Abstract
Percutaneous coronary intervention for chronic total occlusion of coronary arteries remains technically challenging. It shows lower procedural success rates compared with other lesion subsets. It is for this reason that interventional cardiologists have developed many techniques to recanalize chronically occluded arteries. Among them, we experienced some cases in which we used the subintimal tracking and re-entry (STAR) technique. Here we report our experience with a review of the literature.
Chronic total occlusion (CTO) occurs in approximately one third of all patients with significant coronary artery disease who have undergone coronary angiography.1 Percutaneous coronary intervention (PCI) for CTO remains one of the most technically challenging scenarios in interventional cardiology.2,3 Interventional cardiologists have developed various methods to overcome the difficulties in recanalization of chronically totally occluded coronary arteries. The subintimal tracking and re-entry (STAR) technique is a result of such struggles.
An approach by the STAR technique for recanalization of CTO may succeed where other methods fail.4 The procedure, which involves the creation of a subintimal dissection followed by distal reentry, is a promising approach to the treatment of CTO, particularly in the right coronary artery. Here, we describe four cases of recanalization of CTO by use of the STAR technique in patients who had failed previous CTO-recanalization attempts.
A 63-year-old man visited our hospital owing to effort angina. He was a current smoker and had been treated with anti-hypertensive medication. Also, he had undergone percutaneous transluminal angioplasty (PTA) for occlusive disease of both common iliac arteries 6 months ago. At the time of PTA, total occlusion of the right coronary artery was found and PCI was attempted, but recanalization failed (Fig. 1). Although it had developed 3 years ago, his chest pain was bearable until the first attempt of PCI for total occlusion of the right coronary artery performed 6 months ago. However, his chest pain became aggravated as his exercise capacity increased after treatment of both common iliac artery occlusions.
An electrocardiogram showed a normal sinus rhythm and an echocardiogram revealed normal systolic function. We tried to do PCI for total occlusion of the right coronary artery, because the intensity and frequency of his chest pain were gradually increasing. A coronary angiogram showed total occlusion of the midportion of the right coronary artery and significant stenosis of the proximal portion of the right coronary artery (Fig. 2A). First, we tried to cross the wire via the septal branch of the left anterior descending coronary artery by using a retrograde approach, but we could not advance the guidewire into the distal true lumen (Fig. 2B). As a second step, we tried to pass the guidewire through the total occlusion of the right coronary artery by using an antegrade approach, but we also failed to find the distal true lumen (Fig. 2C). Finally, we attempted the STAR technique. After advancing a microcatheter into the occlusion, we removed the guidewire and injected about 1 mL of contrast into the occlusion. Contrast injection made subintimal dissection and visualization of the true vessel lumen possible (Fig. 2D). We then successfully advanced the Fielder FC guidewire (Asahi Intec, Aichi, Japan), floppy guidewire, into the distal true lumen (Fig. 2E). After successful deployment of four Cypher stents (Cordis Corp, Miami Lakes, Florida, USA), the final angiogram showed good distal flow (Fig. 2F).
The patient is currently being treated as an outpatient without chest pain, dyspnea, or claudication. We plan to conduct a follow-up angiogram 6 months after the revascularization of the right coronary artery.
We have accumulated more experience with revascularization of CTO by use of the STAR technique. Case 2 (Fig. 3) was a 76-year-old man who had hypertension and arteriosclerosis obliterans. The patient was admitted to our hospital for treatment of his exertional dyspnea. PCI for CTO had been attempted 1 year previously in another hospital, but the result was unsuccessful. On the coronary angiogram, we could see the CTO of the midportion of the right coronary artery at the takeoff of the side branch. We successfully carried out recanalization with three Taxus stents (Boston Scientific Corp., Natick, Massachusetts) by use of the STAR technique.
