Abstract
Renal cell carcinomas can metastasize to almost any organ. Metachronous solitary contralateral adrenal metastasis from renal cell carcinoma is, however, very rare. Surgical resection is appropriate in isolated metastatic renal cell carcinoma, but the metastasectomy in the case of contralateral adrenal metastasis of renal cell carcinoma has not been well defined. Herein, we report a case of renal cell carcinoma with solitary metachronous contralateral adrenal metastasis occurring 4 years after curative laparoscopic radical nephrectomy. The patient was treated with retroperitoneal laparoscopic adrenalectomy.
Renal cell carcinomas (RCCs) can metastasize to almost any organ. The most common involved sites, in order of frequency, are the lung, lymph nodes, liver, contralateral kidney, and bone. RCC involvement of the ipsilateral adrenal gland is noted in 1.2~10% of radical nephrectomy specimens,1 but the sole involvement of the contralateral adrenal gland as the site of metachronous metastasis is rare.2 Here we present an exceptional case of metachronous solitary adrenal metastasis that was treated by retroperitoneal laparoscopic adrenalectomy.
A 40-year-old man presented to our hospital with an incidentally detected right renal mass. Abdominal and pelvic computed tomography (CT) showed a 5×4.7 cm sized mass with mixed attenuation arising from the superior aspect of the right kidney. No other intraabdominal or adjacent organ involvements were found on CT. The patient underwent retroperitoneal laparoscopic radical nephrectomy and ipsilateral adrenalectomy. The pathology report showed RCC (clear cell type) with a Fuhrman nuclear grade of 2. The tumor had not extended into the perinephric fat, adrenal gland, or left renal vein (stage T1bN0M0). Thus, the patient was followed with annual chest X-rays and abdominal CT. Four years after a right nephrectomy, follow-up abdominal CT revealed a 1.3 cm sized enhanced mass in the left adrenal gland (Fig. 1). In addition, positron emission tomography revealed a fluorodeoxyglucose (FDG)-avid, enlarged left adrenal gland with no other abnormality. Endocrinological evaluation demonstrated normal urinary 17-ketosteroids, 17-hydrocorticoids, metanephrines, cortisol, and vanillylmandelic acid.
The patient underwent retroperitoneal laparoscopic left adrenalectomy. The operative time was 2 hours 3 minutes and estimated intraoperative blood loss was 70 ml. Postoperatively, immediate steroid replacement therapy with prednisolone 2.5 mg and fludrocortisones 0.1 mg was given in the morning for adrenal insufficiency. The histological features of the specimen were consistent with the primary RCC, which had not invade d the adjacent structure (Fig. 2).
The postoperative period was uneventful, and the patient was discharged on postoperative day 3. After 1 month, the patient is being treated with interferon monotherapy.
Approximately 25% of patients with RCC will already have multiple distant metastases at the time of presentation, including the lungs, lymph nodes, liver, bones, contralateral kidney, and less frequently, the adrenal glands.3 The prevalence of RCC involvement of the ipsilateral adrenal gland is 19% in autopsy series and 5.5% in surgical series, whereas the contralateral adrenal is involved in up to 11% of autopsy series and 3.4% of surgical series with a variability of latency in diagnosis.4,5
Although primary RCC metastasis to the adrenal glands is generally hematogenous because of the rich blood supply of the adrenal gland and its high ratio of blood volume to unit weight,6 and the risk of ipsilateral adrenal metastasis is associated with advanced stage tumors of the upper pole, the predisposing factor for contralateral adrenal metastasis by RCC is still unknown.4 Of particular interest, Stein et al.7 reported that metastatic spread to the contralateral adrenal gland showed an 80% incidence of involvement of the renal vein or inferior vena cava by primary RCC. In our case, preoperative imaging of the RCC before retroperitoneal laparoscopic radical nephrectomy revealed stage I disease.
The most favorable diagnostic approach to a solitary contralateral adrenal tumor in patients with a history of RCC is contentious.4 Radiological studies may facilitate the preoperative diagnosis but cannot determine with certainty whether an adrenal tumor in a patient with RCC is a primary adrenal neoplasm, an adrenal cortical adenoma, or a metastasis.4 The preoperative diagnosis of contralateral adrenal metastasis begins with high suspicion based on a history of RCC. In these patients, the findings of a solitary adrenal tumor without elevated serum adrenal hormones is strongly suggestive of a metastatic lesion to the adrenal gland,7 as in our patient.
Oncologically, surgical removal of a solitary adrenal metastasis remains the only treatment option for these patients. Only surgical treatment can achieve satisfactory survival rates. However, it is difficult to estimate overall survival because of the small number of such cases. Some authors have reported that adrenal metastasectomy can achieve a good rate of freedom from disease after surgery and acceptable survival rates when compared with diffuse metastatic disease.2 Kessler et al8 reported that the longer the interval between nephrectomy and the appearance of the adrenal metastasis, the better the prognosis. Probably this latency in the appearance of metastasis represents a less aggressive behavior of cancerous cells, with slower progression that connotes a better prognosis. These results could justify the indication for surgical resection of adrenal metastasis from RCC with subsequent adjuvant therapy with biological response modifiers.
Recently, laparoscopic adrenalectomy has been performed successfully transperitoneally and retroperitoneally to treat a variety of adrenal pathological conditions. Compared with the transperitoneal approach,9 the retroperitoneal approach is technically simple, can be performed quickly, and has low postoperative morbidity and should be regarded as the routine approach for relatively small adrenal tumors that are less than 5 cm in diameter.10 It also avoids invading the intraperitoneal cavity and possible injury to the abdominal organs. In our case, a patient with a previous history of retroperitoneal laparoscopic radical nephrectomy of the contralateral kidney, the adrenal metastasis measured 1.3 cm in CT and was resected successfully through a laparoscopic retroperitoneal approach.
In conclusion, solitary metachronous contralateral adrenal metastases from RCC are rare clinically, but patients may benefit from the surgical resection of contralateral adrenal metastasis from renal carcinoma. In this case, retroperitoneal laparoscopic adrenalectomy is feasible.
Figures and Tables
Fig. 1
Enhanced computed tomography showing a 1.3 cm left adrenal mass, 4 years after a right radical nephrectomy.
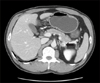
Fig. 2
The histologic features of the specimen: (A) Gross finding of the round tumor (center) in the yellow adrenal gland (right) is noted. (B) The metastatic nodule (closed triangle) is noted near the adrenal gland (closed circle) (×10). (C) The capsule seperating the metastatic tumor (closed triangle) and the adrenal gland (closed circle) is noted (×40). (D) The metastatic tumor growing in a trabecular pattern with clear cytoplasm is noted (×100).

