Abstract
Background
Measurement of right ventricular (RV) systolic function is important for patients with acute pulmonary embolism (PE). However, assessment of RV function is a challenge due to its complex anatomy. We measured RV systolic function with analysis of tricuspid annular motion in acute PE patients.
Methods
From August 2007 to May 2011, all consecutive PE patients were prospectively included. Tricuspid annular motion was analyzed with tricuspid annular plane systolic excursion (TAPSE) and tricuspid annular systolic velocity (TASV).
Results
We analyzed total 50 patients (38 females, 68 ± 14 years). Mean RV fractional area change (RVFAC) was 26.2 ± 10.8%; RV Tei index 0.78 ± 0.35; TR Vmax 3.8 ± 0.5 m/sec; pulmonary vascular resistance (PVR) 3.5 ± 1.2 WU. TAPSE was 16 ± 4 mm and TASV was 11.7 ± 4.0 cm/sec. TAPSE showed significant correlations with RVFAC (r = 0.841, p < 0.001), RV Tei index (r = -0.347, p = 0.018), Log B-type natriuretic peptide (BNP) (r = -0.634, p < 0.001) and PVR (r = -0.635, p < 0.001). TASV also revealed significant correlations with RVFAC (r = 0.605, p < 0.001), RV Tei index (r = -0.380, p = 0.009), LogBNP (r = -0.477, p = 0.001) and PVR (r = -0.483, p = 0.001). The best cutoff of TAPSE for detection of RV systolic dysfunction (defined as RVFAC < 35%) was 1.75 cm [Areas under the curve (AUC) = 0.96, p < 0.001] with a sensitivity of 87% and specificity 91%. The best cutoff for TASV was 13.8 cm/sec (AUC = 0.90, p < 0.001), sensitivity 86% and specificity 78%. However, there was no statistical significance in the detection of RV dysfunction (difference = 0.07, 95% CI = -0.21-0.17, p = 0.130) between TAPSE and TASV.
Measurement of right ventricular (RV) systolic function is essential in the management and assessment of prognosis acute pulmonary embolism (PE) patients.1) The presence of RV systolic dysfunction is a major indication of thrombolytic therapy and a well-known prognostic marker in these patients.2)3) Compared to evaluation of left ventricular function, estimation of RV function is difficult due to its complex 3-dimensional geometry and nonconcentric contraction pattern.4) To overcome this difficulty, many imaging modalities including cardiac magnetic resonance imaging or RV ventriculography were used to estimate RV systolic function. Although many imaging methods can be used to evaluate RV systolic function, 2-dimensional echocardiography (2DE) is the most commonly used imaging method in the assessment of RV systolic function in acute PE. Two-DE is usually a good tool to evaluate RV function and contribute to the selection of treatment in patients with acute PE. Because the direction of RV muscle fibers predominantly runs toward longitudinally, measurement of tricuspid annular motion can be a good marker in the assessment of RV systolic function.5)6) Tricuspid annular plane systolic excursion (TAPSE) is an easily measurable index which reflects RV systolic function along the long axis and it has been shown to be closely related to the RV ejection fraction.7)8) Tricuspid annular systolic velocity (TASV) also can be easily obtained from tissue Doppler imaging analysis and it is a good indicator of RV systolic function.9)10) However, these indices of RV systolic function in patients with acute PE have not been fully studied. We measured RV systolic function with analysis of tricuspid annular motion by TAPSE and TASV in patients with acute PE.
We recruited consecutive patients with first episode of PE from August 2007 to May 2011. The diagnosis of PE was based on contrast-enhanced computerized tomography in patients with clinical suspicion of acute PE in the emergency room. Standard contrast-enhanced PE protocols were performed in patients without renal dysfunction using 16-slice (SOMATOM Sensation16, Siemens AG, Forchheim, Germany) multi-detector-row CT scanners with acquisition of 1-mm sections of the entire chest. The diagnosis of PE was confirmed in the presence of at least one filling defect in the pulmonary arterial tree including the subsegmental level. Patients with arrhythmia or inappropriate echocardiographic image quality were excluded in this study. This study was approved by the institutional review board at Chungnam National University Hospital.