Case 3 (Fig. 4) was an 80-year-old man who presented with dyspnea on exertion. He was on medication for hypertension, diabetes, and angina. He had also failed a prior CTO-recanalization attempt. His coronary angiogram revealed total occlusion of the midportion of the left anterior descending coronary artery at the takeoff of the side branch as in Case 2. He also underwent PCI with three Taxus stents (Boston Scientific Corp., Natick, Massachusetts) by use of the STAR technique.
Case 4 (Fig. 5) was a case of failed recanalization of CTO by use of the STAR technique. A 64-year-old man similar to Case 4, who had diabetes and hypertension, underwent coronary intervention for CTO of the distal left circumflex coronary artery by the STAR technique. However, recanalization failed, leaving storm cloud dissection. Fortunately, other events such as pericardial effusion, coronary artery perforation, or myocardial hematoma did not occur.
The STAR technique, which was first described by Colombo,4 has not been widely used. Its main concept is subintimal angioplasty used in peripheral artery occlusive disease (PAOD). In treating PAOD by use of subintimal angioplasty, a 0.035-inch guidewire with a J-configuration is used for subintimal dissection with distal reentry. In the same manner, a 0.014-inch guidewire was used for subintimal dissection with distal reentry in the first described report by Colombo.4 Carlino later developed the modified STAR technique with the use of a contrast guidance later.5 He used contrast injection via a microcatheter or over-the-wire balloon instead of the J-configured guidewire to create the subintimal dissection. According to his paper, the angiographic success rate was 82.3%, stent thrombosis did not occur, and restenosis with the STAR technique was high. He concluded that the contrast-guided STAR technique appears to be a feasible and relatively safe strategy and can be regarded as a refined evolution to the original approach.
However, the STAR technique is a risky procedure and has some shortcomings. There is a too high rate of compromising the side branch, because the procedure is conducted by subintimal dissection. Also, known complications of the technique are myocardial hematoma, dissection limiting procedure, coronary perforation, and stent thrombosis.5,6 Furthermore, the rate of in-stent restenosis is higher than with other conventional procedures, even when a drug-eluting stent is implanted. Colombo reported that the rate of in-stent restenosis was 53% (use of drug-eluting stents: 53%) and Carlino reported that the rate of in-stent restenosis was 44.7% (use of drug-eluting stents: 92.7%).4,5 According to these two reports, the marked increase in utilization of drug-eluting stents did not overcome the in-stent restenosis. Unfortunately, the mechanism of the higher tendency for in-stent restenosis has not been elucidated. In light of Schwartz's report,7 one reason that the STAR technique has a higher incidence of in-stent restenosis may be that recanalization by the STAR technique results in more injured vessel walls compared with other conventional techniques. Although we did not experience terrible complications, some troubles such as storm cloud dissection precluded recanalization (Case 4), and major side branch dissection (Case 3) occurred. We inserted drug-eluting stents in all of our cases. As of yet, we have not checked the follow-up coronary angiograms, because the patients have not had myocardial ischemic symptoms and the 6-month time period has not yet passed. Nevertheless, there is a high possibility of in-stent restenosis.
In terms of risk of the procedure and complications, the technique should not be a first-line approach to the treatment of what remain the most challenging lesions in interventional cardiology. It should really be advised as a final resort when other means fail and when a surgical procedure is not possible. Actually, all of our cases had a history of unsuccessful recanalization. The reasons for previous failure in our cases were total occlusion at the takeoff of the side branch (Cases 2, 3, and 4) and too hardly long occlusion (Case 1). We performed successful PCI by use of the STAR technique for two right coronary arteries (Case 1 and 2) and one left anterior descending coronary artery (Case 3), but the PCI failed for one left circumflex coronary artery (Case 4). Although there are too few cases to judge, this is consistent with previous reports that the rate of STAR technique utilization is high in the right coronary artery (79.4~87%).4,5 However, why the right coronary artery is favored for the STAR technique is unclear. There is a chance of selection bias. Actually, 79.4% of the lesions treated by Carlino were in the right coronary artery (left anterior descending coronary artery: 1.5%, left circumflex artery: 19.1%).5 One possibility is that the right coronary artery has a lesser tendency for tortuosity.
