Abstract
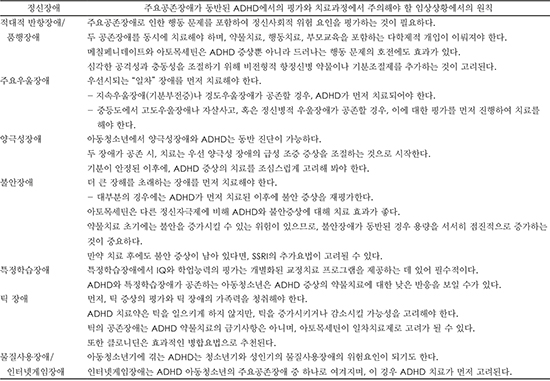
Attention-deficit hyperactivity disorder (ADHD) occurs with a high prevalence of comorbid disorders, and these comorbid disorders can affect assessment, clinical symptoms, prognosis, and treatment strategies for children with ADHD. The goal of this study was to develop a clinical practice guideline for ADHD and its specific comorbid disorders. Due to limited numbers of previous clinical studies, current recommendations are based on literature review and expert consensus among Korean child and adolescent psychiatrists. We suggest the use of multidisciplinary evaluations, interview techniques, and assessment tools in order to differentiate major comorbid disorders from ADHD. Specific ADHD comorbid disorders (e.g., medical comorbidity, oppositional defiant disorder, conduct disorder, bipolar disorder, major depressive disorder, anxiety disorder, specific learning disorder, tic disorder, and substance use disorder) have suggested treatment protocols that include pharmacological and behavioral treatments. Children and adolescents with ADHD may have comorbid disorders. The use of current clinical practice guidelines will be helpful when treating ADHD children with comorbid disorders.
References
1. Jameson ND, Sheppard BK, Lateef TM, Vande Voort JL, He JP, Merikangas KR. Medical comorbidity of attention-deficit/hyperactivity disorder in US adolescents. J Child Neurol. 2016; 31:1282–1289.

2. Cuffe SP, Visser SN, Holbrook JR, Danielson ML, Geryk LL, Wolraich ML, et al. ADHD and psychiatric comorbidity: functional outcomes in a school-based sample of children. J Atten Disord. 2015; 11. 25. [Epub]. DOI: 10.1177/1087054715613437.

3. Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006; 163:716–723.

4. Huh Y, Choi I, Song M, Kim S, Hong SD, Joung Y. A comparison of comorbidity and psychological outcomes in children and adolescents with attention-deficit/hyperactivity disorder. Psychiatry Investig. 2011; 8:95–101.

5. Pliszka S. AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2007; 46:894–921.

6. Efron D, Bryson H, Lycett K, Sciberras E. Children referred for evaluation for ADHD: comorbidity profiles and characteristics associated with a positive diagnosis. Child Care Health Dev. 2016; 42:718–724.

7. Korean Academy of Child and Adolescents Psychiatry. Adolescent Psychiatry. Seoul: Sigmapress;2012. p. 90–103.
8. Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000; 39:28–38.

9. Cho SC, Kim BN, Kim JW, Kim HW, Choi HJ, Jung SW, et al. The reliability and validity of Diagnostic Interview Schedule for Children version IV-Korean version (DISC-IV). J Korean Acad Child Adolesc Psychiatry. 2007; 18:138–144.
10. Endicott J, Spitzer RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch Gen Psychiatry. 1978; 35:837–844.
11. Kim YS, Cheon KA, Kim BN, Chang SA, Yoo HJ, Kim JW, et al. The reliability and validity of Kiddie-Schedule for Affective Disorders and Schizophrenia-Present and Lifetime version- Korean version (K-SADS-PL-K). Yonsei Med J. 2004; 45:81–89.

12. Oh K, Hong KM, Lee H, Ha E. Korean version of child behavior checklist (K-CBCL). Seoul: Chung Ang Aptitude Publishing Co;1997.
13. Cho SM, Park HY, Kim JH, Hong CH, Hwang ST. A standardization study of the Korean Personality Rating Scale for Children (KPRC). Korean J Clin Psychol. 2006; 25:825–848.
14. Lee YS, Kim SH, You JH, Baek HT, Na C, Kim BN, et al. Attention deficit hyperactivity disorder like behavioral problems and parenting stress in pediatric allergic rhinitis. Psychiatry Investig. 2014; 11:266–271.

