Introduction
Punctate type of palmoplantar keratoderma is classified
into three groups,1 including punctate palmoplantar
keratoderma (PPPK), filiform keratoderma, and marginal
papular keratoderma (MPK). MPKs are a complex group
of disorders that share keratotic papules, usually crateriform,
along the borders of the hands and feet as a
common clinical feature. MPK includes acrokeratoelastoidosis
(AKE) and focal acral hyperkeratosis (FAH),
which share similar clinical features and histologically
identical epidermal alterations. These disorders are distinguished
solely by the absence of elastorrhexis in FAH.
Here, we present a familial case of FAH associated with
hyperthyroidism.
Case Report
A 57-year-old Japanese woman was referred to our
department for evaluation of small asymptomatic firm
horny umbilicated papules on the hands and feet. The
lesions were first developed at the age of 30 years and
gradually increased. These lesions were found on the
dorsal surfaces and at the junction between palmar and
dorsal skin, especially surfaces of the fingers, metacarpophalangeal
and interphalangeal joints (Fig. 1). There
were no nail deformities. Two months before her visit,
she commenced thiamazole because she was diagnosed
as hyperthyroidism with TSH: 0.005 µU/ml (normal:
0.5~5.0 µU/ml), free T4 4.94 ng/dl (normal: 0.88~1.62
ng/dl), free T3 18.17 pg/ml (normal: 2.33~4.00 pg/ml).
After the treatment, therapy-related hypothyroidism
(TSH: 15.1, free T4 0.378, free T3: 2.09) was developed
which were accompanied by rapidly increasing
skin lesions on her hands. Her past history was not
tracable. Her oldest sister and her daughter exhibited similar skin lesions. Routine laboratory tests were normal
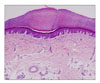
except abnormal thyroid hormones. Histopathological
examination of skin biopsies from the papules revealed
orthohyperkeratosis within focal cup-like depression
of the epidermis (Fig. 2). Elastica van Gieson,
Weigert, and alcian blue stains showed uniform elastic
fibers with no evidence of elastorrhexis. Based on these
findings, we diagnosed these papules as FAH. Topical
treatment with maxacalcitol showed no response.
Discussion
AKE and FAH are genodermatoses that share similar
clinical features and histologically identical epidermal
alteration. FAH is distinguished from AKE on the sole
histological basis of lack of elastorrhexis.2-5 Both disorders
are usually sporadic, although familial cases are autosomal
dominant inheritance that have been described
like our case and a possible linkage to chromosome 2
has been suggested.4 Both form have their onset in
childhood or early adult life and frequently develop until
the age of 20 years.2,3 The lesions are symmetrical
and asymptomatic, although unilateral and painful variants
have been documented.3 Lesions gradually increase
in number and size over the years like our case.2,3
The patient in our study reported that the number of
lesions at the age of 30 years were like that of her
30-year-old daughter.
The causes of AKE and FAH are unknown.2-6 No
human papilloma virus (HPV) DNA has been detected
in affected lesions. There is no evidence that trauma,
arsenic ingestion, or light exposure are factors in the development
of these disorders.3 To our knowledge, there
were no reports on an association between FAH and
hyperthyroidism. However, rapid extension of AKE lesions
during pregnancy has been reported.3,6 In one report,
AKE lesions first appeared at the age of 6 years
showed rapid extension during her pregnancy at the age
of 20 years old. Abnormal thyroid function during pregnancy
is well known. In the first trimester of pregnancy,
human chorionic gonadotropin (hCG) is rapidly increased
at the peak between 7 and 13 weeks of gestation.
hCG has mild TSH-like activity, leading to slightly high
free T4 and subclinical hyperthyroidism during early
pregnancy. At late pregnancy, the level of thyroid hormone
becomes relatively low. In our case, thyroid hormones
were rapidly decreased after starting thiamazole,
accompanying the rapid increase of skin lesions. These
findings suggest that thyroid hormone might have a
suppressive effect on AKE and FAH. However, two
previous reports3,6 did not clearly describe AKE deteriorated in late pregnancy. Therefore, the increased lesions
of AKE in the present case might depend on the usage
of thiamazole rather than altered thyroid functions.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download