Standard echocardiographic examinations with Doppler studies were performed on the day of admission using Vivid 7 or E9 (GE Vingmed, Horten, Norway). The echocardiographic images of all subjects were obtained from the parasternal and apical views. Studies were stored digitally and analyzed off-line. RV fractional area change (RVFAC) was calculated from the apical 4-chamber view using the percentage change in areas of the end-diastolic and end-systolic areas of the RV.11) TAPSE was acquired by placing an M-mode cursor through the tricuspid annulus and the distance of longitudinal movement of the annulus during systolic period was measured.11)12) RV myocardial performance (Tei) index was defined as the ratio of isovolumic relaxation time and isovolumic contraction time divided by ejection time of RV.11)12) TASV was obtained after placement of a sample volume on the tricuspid annuls at the place of attachment of the anterior leaflet of the tricuspid valve on the tissue Doppler imaging. Care was taken to obtain an ultrasound beam parallel to the direction of tricuspid annular motion.11)12) TASV was measured and digitally obtained at 100 mm/sec. Pulmonary artery systolic pressure was estimated from the maximal continuous-wave Doppler velocity of the tricuspid regurgitation (TR) jet plus estimated right atrial pressure with size of inferior vena cava and degree of change in caval diameter during respiration.11)12) An index of pulmonary vascular resistance was derived by dividing the maximal velocity of the TR jet by the RV outflow tract velocity-time integral.13) An average of 3 measurements was used. The presence of McConnell sign, normal contraction or sparing of the RV apex with hypokinesis of midportion of the RV free wall, was checked.14)
Follow-up echocardiographic studies were routinely planned and performed on the third, fifth and seventh day of hospitalization. The latest echocardiographic data taken during hospitalization were used in the analysis.
Intraobserver and interobserver variabilities of the TAPSE and TASV were evaluated in 15 random subjects by two investigators and measured by calculating the intraclass correlation coefficients.
The data were analyzed using standard software (SPSS version 19.0, IBM, Chicago, IL, USA) and MedCalc (version 12.3.0, MedCalc Software, Mariakerke, Belgium). Summary data were expressed as mean values ± SD or percentage of patients. Linear regression analysis was performed to evaluate the relationship between TAPSE and TASV, and other variables. Due to skewed distribution, B-type natriuretic peptide (BNP) concentration was assessed using logarithmically transformed values (base 10). The optimal cutoff value for predicting RV systolic dysfunction defined by RVFAC < 35% was determined by the receiver-operating characteristic curve analysis. Comparison of areas under the curve (AUC) was done with the method suggested by Hanley and McNeil.15) Time to first event analysis was performed using a Cox proportional hazards model with the combined endpoint of death, recurrence of PE and PE related hospital admission. To avoid overfitting of the model, we used a bootstrapping in that analysis. A p value less than 0.05 was considered statistically significant.
A total 50 consecutive patients (38 females, mean age 68 ± 14 years old) were included in this study. Their baseline clinical and routine echocardiographic data are listed in Table 1. Common underlying etiologies were operations, malignancies and cerebrovascular accidents. In our study cohort, 9 had surgical treatments within 1 month. Five of them had orthopedic surgery of their lower extremities, 2 had abdominal surgeries, 1 had spinal surgery and 1 had flap surgery of her buttock. Six had malignancy; 2 stomach cancer, 1 pancreatic cancer, 1 renal cell carcinoma, 1 colon cancer and 1 bladder cancer. However, the underlying cause was not identified in about 42% of the patients. RV systolic dysfunction, defined by RVFAC less than 35%, was present in 39 patients (78%) and 17 patients (34%) underwent thrombolytic therapy. Of them, 2 had complications associated with thrombolytic therapy (1 minor bleeding and 1 major bleeding).
