Abstract
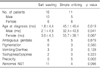
This study was performed to investigate the clinical features of congenital adrenal hyperplasia (CAH) with steroid 21-hydroxylase deficiency and to compare the salt-wasting (SW) type with the simple virilizing (SV) type. Twenty-seven patients (15 boys, 12 girls) who received a diagnosis of CAH at Chonnam University Hospital from May 1998 to May 2008 were enrolled in the present study. The patients' medical records were analyzed retrospectively. Age and clinical symptoms at diagnosis, ratio of bone age to chronologic age, body mass index (BMI), and treatment dose of hydrocortisone were reviewed. Of the 27 patients, 16 patients had SW type and 11 patients had SV type. The SV patients were significantly older (p<0.05) at the time of diagnosis (45.1±40.4 months) than were the SW patients (1.8±4.4 months). In the SW patients, the initial ratio of bone age to chronologic age was 1.10±0.15 in the boys and 1.52±0.74 in the girls, and the final BMI was 16.6±2.81 kg/m2 in the boys and 17.4±4.21 kg/m2 in the girls. In the SV patients, the initial ratio of bone age to chronologic age was 1.26±0.38 in the boys and 1.45±0.31 in the girls, and the final BMI was 17.5±2.62 kg/m2 in the boys and 19.6±1.80 kg/m2 in the girls. The treatment dose of hydrocortisone was 18.4±6.54 mg/m2/day in the SW patients and 16.1±5.50 mg/m2/day in the SV patients. The ratio of bone age to chronological age, BMI, and dose of hydrocortisone were not significantly different between the SV and SW patients.
Figures and Tables
References
2. Pang S, Wallace MA, Hofman L, Thuline HC, Dorche C, Lyon IC, et al. Worldwide experience in newborn screening for classical congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Pediatrics. 1998. 81:866–874.

3. Lee HJ, Moon HR. Seventeen years experience on inborn errors of metabolism; a study for future development of inborn errors of metabolism in Korea. J Korean Pediatr Soc. 1990. 33:1031–1036.
4. Lee H. CYP21 mutations and congenital adrenal hyperplasia. Clin Genet. 2001. 59:293–301.
5. Kim HS. Congenital adrenal hyperplasia in Korea. J Korean Soc Pediatr Endocrinol. 2005. 10:132–137.
6. Bickel H. Bickel H, Guthrie R, Hammerson G, editors. Rationale of neonatal screening for inborn errors of metabolism. Neonatal screening for inborn errors of metabolism. 1980. Springer Verlag;1–6.

7. Lee DH. Newborn screening of inherited metabolic disease in Korea. Korean J Pediatr. 2006. 49:1125–1139.

8. Votava F, Török D, Kovács J, Möslinger D, Baumgartner-Parzer SM, Sólyom J, et al. Estimation of the false-negative rate in newborn screening for congenital adrenal hyperplasia. Eur J Endocrinol. 2005. 152:869–874.

9. New MI, Gertner JM, Speiser PW, Del Balzo P. Growth and final height in classical and nonclassical 21-hydroxylase deficiency. J Endocrinol Invest. 1989. 12:Suppl 3. 91–95.
11. Kaplan SA. Diseases of the adrenal cortex. II. Congenital adrenal hyperplasia. Pediatr Clin North Am. 1979. 26:77–89.

12. Soliman AT, AlLamki M, AlSalmi I, Asfour M. Congenital adrenal hyperplasia complicated by central precocious puberty: linear growth during infancy and treatment with gonadotropin-releasing hormone analog. Metabolism. 1997. 46:513–517.

13. Yi KH. Effect on final height of gonadotropin-releasing hormone agonist (GnRHa) in children with congenital adrenal hyperplasia. J Korean Soc Pediatr Endocrinol. 2005. 10:50–56.
14. Cornean RE, Hindmarsh PC, Brook CG. Obesity in 21-hydroxylase deficient patients. Arch Dis Child. 1998. 78:261–263.

15. White PC, New MI, Dupont B. Structure of human steroid 21-hydroxylase genes. Proc Natl Acad Sci USA. 1986. 83:5111–5115.

16. Higashi Y, Yoshioka H, Yamane M, Gotoh O, Fujii-Kuriyama Y. Complete nucleotide sequence of two steroid 21-hydroxylase genes tandemly arrranged in human chromosome: a pseudogene and a genuine gene. Proc Natl Acad Sci USA. 1986. 83:2841–2845.

17. Rodrigues NR, Dunham I, Yu CY, Carroll MC, Porter RR, Campbell RD. Molecular characterization of the HLA linked steroid 21-hydroxylase B gene from an individual with congenital adrenal hyperplasia. EMBO J. 1987. 6:1653–1661.

18. Wedell A. Molecular genetics of congenital adrenal hyperplasia (21-hydroxylase deficiency): implications for diagnosis, prognosis and treatment. Acta Pediatr. 1998. 87:159–164.

19. Ko JM, Chio JH, Kim GH, Yoo HW. Genotype of steroid 21-hydroxylase gene and clinical characteristics in patients with congenital adrenal hyperplasia 21-Hydroxylase deficiency. J Korean Soc Pediatr Endocrinol. 2005. 10:57–63.
20. Jin DK, Kim JS, Song SM, Park SJ, Hwang HZ, On HY, et al. A study on the relationship between genotype and phenotype in Korean patients with congenital adrenogenital syndrome caused by 21-hydroxylase deficiency. J Korean Soc Endocrinol. 2000. 15:237–247.
21. Wilkins L, Lewis RA, Klein R, Rosemberg E. The suppression of androgen secretion by cortisone in a case of congenital adrenal hyperplasia. Bull Johns Hopkins Hosp. 1950. 86:249–252.
22. Bartter FC, Forbes AP, Leaf A. Congenital adrenal hyperplasia associated with the adrenogenital syndrome: an attempt to correct its disordered hormonal pattern. J Clin Invest. 1950. 29:797.
23. Joint LWPES/ESPE CAH Working Group. ESPE CAH Working Group. Consensus statement on 21-hydroxylase deficiency from the Lawson Wilkins Pediatric Endocrine Society and the European Society for Paediatric Endocrinology. J Clin Endocrinol Metab. 2002. 87:4048–4053.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download