with severe organic MR. Our findings underscore the importance of a comprehensive echocardiographic evaluation of MR rather than relying on one or two simple Doppler measures which sometimes may be misleading.
Figures and Tables
Fig. 1
E wave velocity between patients with no or mild mitral regurgitation (MR) compared with those who have severe MR. Those with no or mild MR were more likely to have an E wave velocity less than 1.2 m/sec. However, those with severe MR were noted to have wide variations in the E wave velocity. In fact, E wave velocity greater than 1.2 m/sec was specific in eliminating severe MR, yet it was not sensitive enough because some patients with severe MR still had E wave velocities less than 1.2 m/sec. Error bars indicate the range of E wave velocities in the control group and the case group. The boxed area shows the E wave velocities of the majority of subjects.

Fig. 2
Illustrative case of a patient with ruptured chords by transthoracic (A) and transesophageal echocardiogram (B)demonstrated by the white arrows. Quantitation of mitral regurgitation by proximal isovelocity surface area method (C) showed the regurgitant volume to be 67 mL [mitral regurgitation (MR) peak velocity Doppler profile not shown]. Even though this patient had severe MR, the mitral inflow pattern did not demonstrate an E wave > 1.2 m/sec (D).

Fig. 3
Receiver operator curve. The receiver operator curve demonstrates that an E wave velocity (E) of 1.2 m/sec had good specificity but low sensitivity in identifying patients with severe mitral regurgitation. However, an E of 0.9 m/sec had better sensitivity and better specificity. AUC: area under the curve.
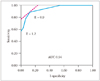
Fig. 4
A-wave dominant pattern between case patients and control patients. Patients with no or mild mitral regurgitation (MR) are more than likely to have an A wave-dominant pattern than those with severe MR. However, 18% of the patients with severe MR also showed an A wave dominance.
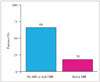
Table 2
Patient characteristics in case group vs. control group at surgery

Values are presented as mean (standard deviation) unless specified otherwise. EF: ejection fraction, LVEDD: left ventricular end-diastolic dimension, LVESD: left ventricular end-systolic dimension, E < A: E wave less than A wave, LAVI: left atrial volume index, RVSP: right ventricular systolic pressure, e': average annular velocity
References
1. Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, Detaint D, Capps M, Nkomo V, Scott C, Schaff HV, Tajik AJ. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med. 2005; 352:875–883.

2. Thomas L, Foster E, Schiller NB. Peak mitral inflow velocity predicts mitral regurgitation severity. J Am Coll Cardiol. 1998; 31:174–179.
3. Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJ. American Society of Echocardiography. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003; 16:777–802.

4. Lancellotti P, Moura L, Pierard LA, Agricola E, Popescu BA, Tribouilloy C, Hagendorff A, Monin JL, Badano L, Zamorano JL. European Association of Echocardiography. European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve disease). Eur J Echocardiogr. 2010; 11:307–332.

5. Recusani F, Bargiggia GS, Yoganathan AP, Raisaro A, Valdes-Cruz LM, Sung HW, Bertucci C, Gallati M, Moises VA, Simpson IA. A new method for quantification of regurgitant flow rate using color Doppler flow imaging of the flow convergence region proximal to a discrete orifice. An in vitro study. Circulation. 1991; 83:594–604.

6. Rodriguez L, Anconina J, Flachskampf FA, Weyman AE, Levine RA, Thomas JD. Impact of finite orifice size on proximal flow convergence.Implications for Doppler quantification of valvular regurgitation. Circ Res. 1992; 70:923–930.

7. Rokey R, Sterling LL, Zoghbi WA, Sartori MP, Limacher MC, Kuo LC, Quinones MA. Determination of regurgitant fraction in isolated mitral or aortic regurgitation by pulsed Doppler two-dimensional echocardiography. J Am Coll Cardiol. 1986; 7:1273–1278.

8. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Society of Cardiovascular Anesthesiologists. Society for Cardiovascular Angiography and Interventions. Society of Thoracic Surgeons. Bonow RO, Carabello BA, Kanu C, de Leon AC Jr, Faxon DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O'Gara PT, O'Rourke RA, Otto CM, Shah PM, Shanewise JS, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation. 2006; 114:e84–e231.
9. Crawford MH, Souchek J, Oprian CA, Miller DC, Rahimtoola S, Giacomini JC, Sethi G, Hammermeister KE. Department of Veterans Affairs Cooperative Study on Valvular Heart Disease. Determinants of survival and left ventricular performance after mitral valve replacement. Circulation. 1990; 81:1173–1181.

10. Enriquez-Sarano M, Tajik AJ, Schaff HV, Orszulak TA, McGoon MD, Bailey KR, Frye RL. Echocardiographic prediction of left ventricular function after correction of mitral regurgitation: results and clinical implications. J Am Coll Cardiol. 1994; 24:1536–1543.

11. Enriquez-Sarano M, Schaff HV, Orszulak TA, Tajik AJ, Bailey KR, Frye RL. Valve repair improves the outcome of surgery for mitral regurgitation. A multivariate analysis. Circulation. 1995; 91:1022–1028.

12. Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC). European Association for Cardio-Thoracic Surgery (EACTS). Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Iung B, Lancellotti P, Pierard L, Price S, Schafers HJ, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppell UO, Windecker S, Zamorano JL, Zembala M. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012; 33:2451–2496.

13. Appleton CP, Hatle LK, Popp RL. Relation of transmitral flow velocity patterns to left ventricular diastolic function: new insights from a combined hemodynamic and Doppler echocardiographic study. J Am Coll Cardiol. 1988; 12:426–440.

14. Choong CY, Herrmann HC, Weyman AE, Fifer MA. Preload dependence of Doppler-derived indexes of left ventricular diastolic function in humans. J Am Coll Cardiol. 1987; 10:800–808.

15. Gardin JM, Davidson DM, Rohan MK, Butman S, Knoll M, Garcia R, Dubria S, Gardin SK, Henry WL. Relationship between age, body size, gender, and blood pressure and Doppler flow measurements in the aorta and pulmonary artery. Am Heart J. 1987; 113:101–109.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download