15. Lahey BB, Loeber R, Burke JD, Applegate B. Predicting future antisocial personality disorder in males from a clinical assessment in childhood. J Consult Clin Psychol. 2005; 73:389–399.

16. Harpold T, Biederman J, Gignac M, Hammerness P, Surman C, Potter A, et al. Is oppositional defiant disorder a meaningful diagnosis in adults? Results from a large sample of adults with ADHD. J Nerv Ment Dis. 2007; 195:601–605.
17. Steinhoff KW. Special issues in the diagnosis and treatment of ADHD in adolescents. Postgrad Med. 2008; 120:60–68.

18. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Washington, DC: American Psychiatric Association;2013.
19. Danforth JS, Harvey E, Ulaszek WR, McKee TE. The outcome of group parent training for families of children with attention-deficit hyperactivity disorder and defiant/aggressive behavior. J Behav Ther Exp Psychiatry. 2006; 37:188–205.

20. Kazdin AE. Parent management training: evidence, outcomes, and issues. J Am Acad Child Adolesc Psychiatry. 1997; 36:1349–1356.

21. Spencer TJ, Abikoff HB, Connor DF, Biederman J, Pliszka SR, Boellner S, et al. Efficacy and safety of mixed amphetamine salts extended release (adderall XR) in the management of oppositional defiant disorder with or without comorbid attention-deficit/hyperactivity disorder in school-aged children and adolescents: a 4-week, multicenter, randomized, double-blind, parallel-group, placebo-controlled, forced-dose-escalation study. Clin Ther. 2006; 28:402–418.

22. Garg J, Arun P, Chavan BS. Comparative efficacy of methylphenidate and atomoxetine in oppositional defiant disorder comorbid with attention deficit hyperactivity disorder. Int J Appl Basic Med Res. 2015; 5:114–118.

23. Newcorn JH, Spencer TJ, Biederman J, Milton DR, Michelson D. Atomoxetine treatment in children and adolescents with attention-deficit/hyperactivity disorder and comorbid oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry. 2005; 44:240–248.

24. Bangs ME, Hazell P, Danckaerts M, Hoare P, Coghill DR, Wehmeier PM, et al. Atomoxetine for the treatment of attention-deficit/hyperactivity disorder and oppositional defiant disorder. Pediatrics. 2008; 121:e314–e320.

25. Palumbo DR, Sallee FR, Pelham WE Jr, Bukstein OG, Daviss WB, McDermott MP. Clonidine for attention-deficit/hyperactivity disorder: I. Efficacy and tolerability outcomes. J Am Acad Child Adolesc Psychiatry. 2008; 47:180–188.

26. Connor DF, Barkley RA, Davis HT. A pilot study of methylphenidate, clonidine, or the combination in ADHD comorbid with aggressive oppositional defiant or conduct disorder. Clin Pediatr (Phila). 2000; 39:15–25.

27. Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry. 1991; 148:564–577.

28. van Lieshout M, Luman M, Twisk JW, van Ewijk H, Groenman AP, Thissen AJ, et al. A 6-year follow-up of a large European cohort of children with attention-deficit/hyperactivity disorder-combined subtype: outcomes in late adolescence and young adulthood. Eur Child Adolesc Psychiatry. 2016; 25:1007–1017.

29. Mannuzza S, Klein RG, Moulton JL 3rd. Lifetime criminality among boys with attention deficit hyperactivity disorder: a prospective follow-up study into adulthood using official arrest records. Psychiatry Res. 2008; 160:237–246.

31. Biederman J, Faraone SV, Milberger S, Jetton JG, Chen L, Mick E, et al. Is childhood oppositional defiant disorder a precursor to adolescent conduct disorder? Findings from a four-year follow-up study of children with ADHD. J Am Acad Child Adolesc Psychiatry. 1996; 35:1193–1204.

