Abstract
Background
Left atrial appendage (LAA) anatomy and function have been well characterized both in healthy and diseased people, whereas relatively little attention has been focused on the right atrial appendage (RAA). We sought to evaluate RAA flow velocity and to compare these parameters with LAA indices and with a study of biomarkers, such as brain natriuretic peptide, among patients with sinus rhythm (SR) and atrial fibrillation (AF).
Methods
In a series of 79 consecutive patients referred for transesophageal echocardiography, 43 patients (23 with AF and 20 controls) were evaluated.
Results
AF was associated with a decrease in flow velocity for both LAA and RAA [LAA velocity-SR vs. AF: 61 ± 22 vs. 29 ± 18 m/sec (p < 0.01), RAA velocity-SR vs. AF: 46 ± 20 vs. 19 ± 8 m/sec (p < 0.01)]. Based on simple linear regression analysis, LAA velocity and RAA velocity were positively correlated, and RAA velocity was inversely correlated with brain natriuretic peptide (BNP).
Atrial fibrillation (AF) is associated with serious complications such as atrial thrombosis and cerebral infarction compared with sinus rhythm (SR).1) Left atrial appendage (LAA) dysfunction is known as a significant predictor of thrombus formation.2)3) LAA anatomy and function have been well characterized both in patients with AF and with SR,4-6) whereas little attention has been focused on the right atrial appendage (RAA).
Recently, RAA thrombi7-10) and RAA function11) have been reported in patients with AF. Bilge et al.12) suggested that RAA function is also decreased in patients with AF compared to those with SR.
Therefore, we hypothesized that RAA dysfunction is associated with left ventricular dysfunction as is LAA dysfunction. In this study, RAA flow velocity and LAA flow velocity were compared among patients with AF and SR. We found that RAA flow velocity correlates with LAA flow velocity, and that RAA velocity correlates with the concentration of brain natriuretic peptide (BNP), a biochemical marker of left ventricular dysfunction.
Seventy-nine patients referred for transesophageal echocardiography were evaluated in our study from April to July 2008. Of these patients, we excluded those with valvular heart disease, malignancy, or severe congestive heart failure. A total of 43 patients including 23 AF patients and 20 control patients were enrolled in our study. Baseline clinical characteristics included age, sex, height, weight, smoking history, and the statuses of various medical conditions including systemic hypertension, diabetes, and hyperlipidemia. We defined hyperlipidemia as a triglyceride level greater than 200 mg/dL or an low-density lipoprotein level greater than 130 mg/dL.
Approval was granted by the institutional review board, and patients were required to provide informed consent.
All patients underwent both transthoracic and multiplane transesophageal echocardiography.
The studies were performed with a 3.25-MHz transthoracic transducer (Philips Medical Systems, Andover, MA, USA) with patients in the left lateral decubitus position. Transthoracic echocardiography studies were carried out according to the recommendations of the American Society of Echocardiography.13) M-mode left atrial (LA) dimension, right ventricular (RV) dimension, and interventricular septal dimension were measured in the parasternal long-axis view at end-diastole. Left ventricular end diastolic dimension, left ventricular end systolic dimension, and ejection fraction were measured in the parasternal long-axis view. Tissue velocities (E and e') were measured at septum in Doppler images, and E/e' was calculated. RV systolic pressure was calculated using the RV-right atrial pressure gradient and tricuspid regurgitation velocity.14)
Transesophageal echocardiography was performed using a commercial 2-7-MHz multiplane probe (Philips Medical Systems, Andover, MA, USA) after patient fasting. Topical lidocaine spray and viscous lidocaine solution were used to anesthetize the oropharynx before the investigation. The LAA was imaged in the basal short-axis view using a transverse scan from 0 to 45 degrees (Fig. 1). The scanning plane was rotated from 90 to 145 degrees to achieve visualization of the RAA (Fig. 2).15) Peak LAA and RAA ejection and filling velocities were measured by placing a pulsed wave Doppler sample volume just inside the base of the appendage, as suggested by Fatkin et al.4)
All blood samples were obtained the day after hospital admission and before transesophageal echocardiogram (TEE). The plasma BNP and high-sensitivity C-reactive protein (hs-CRP) concentrations were measured with an ACCESS 2 produced by Beckman Coulter and an LX20 produced by Beckman Coulter (Brea, CA, USA), respectively.
Values are expressed as mean ± SD. Continuous variables between groups were compared using student's t-test. Norminal variables between groups were compared using Chi-square test. Correlations between RAA velocities and LAA velocities and between RAA velocities and BNP were performed with a pearson's correlation analysis (version 12.0 for Windows; SPSS, Chicago, IL, USA).
The clinical characteristics for all 43 patients (mean age 64.1 ± 14.3 years), including the AF group and SR group, are shown in Table 1. There were no statistically significant differences in height, weight, or body surface area level between the AF group and SR group. Hypertension, diabetes mellitus, smoking, and hyperlipidemia were more frequently seen in the AF group than they were in the SR group.