References
1. Kuczyk M, Wegener G, Jonas U. The therapeutic value of adrenalectomy in case of solitary metastatic spread originating from primary renal cell cancer. Eur Urol. 2005. 48:252–257.

2. Antonelli A, Cozzoli A, Simeone C, Zani D, Zanotelli T, Portesi E, et al. Surgical treatment of adrenal metastasis from renal cell carcinoma: a single-centre experience of 45 patients. BJU Int. 2006. 97:505–508.

3. Fuselier HA Jr, Guice SL 3rd, Brannan W, Ochsner MG, Sangisetty KV, Beckman EN, et al. Renal cell carcinoma: the Ochsner Medical Institution experience (1945-1978). J Urol. 1983. 130:445–448.

4. Lau WK, Zincke H, Lohse CM, Cheville JC, Weaver AL, Blute ML. Contralateral adrenal metastasis of renal cell carcinoma: treatment, outcome and a review. BJU Int. 2003. 91:775–779.

5. Stephenson AJ, Chetner MP, Rourke K, Gleave ME, Signaevsky M, Palmer B, et al. Guidelines for the surveillance of localized renal cell carcinoma based on the patterns of relapse after nephrectomy. J Urol. 2004. 172:58–62.

6. Sagalowsky AI, Kadesky KT, Ewalt DM, Kennedy TJ. Factors influencing adrenal metastasis in renal cell carcinoma. J Urol. 1994. 151:1181–1184.

7. Stein A, Mecz Y, Sova Y, Lurie M, Lurie A. Synchronous and metachronous contralateral adrenal metastases from primary renal cell carcinoma. Urol Int. 1997. 58:58–60.

8. Kessler OJ, Mukamel E, Weinstein R, Gayer E, Konichezky M, Servadio C. Metachronous renal cell carcinoma metastasis to the contralateral adrenal gland. Urology. 1998. 51:539–543.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download