32. Kutcher S, Aman M, Brooks SJ, Buitelaar J, van Daalen E, Fegert J, et al. International consensus statement on attention-deficit/hyperactivity disorder (ADHD) and disruptive behaviour disorders (DBDs): clinical implications and treatment practice suggestions. Eur Neuropsychopharmacol. 2004; 14:11–28.

33. MTA Cooperative Group. National Institute of Mental Health Multimodal Treatment Study of ADHD follow-up: changes in effectiveness and growth after the end of treatment. Pediatrics. 2004; 113:762–769.
34. Klein RG, Abikoff H, Klass E, Ganeles D, Seese LM, Pollack S. Clinical efficacy of methylphenidate in conduct disorder with and without attention deficit hyperactivity disorder. Arch Gen Psychiatry. 1997; 54:1073–1080.

35. Connor DF, Glatt SJ, Lopez ID, Jackson D, Melloni RH Jr. Psychopharmacology and aggression. I: a meta-analysis of stimulant effects on overt/covert aggression-related behaviors in ADHD. J Am Acad Child Adolesc Psychiatry. 2002; 41:253–261.

36. Pliszka SR. Psychiatric comorbidities in children with attention deficit hyperactivity disorder: implications for management. Paediatr Drugs. 2003; 5:741–750.

37. Pringsheim T, Hirsch L, Gardner D, Gorman DA. The pharmacological management of oppositional behaviour, conduct problems, and aggression in children and adolescents with attention-deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder: a systematic review and meta-analysis. Part 2: antipsychotics and traditional mood stabilizers. Can J Psychiatry. 2015; 60:52–61.

38. Aman MG, Bukstein OG, Gadow KD, Arnold LE, Molina BS, McNamara NK, et al. What does risperidone add to parent training and stimulant for severe aggression in child attention-deficit/hyperactivity disorder? J Am Acad Child Adolesc Psychiatry. 2014; 53:47–60.e1.

39. Armenteros JL, Lewis JE, Davalos M. Risperidone augmentation for treatment-resistant aggression in attention-deficit/hyperactivity disorder: a placebo-controlled pilot study. J Am Acad Child Adolesc Psychiatry. 2007; 46:558–565.

40. Snyder R, Turgay A, Aman M, Binder C, Fisman S, Carroll A. Risperidone Conduct Study Group. Effects of risperidone on conduct and disruptive behavior disorders in children with subaverage IQs. J Am Acad Child Adolesc Psychiatry. 2002; 41:1026–1036.

41. Malone RP, Delaney MA, Luebbert JF, Cater J, Campbell M. A double-blind placebo-controlled study of lithium in hospitalized aggressive children and adolescents with conduct disorder. Arch Gen Psychiatry. 2000; 57:649–654.

42. Donovan SJ, Stewart JW, Nunes EV, Quitkin FM, Parides M, Daniel W, et al. Divalproex treatment for youth with explosive temper and mood lability: a double-blind, placebo-controlled crossover design. Am J Psychiatry. 2000; 157:818–820.

43. Biederman J, Wilens T, Mick E, Milberger S, Spencer TJ, Faraone SV. Psychoactive substance use disorders in adults with attention deficit hyperactivity disorder (ADHD): effects of ADHD and psychiatric comorbidity. Am J Psychiatry. 1995; 152:1652–1658.

44. Diler RS, Daviss WB, Lopez A, Axelson D, Iyengar S, Birmaher B. Differentiating major depressive disorder in youths with attention deficit hyperactivity disorder. J Affect Disord. 2007; 102:125–130.

45. Biederman J, Mick E, Faraone SV. Depression in attention deficit hyperactivity disorder (ADHD) children: “true” depression or demoralization? J Affect Disord. 1998; 47:113–122.

46. Bushe CJ, Savill NC. Suicide related events and attention deficit hyperactivity disorder treatments in children and adolescents: a meta-analysis of atomoxetine and methylphenidate comparator clinical trials. Child Adolesc Psychiatry Ment Health. 2013; 7:19.

47. Agosti V, Chen Y, Levin FR. Does attention deficit hyperactivity disorder increase the risk of suicide attempts? J Affect Disord. 2011; 133:595–599.