McConnell's sign was found in 33 patients (66%). TAPSE and TASV showed significant correlation (r = 0.582, p < 0.001). TAPSE showed significant correlations with RVFAC (r = 0.841, p < 0.001), RV Tei index (r = -0.347, p = 0.018), pulmonary vascular resistance (PVR) (r = -0.635, p < 0.001) and LogBNP (r = -0.634, p < 0.001) (Fig. 1). TASV showed significant correlations with RVFAC (r = 0.605, p < 0.001), RV Tei index (r = -0.380, p = 0.009), PVR (r = -0.483, p = 0.001) and LogBNP (r = -0.477, p = 0.001) (Fig. 2). TAPSE showed significant correlations with serum markers of RV dysfunction such as troponin-I level (r = -0.335, p = 0.019) and creatinine kinase-MB (CK-MB, r = -0.402, p = 0.005). However, TASV did not reveal the correlation with troponin I and CK-MB.
Echocardiographic parameters were improved with treatment during hospitalization (mean duration: 5.1 ± 6.3 days). Follow-up echocardiographic data were available in 44 patients and their data were summarized in Table 2.
There were 39 patients with RV systolic dysfunction determined by RVFAC (< 35%). The best cutoff of TAPSE for detection of RV systolic dysfunction was 1.75 cm (AUC = 0.96, p < 0.001) with a sensitivity of 87% and specificity 91%. The best cutoff for TASV was 13.8 cm/sec (AUC = 0.90, p < 0.001), sensitivity 86% and specificity 78%. However, there was no statistical significance in the detection of RV dysfunction with the comparison of AUC's by Hanley-McNeil method (difference = 0.07, 95% CI = -0.21-0.17, p = 0.130) (Fig. 3).
During the follow-up period of 27 ± 15 months, there were 9 deaths and 1 recurrence of PE. Among the 9 deaths, there were 4 cardiovascular deaths (2 died during hospital admission of PE and 2 died suddenly from discontinuance of medications). There was no statistical difference between normal or depressed RV function determined by TAPSE and TASV by survival analysis (Fig. 4). After Cox proportional hazard regression analysis, TAPSE and TASV were not associated with any cause death and adverse clinical events (Table 3).
Interobserver variability of TAPSE was small [intraclass correlation coefficient was 0.95 (95% CI = 0.89-0.98) p < 0.001], and similar to intraobserver [0.97 (95% CI = 0.93-0.99), p < 0.01]. Interobserver variability of TASV was small [intraclass correlation coefficient was 0.98 (95% CI = 0.96-0.99), p < 0.001], and similar to intraobserver [0.98 (95% CI = 0.97-1.00), p < 0.01].
In this study, we showed good correlations between tricuspid annular motion indices (TAPSE and TASV) and echocardiographic parameters and serum BNP concentrations in patients with acute PE. Although TAPSE and TASV revealed good correlations with conventional echocardiographic RV parameters, they were not associated with adverse clinical events, cardiac death or any cause death in this study.
PE is a relatively common cardiovascular disease and its annual incidence in the United States is about 600000 cases.16) The consequences of acute PE are mainly hemodynamic and become evident when more than a third of pulmonary arterial bed is obstructed.17) Emboli might abruptly increase pulmonary arterial resistance and pressure by obstructing the pulmonary vascular bed. The increased pulmonary arterial resistance can affect the structure and function of RV.16)