To our knowledge, our report concerning recanalization of CTO by use of the STAR technique is the first such report in Korea. In conclusion, recanalization by the STAR technique with the use of drug-eluting stenting may be the best option in selected CTO after failure or infeasibility of the standard antegrade or retrograde technique, especially in the right coronary artery.
Figures and Tables
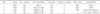
 | Fig. 1First attempt at percutaneous coronary intervention for chronic total occlusion of the midportion of the right coronary artery in Case 1. (A) Right coronary angiogram showed significant stenosis of the proximal portion of the right coronary artery and chronic total occlusion of the midportion of the right coronary artery. (B) Attempt to cross the guidewire through the chronic total occlusion failed. |
 | Fig. 2Second attempt at percutaneous coronary intervention 6 months after the first attempt in Case 1. (A) Angiogram showed total occlusion of the midportion of the right coronary artery (star). (B) Retrograde intervention via the septal branch under contralateral contrast injection failed. (C) Guidewire passage via the antegrade approach failed. Note that the guidewire tip was outside the distal true lumen. (D) Subintimal tracking by contrast injection via microcatheter made the path to the distal true lumen (arrow). (E) Percutaneous transluminal coronary angioplasty was performed by using the anchor balloon technique after successful wiring into the distal true lumen. (F) Final angiogram after deployment of four sirolimus-eluting stents showed a good result without residual stenosis. |
 | Fig. 3Right coronary angiogram and percutaneous coronary intervention in Case 2. (A) Coronary angiogram showed total occlusion of the midportion of the right coronary artery at the takeoff of the side branch (star). (B) After subintimal tracking by contrast injection via microcatheter, the distal true lumen was visible (arrow). (C) Percutaneous transluminal balloon angioplasty was performed. (D) We obtained good results after deployment of three paclitaxel-eluting stents. |
 | Fig. 4Left coronary angiogram and percutaneous coronary intervention in Case 3. (A) Coronary angiogram showed total occlusion of the midportion of the left anterior descending coronary artery at the side branch (star). (B) After subintimal tracking by contrast injection via microcatheter, we could see the distal true lumen (arrow) with large dissection of the midportion of the left anterior descending coronary artery and diagonal branch. (C) The angiogram showed a good entrance of the guidewire into the distal true lumen. (D) Final angiogram revealed good distal flow without any complications after deployment of two paclitaxel-eluting stents for the left anterior descending coronary artery and one paclitaxel-eluting stent for the diagonal branch by kissing balloon angioplasty. |
 | Fig. 5Left coronary angiogram and percutaneous coronary intervention in Case 4. (A) Coronary angiogram revealed total occlusion of the distal portion of the left circumflex coronary artery at the side branch (star). (B) After contrast injection by use of a microcatheter, large dissection occurred. (C) Despite a visible distal true lumen (arrow), crossing the guidewire failed. |
References
1. Christofferson RD, Lehmann KG, Martin GV, Every N, Caldwell JH, Kapadia SR. Effect of chronic total coronary occlusion on treatment strategy. Am J Cardiol. 2005. 95:1088–1091.

2. Stone GW, Kandzari DE, Mehran R, Colombo A, Schwartz RS, Bailey S, et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part I. Circulation. 2005. 112:2364–2372.

3. Stone GW, Reifart NJ, Moussa I, Hoye A, Cox DA, Colombo A, et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part II. Circulation. 2005. 112:2530–2537.

4. Colombo A, Mikhail GW, Michev I, Iakovou I, Airoldi F, Chieffo A, et al. Treating chronic total occlusions using subintimal tracking and reentry: the STAR technique. Catheter Cardiovasc Interv. 2005. 64:407–411.

5. Carlino M, Godino C, Latib A, Moses JW, Colombo A. Subintimal tracking and re-entry technique with contrast guidance: a safer approach. Catheter Cardiovasc Interv. 2008. 72:790–796.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download