Abstract
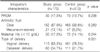
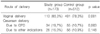
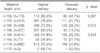
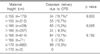
This study was performed to identify the relationship between maternal height of ≤155 cm and the risk of cesarean delivery and cesarean delivery due to cephalopelvic disproportion (CPD) among women who had delivered in Chonnam National University Hospital from January 1997 to December 2007. A total of 1214 term, uncomplicated, singleton nulliparous pregnant women were selected among 10,434 deliveries, and the patients were divided into two groups based on maternal height: ≤155 cm (173 cases) as the study group and >155 cm (512 cases) as the control group. Various baseline clinical characteristics, intrapartum characteristics, and maternal and neonatal outcomes were analyzed. The cesarean delivery rate was 34.7% (60/173) in the study group and 21.7% (111/512) in the control group, which was statistically significant (p=0.001). The cesarean delivery rate due to CPD was 19.7% (34/173) in the study group and 10.7% (55/512) in the control group, which was statistically significant (p=0.003). Birth weight was significantly lower in the study group than in the control group (3193.2±336.8 g and 3293.0±384.1 g respectively, p<0.003). In conclusion, the overall cesarean delivery rate and cesarean delivery rate due to CPD were higher and the birth weight was lower in the term nulliparous women with short stature.
References
1. ACOG. Practice Bulletin No 49. Dystocia and augmentation of labor. 2003. 12.
2. Korean Health Insurance Review & Assessment Service. Appropriateness assessment of cesarean delivery in year 2003.
3. Park YY. Major and minor indications of cesarean delivery (1965-1995). Korean J Obstet Gynecol. 1999. 42:254–259.
4. Abou-Zahr Carla Lidia, Royston Erica. Maternal mortality, a global factbook. 1991. Geneva: World Health Organization;598.
5. Van Roosmalen J, Brand R. Maternal height and the outcome of labor in rural Tanzania. Int J Gynecol Obstet. 1992. 37:169–177.

6. Harlow BL, Frigoletto FD, Cramer DW, Evans JK, Bain RP, Ewigman B, et al. Epidemiologic predictors of cesarean section in nulliparous patients at low risk. Am J Obstet Gynecol. 1995. 172:156–162.

7. Maternal anthropometry and pregnancy outcomes. A WHO collaborative study. Bull World Health Organ. 1995. 73:Suppl. 1–98.
8. Ogala WN, Audu L. Predicting conception and safe delivery of a macrosomic baby. Cent Afr J Med. 1996. 42:316–319.
9. Turcot L, Marcoux S, Fraser WD. Multivariate analysis of risk factors for operative delivery in nulliparous women. Canadain Early Amniotomy Study Group. Am J Obstet Gynecol. 1997. 176:395–402.

10. Stewart KS, Cowan DB, Philpott RH. Pelvic dimensions and the outcome of trial of labour in Shona and Zulu primigravidas. S Afr Med J. 1979. 55:847–851.
11. Frame S, Moore J, Peters A, Hall D. Maternal height and shoe size as predictors of pelvic disproportion: an assessment. Br J Obstet Gynaecol. 1985. 92:1239–1245.

12. Camilleri AP. The obstetric significance of short stature. Eur J Obstet Gynecol Reprod Biol. 1981. 12:347–356.

13. Kappel B, Eriksen G, Hansen KB, Hvidman L, Krag-Olsen B, Nielsen J, et al. Short stature in Scandinavian women. An obstetrical risk factor. Acta Obstet Gynecol Scand. 1987. 66:153–158.

14. Brabin L, Verhoeff F, Brabin BJ. Maternal height, birhtweight and cephalopelvic disproportion in urban Nigeria and rural Malawi. Acta Obstet Gynecol Scand. 2002. 81:502–507.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download