The transthoracic echocardiographic (TTE) parameters are listed in Table 2. LA size was significantly larger among patients in the AF group than in the SR group [AF vs. SR: 4.6 ± 0.65 vs. 3.5 ± 0.78 cm (p = 0.00)]. The E/e' value was greater in the AF group [AF vs. SR: 9.35 ± 3.51 vs. 7.35 ± 2.97 (p = 39 0.059)], but it was not statistically significant. Significant differences were not seen for any other measurements.
LAA and RAA velocities according to TEE were all significantly slower in the AF group compared to those in the SR group (Table 3). The mean LAA ejection velocity (LAA E) was 29 ± 18 cm/sec in the AF group and 61 ± 22 cm/sec in the SR group (p < 0.001), and the mean LAA filling velocity (LAA F) was 33 ± 18 m/sec in the AF group and 58 ± 29 m/sec in the SR group (p < 0.001). The mean RAA ejection velocity (RAA e) and filling velocity (RAA f) were also slower in the AF group than in the SR group [AF vs. SR: 19 ± 8 vs. 46 ± 20 cm/sec (p < 0.001), 22 ± 0.12 vs. 39 ± 13 cm/sec (p < 0.001)].
There was no statistically significant difference in hs-CRP concentration between the two groups, but the BNP level was higher in the AF group than in the SR group [AF vs. SR: 301.4 ± 286.6 vs. 107.2 ± 158.3 pg/mol (p = 0.016)] (Table 4).
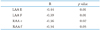
BNP concentration was negatively correlated with LAA emptying velocity (r = -0.44; p = 0.01) and with LAA filling velocity (r = -0.39; p = 0.01). BNP expression was also negatively correlated with RAA emptying velocity (r = -0.36; p = 0.02) and with RAA filling velocity (r = -0.34; p = 0.03) (Table 5). RAA velocities and LAA velocities were significantly positively correlated with each other (r = 0.53; p = 0.0, r = 0.5; p = 0.0, r = 0.62; p = 0.0, r = 0.61; p = 0.0).
Evaluation of the LAA using transesophageal echocardiography of AF is a standard procedure in patients who are in fibrillation. In 2-D imaging, potential thrombus and spontaneous echo contrast should be analyzed. A pulsed Doppler TEE analysis of LAA emptying flow should be conducted to supplement the 2-D analysis as these examinations have been shown to be highly reproducible and to help assess thromboembolic risk.16)
Mikael Kortz et al.17) found that the LAA blood flow pattern in healthy subjects was variable, changing from quadri- to tri- and biphasic with increasing heart rate. In another study, a similar relationship was also observed for the RAA.
When heart failure or hypertension occurs, one of the most important forms of remodeling is an increase in muscle mass in response to a pressure or volume overload or myocardial injury.18) In cases of ventricular remodeling, both enlargement of the myocytes and interstitial or perivascular fibrosis are observed simultaneously.
The peripheral plasma BNP concentration can be used as a biochemical marker of left ventricular dysfunction. This protein increases not only in patients with systolic dysfunction, such as in dilated cardiomyopathy, but also in patients with hypertension or hypertrophic cardiomyopathy, of which usually not involve systolic dysfunction. The plasma BNP concentration increases in proportion to the degree of left ventricular end-systolic stress and end-diastolic pressure. Patients with AF showed an inverse correlation between BNP concentration and LAA flow velocity.3)
There are few studies about the RAA, most likely because of its location and clinical importance. The RAA is a cardiac structure that is difficult to examine using TTE. However, TEE is a good tool to evaluate RAA. In 1999, Bilge et al.19) analyzed RAA blood flow patterns in normal subjects without cardiovascular disease using TEE, resulting in the first study on RAA. Since then, several studies on RAA anatomy and RAA function and its implications for thrombus formation have been reported.12)20)21)
In our study, we were able to easily examine RAA function and anatomy using TEE, especially peak emptying velocity and peak filling velocity. LAA and RAA peak emptying and filling velocities were lower in the AF group compared with those in the control group. These results suggest that AF leads to decrease not only in LA function but also in RA function. The larger E/e' in the AF group indicates that AF group has worse LV diastolic dysfunction than SR group.
BNP concentration is known to be associated with LA function.22) In our study, BNP level was correlated with LAA and RAA velocity (emptying and filling). BNP concentration may therefore correlate with RAA function.
There were several limitations to this study. First, we did not observe significant correlations between variables in patients with AF. This lack of significance may be associated with small size of the study group. Second, no hemodynamic parameters like right atrial pressure or right atrial volume were included in the analysis. Third, we could not exclude all possible heart problems which may have affected the SRs of patients used as a control group. Despite these limitations, the results of this study will serve as a very useful reference for future studies about RAA anatomy and function.
In conclusion, AF is associated with depressed RAA and LAA flow velocities and with increased LA size. RAA velocity was found to be positively correlated with LAA velocity and negatively correlated with BNP concentration. Therefore, plasma BNP concentration may serve as a determinant of LAA and RAA functions. Further study is required to determine the clinical significance of RAA.
Figures and Tables
Table 1
Baseline characteristics between SR and AF groups were compared using t-test and Chi-square test