Echocardiography remains the most common first-line imaging test in acute PE patients and uses indirect signs of the hemodynamic consequences of RV pressure overload to diagnose acute PE.18) RV dilatation, hypokinesis of RV free wall or signs of RV pressure overload are major echocardiographic markers of RV dysfunction.1) Despite 2DE cannot be used as a diagnostic test in the detection of PE, the absence of echocardiographic signs of RV overload or dysfunction can exclude PE in patients with suspected high-risk PE presenting with shock or hypotension. Echocardiography also can give additional information about the differential diagnosis of the cause of shock. In addition, echocardiographic assessment of RV systolic function can be used to determine treatment modality in these patients. However, assessment of RV systolic function is usually difficult because of the complex shape of the RV.
RV systolic function has been evaluated using several parameters in echocardiographic examination. Of them, RVFAC, TAPSE and TASV are most commonly used indices in 2DE measurements. RVFAC is most commonly used parameter with proven prognostic power in many cardiovascular disease including heart failure and PE.19)20) However, RVFAC can be influenced by image quality and tracing of RV free wall.11) TAPSE and TASV are parameters assessing the motion of tricuspid annulus.9)21) The major advantages of these parameters are that they are easy to perform and have fewer reproducibility errors.11) Unlike strain measurements of the RV, these can be obtained with routine echocardiographic examination and do not require off-line measurement.
In this study, TAPSE and TASV was significantly decreased in the baseline examination and improved with treatment. We also showed significant correlation between TAPSE and TASV and PVR. This can be an expression of reduced systolic longitudinal RV function due to increased RV afterload. The more pronounced decrease in TAPSE or TASV can indicate a more reduced RV systolic function and can be associated with a clinically significant PE. Although TAPSE and TASV are the most commonly used conventional echocardiographic parameters in the detection of RV systolic function,11)12) it can be affected by tethering or translational motion of the heart. Moreover, TAPSE and TASV cannot exclude PE like other echocardiographic parameters.
We did not find the association of decreased tricuspid annular motion and adverse clinical outcomes in this study. This may be because there were a relatively small number of patients in this study and that there was lower incidence of clinical events in PE patients with treatment. In our study, there were 4 cardiovascular deaths (2 died during hospital admission of PE and 2 died suddenly from discontinuance of medications). There were 2 cancer related deaths and 3 deaths associated with preexisting medical conditions. Our data is constituent with the previous study by Carson et al.22) They concluded that clinically apparent PE was an uncommon cause of death and most deaths were due to underlying diseases like cancer, heart failure or chronic lung disease.
This is an observational study with analysis of relatively small numbers of stored digital images. Bias may have been introduced from patient selection. Analysis may have been affected by image quality. Second, we assessed RV systolic function by RVFAC in the differentiation of RV systolic dysfunction. Other more accurate and objective imaging modalities, such as cardiac magnetic resonance imaging or RV angiography, would have increased this study's reliability. Unfortunately, patients with acute PE usually needed intensive therapy and were not suitable for these imaging studies in their presentation. A prospective study with a larger number of patients and using different echocardiographic machines at the same time will be needed to confirm the correlations and the clinical impact of this measurement.
Figures and Tables
Fig. 1
Correlations between tricuspid annular plane systolic excursion (TAPSE) and echocardiographic parameters and serum B-natriuretic peptide (BNP) level. TAPSE shows good correlations with RV fractional area change (RVFAC, A), RV Tei index (B), pulmonary vascular resistance (PVR, C) and LogBNP (D).