48. Bond DJ, Hadjipavlou G, Lam RW, McIntyre RS, Beaulieu S, Schaffer A, et al. The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid attention-deficit/hyperactivity disorder. Ann Clin Psychiatry. 2012; 24:23–37.
49. Atomoxetine ADHD and Comorbid MDD Study Group. Bangs ME, Emslie GJ, Spencer TJ, Ramsey JL, Carlson C, et al. Efficacy and safety of atomoxetine in adolescents with attention-deficit/hyperactivity disorder and major depression. J Child Adolesc Psychopharmacol. 2007; 17:407–420.

50. Hughes CW, Emslie GJ, Crismon ML, Posner K, Birmaher B, Ryan N, et al. Texas Children's Medication Algorithm Project: update from Texas consensus conference panel on medication treatment of childhood major depressive disorder. J Am Acad Child Adolesc Psychiatry. 2007; 46:667–686.

51. Kratochvil CJ, Newcorn JH, Arnold LE, Duesenberg D, Emslie GJ, Quintana H, et al. Atomoxetine alone or combined with fluoxetine for treating ADHD with comorbid depressive or anxiety symptoms. J Am Acad Child Adolesc Psychiatry. 2005; 44:915–924.

52. Gammon GD, Brown TE. Fluoxetine and methylphenidate in combination for treatment of attention deficit disorder and comorbid depressive disorder. J Child Adolesc Psychopharmacol. 1993; 3:1–10.

53. Wagner KD, Ambrosini P, Rynn M, Wohlberg C, Yang R, Greenbaum MS, et al. Efficacy of sertraline in the treatment of children and adolescents with major depressive disorder: two randomized controlled trials. JAMA. 2003; 290:1033–1041.

54. Emslie GJ, Mayes TL. Mood disorders in children and adolescents: psychopharmacological treatment. Biol Psychiatry. 2001; 49:1082–1090.

55. Daviss WB, Bentivoglio P, Racusin R, Brown KM, Bostic JQ, Wiley L. Bupropion sustained release in adolescents with comorbid attention-deficit/hyperactivity disorder and depression. J Am Acad Child Adolesc Psychiatry. 2001; 40:307–314.

56. Kratochvil CJ, May DE, Silva SG, Madaan V, Puumala SE, Curry JF, et al. Treatment response in depressed adolescents with and without co-morbid attention-deficit/hyperactivity disorder in the Treatment for Adolescents with Depression Study. J Child Adolesc Psychopharmacol. 2009; 19:519–527.

57. A 14-month randomized clinical trial of treatment strategies for attention- deficit/hyperactivity disorder. The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD. Arch Gen Psychiatry. 1999; 56:1073–1086.
58. West SA, McElroy SL, Strakowski SM, Keck PE Jr, McConville BJ. Attention deficit hyperactivity disorder in adolescent mania. Am J Psychiatry. 1995; 152:271–273.

59. Biederman J, Faraone S, Mick E, Wozniak J, Chen L, Ouellette C, et al. Attention-deficit hyperactivity disorder and juvenile mania: an overlooked comorbidity? J Am Acad Child Adolesc Psychiatry. 1996; 35:997–1008.

60. Milberger S, Biederman J, Faraone SV, Murphy J, Tsuang MT. Attention deficit hyperactivity disorder and comorbid disorders: issues of overlapping symptoms. Am J Psychiatry. 1995; 152:1793–1799.

61. Donfrancesco R, Miano S, Martines F, Ferrante L, Melegari MG, Masi G. Bipolar disorder co-morbidity in children with attention deficit hyperactivity disorder. Psychiatry Res. 2011; 186:333–337.