Table 3
Comparison of appendage velocity in patients with AF and SR (transesophageal echocardiographic assessment)

References
2. Caplan LR, D'Cruz I, Hier DB, Reddy H, Shah S. Atrial size, atrial fibrillation, and stroke. Ann Neurol. 1986. 19:158–161.

3. Igarashi Y, Kashimura K, Makiyama Y, Sato T, Ojima K, Aizawa Y. Left atrial appendage dysfunction in chronic nonvalvular atrial fibrillation is significantly associated with an elevated level of brain natriuretic peptide and a prothrombotic state. Jpn Circ J. 2001. 65:788–792.

4. Fatkin D, Kelly RP, Feneley MP. Relations between left atrial appendage blood flow velocity, spontaneous echocardiographic contrast and thromboembolic risk in vivo. J Am Coll Cardiol. 1994. 23:961–969.

5. Grimm RA, Stewart WJ, Maloney JD, Cohen GI, Pearce GL, Salcedo EE, Klein AL. Impact of electrical cardioversion for atrial fibrillation on left atrial appendage function and spontaneous echo contrast: characterization by simultaneous transesophageal echocardiography. J Am Coll Cardiol. 1993. 22:1359–1366.

6. Zeppellini R, Schön F, Gheno G, Drozdz J, Balzereit A, Cucchini F, Erbel R. Left atrial appendage systolic forward flow. Am J Cardiol. 1995. 75:204–206.

7. Klein AL, Grimm RA, Jasper SE, Murray RD, Apperson-Hansen C, Lieber EA, Black IW, Davidoff R, Erbel R, Halperin JL, Orsinelli DA, Porter TR, Stoddard MF. ACUTE Steering and Publications Committee for the ACUTE Investigators. Efficacy of transesophageal echocardiography-guided cardioversion of patients with atrial fibrillation at 6 months: a randomized controlled trial. Am Heart J. 2006. 151:380–389.

8. Manning WJ, Silverman DI, Gordon SP, Krumholz HM, Douglas PS. Cardioversion from atrial fibrillation without prolonged anticoagulation with use of transesophageal echocardiography to exclude the presence of atrial thrombi. N Engl J Med. 1993. 328:750–755.

9. Manning WJ, Silverman DI, Keighley CS, Oettgen P, Douglas PS. Transesophageal echocardiographically facilitated early cardioversion from atrial fibrillation using short-term anticoagulation: final results of a prospective 4.5-year study. J Am Coll Cardiol. 1995. 25:1354–1361.

10. Stoddard MF, Dawkins PR, Prince CR, Longaker RA. Transesophageal echocardiographic guidance of cardioversion in patients with atrial fibrillation. Am Heart J. 1995. 129:1204–1215.

11. Omran H, Jung W, MacCarter D, Schimpf R, Rabahieh R, Schumacher B, Wolpert C, Becher H, Lüderitz B. Right atrial thrombi and depressed right atrial appendage function after cardioversion of atrial fibrillation. Echocardiography. 1999. 16:245–251.

12. Bilge M, Eryonucu B, Güler N, Erkoç R. Right atrial appendage function in patients with chronic nonvalvular atrial fibrillation. Jpn Heart J. 2000. 41:451–462.

13. Henry WL, DeMaria A, Gramiak R, King DL, Kisslo JA, Popp RL, Sahn DJ, Schiller NB, Tajik A, Teichholz LE, Weyman AE. Report of the American Society of Echocardiography Committee on Nomenclature and Standards in Two-dimensional Echocardiography. Circulation. 1980. 62:212–217.

14. Yock PG, Popp RL. Noninvasive estimation of right ventricular systolic pressure by Doppler ultrasound in patients with tricuspid regurgitation. Circulation. 1984. 70:657–662.

15. Seward JB, Khandheria BK, Freeman WK, Oh JK, Enriquez-Sarano M, Miller FA, Edwards WD, Tajik AJ. Multiplane transesophageal echocardiography: image orientation, examination technique, anatomic correlations, and clinical applications. Mayo Clin Proc. 1993. 68:523–551.

16. Donal E, Yamada H, Leclercq C, Herpin D. The left atrial appendage, a small, blind-ended structure: a review of its echocardiographic evaluation and its clinical role. Chest. 2005. 128:1853–1862.

17. Mikael Kortz RA, Delemarre BJ, van Dantzig JM, Bot H, Kamp O, Visser CA. Left atrial appendage blood flow determined by transesophageal echocardiography in healthy subjects. Am J Cardiol. 1993. 71:976–981.

18. Titcomb CP Jr. LVH: consequences associated with cardiac remodeling. J Insur Med. 2004. 36:42–46.
19. Bilge M, Eryonucu B, Güler N, Aşker M. Evaluation of right atrial appendage blood flow by transesophageal echocardiography in subjects with a normal heart. Jpn Heart J. 1999. 40:599–607.

20. de Divitiis M, Omran H, Rabahieh R, Rang B, Illien S, Schimpf R, MacCarter D, Jung W, Becher H, Lüderitz B. Right atrial appendage thrombosis in atrial fibrillation: its frequency and its clinical predictors. Am J Cardiol. 1999. 84:1023–1028.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download