Fig. 2
Correlations between tricuspid annular systolic velocity (TASV) and echocardiographic parameters and serum B-natriuretic peptide (BNP) level. TASV shows good correlations with RV fractional area change (RVFAC, A), RV Tei index (B), pulmonary vascular resistance (PVR, C) and LogBNP (D).

Fig. 3
Receiver operating curve analysis in the detection of right ventricular (RV) systolic dysfunction (determined by RV fractional area change < 35%). Tricuspid annular plane systolic excursion (TAPSE) shows larger area under the curve than tricuspid annular systolic velocity (TASV). However, there is no statistical significance (difference = 0.07, 95% CI: -0.02-0.17, p = 0.130) in the detection of RV systolic dysfunction. AUC: areas under the curve, CI: confidential interval.
Fig. 4
Survival curves by Kaplan-Meier analysis. There was no statistical significance in the groups of right ventricular systolic dysfunction by tricuspid annular plane systolic excursion (TAPSE, A) or tricuspid annular systolic velocity (TASV, B). p value was calculated by log-rank test.

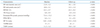
Table 1
Baseline characteristics (n = 50)

CVA: cerebrovascular accident, TIA: transient ischemic attack, BNP: B-type natriuretic peptide, CK-MB: creatinine kinase-MB, LV: left ventricle, RV: right ventricle, RVFAC: right ventricular fractional area change, TR: tricuspid regurgitation, PA: pulmonary artery, PVR: pulmonary vascular resistance, TAPSE: tricuspid annular plane systolic excursion, TASV: tricuspid annular systolic velocity
References
1. Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galiè N, Pruszczyk P, Bengel F, Brady AJ, Ferreira D, Janssens U, Klepetko W, Mayer E, Remy-Jardin M, Bassand JP. ESC Committee for Practice Guidelines (CPG). Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur Heart J. 2008. 29:2276–2315.
2. Kucher N, Rossi E, De Rosa M, Goldhaber SZ. Prognostic role of echocardiography among patients with acute pulmonary embolism and a systolic arterial pressure of 90 mm Hg or higher. Arch Intern Med. 2005. 165:1777–1781.

3. Grifoni S, Olivotto I, Cecchini P, Pieralli F, Camaiti A, Santoro G, Conti A, Agnelli G, Berni G. Short-term clinical outcome of patients with acute pulmonary embolism, normal blood pressure, and echocardiographic right ventricular dysfunction. Circulation. 2000. 101:2817–2822.

4. Dell'Italia LJ. The right ventricle: anatomy, physiology, and clinical importance. Curr Probl Cardiol. 1991. 16:653–720.
5. Tandri H, Daya SK, Nasir K, Bomma C, Lima JA, Calkins H, Bluemke DA. Normal reference values for the adult right ventricle by magnetic resonance imaging. Am J Cardiol. 2006. 98:1660–1664.

6. Cresci SG, Goldstein JA. Hemodynamic manifestations of ischemic right heart dysfunction. Cathet Cardiovasc Diagn. 1992. 27:28–33. discussion 33-4.

7. Kaul S, Tei C, Hopkins JM, Shah PM. Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J. 1984. 107:526–531.

8. Ueti OM, Camargo EE, Ueti Ade A, de Lima-Filho EC, Nogueira EA. Assessment of right ventricular function with Doppler echocardiographic indices derived from tricuspid annular motion: comparison with radionuclide angiography. Heart. 2002. 88:244–248.

9. Meluzín J, Spinarová L, Bakala J, Toman J, Krejcí J, Hude P, Kára T, Soucek M. Pulsed Doppler tissue imaging of the velocity of tricuspid annular systolic motion; a new, rapid, and non-invasive method of evaluating right ventricular systolic function. Eur Heart J. 2001. 22:340–348.

10. Saxena N, Rajagopalan N, Edelman K, López-Candales A. Tricuspid annular systolic velocity: a useful measurement in determining right ventricular systolic function regardless of pulmonary artery pressures. Echocardiography. 2006. 23:750–755.

11. Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010. 23:685–713. quiz 786-8.

12. Grapsa J, Dawson D, Nihoyannopoulos P. Assessment of right ventricular structure and function in pulmonary hypertension. J Cardiovasc Ultrasound. 2011. 19:115–125.

13. Abbas AE, Fortuin FD, Schiller NB, Appleton CP, Moreno CA, Lester SJ. A simple method for noninvasive estimation of pulmonary vascular resistance. J Am Coll Cardiol. 2003. 41:1021–1027.

14. McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996. 78:469–473.

15. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982. 143:29–36.

16. Wood KE. Major pulmonary embolism: review of a pathophysiologic approach to the golden hour of hemodynamically significant pulmonary embolism. Chest. 2002. 121:877–905.
17. McIntyre KM, Sasahara AA. The hemodynamic response to pulmonary embolism in patients without prior cardiopulmonary disease. Am J Cardiol. 1971. 28:288–294.

18. Leibowitz D. Role of echocardiography in the diagnosis and treatment of acute pulmonary thromboembolism. J Am Soc Echocardiogr. 2001. 14:921–926.

19. Di Salvo TG, Mathier M, Semigran MJ, Dec GW. Preserved right ventricular ejection fraction predicts exercise capacity and survival in advanced heart failure. J Am Coll Cardiol. 1995. 25:1143–1153.

20. Nass N, McConnell MV, Goldhaber SZ, Chyu S, Solomon SD. Recovery of regional right ventricular function after thrombolysis for pulmonary embolism. Am J Cardiol. 1999. 83:804–806. A10





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download