62. Jung HY, Cho HS, Joo YH, Shin HK, Yi JS, Hwang S, et al. A validation study of the Korean-version of the Young Mania Rating Scale. J Korean Neuropsychiatr Assoc. 2003; 42:263–269.
63. Cheon KA, Shin DW, Kim B, So YS, Jun JY, Song DH. The reliability and validity of the Child Bipolar Questionnaire 2.0 (CBQ 2.0)-Korean version. J Korean Neuropsychiatr Assoc. 2008; 47:269–278.
64. Jon DI, Yoon BH, Jung HY, Ha KS, Shin YC, Bahk WM. A validation study of the Korean version Mood Disorder Questionnaire (K-MDQ). J Korean Neuropsychiatr Assoc. 2005; 44:583–590.
65. Consoli A, Bouzamondo A, Guilé JM, Lechat P, Cohen D. Comorbidity with ADHD decreases response to pharmacotherapy in children and adolescents with acute mania: evidence from a metaanalysis. Can J Psychiatry. 2007; 52:323–328.

66. Biederman J, Mick E, Bostic JQ, Prince J, Daly J, Wilens TE, et al. The naturalistic course of pharmacologic treatment of children with maniclike symptoms: a systematic chart review. J Clin Psychiatry. 1998; 59:628–637. quiz 638.

67. DelBello MP, Soutullo CA, Hendricks W, Niemeier RT, McElroy SL, Strakowski SM. Prior stimulant treatment in adolescents with bipolar disorder: association with age at onset. Bipolar Disord. 2001; 3:53–57.

68. Carlson GA, Loney J, Salisbury H, Kramer JR, Arthur C. Stimulant treatment in young boys with symptoms suggesting childhood mania: a report from a longitudinal study. J Child Adolesc Psychopharmacol. 2000; 10:175–184.

69. Liu HY, Potter MP, Woodworth KY, Yorks DM, Petty CR, Wozniak JR, et al. Pharmacologic treatments for pediatric bipolar disorder: a review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2011; 50:749–762.e39.

70. Carlson GA, Rapport MD, Kelly KL, Pataki CS. The effects of methylphenidate and lithium on attention and activity level. J Am Acad Child Adolesc Psychiatry. 1992; 31:262–270.

71. Jensen PS, Hinshaw SP, Kraemer HC, Lenora N, Newcorn JH, Abikoff HB, et al. ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. J Am Acad Child Adolesc Psychiatry. 2001; 40:147–158.

72. Byun H, Yang J, Lee M, Jang W, Yang JW, Kim JH, et al. Psychiatric comorbidity in Korean children and adolescents with attention-deficit hyperactivity disorder: psychopathology according to subtype. Yonsei Med J. 2006; 47:113–121.

73. Ter-Stepanian M, Grizenko N, Zappitelli M, Joober R. Clinical response to methylphenidate in children diagnosed with attention-deficit hyperactivity disorder and comorbid psychiatric disorders. Can J Psychiatry. 2010; 55:305–312.

74. Goez H, Back-Bennet O, Zelnik N. Differential stimulant response on attention in children with comorbid anxiety and oppositional defiant disorder. J Child Neurol. 2007; 22:538–542.

75. Barkley RA, McMurray MB, Edelbrock CS, Robbins K. Side effects of methylphenidate in children with attention deficit hyperactivity disorder: a systemic, placebo-controlled evaluation. Pediatrics. 1990; 86:184–192.

76. Diamond IR, Tannock R, Schachar RJ. Response to methylphenidate in children with ADHD and comorbid anxiety. J Am Acad Child Adolesc Psychiatry. 1999; 38:402–409.

77. Geller D, Donnelly C, Lopez F, Rubin R, Newcorn J, Sutton V, et al. Atomoxetine treatment for pediatric patients with attention-deficit/hyperactivity disorder with comorbid anxiety disorder. J Am Acad Child Adolesc Psychiatry. 2007; 46:1119–1127.

78. Snircova E, Marcincakova-Husarova V, Hrtanek I, Kulhan T, Ondrejka I, Nosalova G. Anxiety reduction on atomoxetine and methylphenidate medication in children with ADHD. Pediatr Int. 2016; 58:476–481.

79. Pliszka SR, Crismon ML, Hughes CW, Corners CK, Emslie GJ, Jensen PS, et al. The Texas Children's Medication Algorithm Project: revision of the algorithm for pharmacotherapy of attention-deficit/ hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2006; 45:642–657.

80. March JS, Swanson JM, Arnold LE, Hoza B, Conners CK, Hinshaw SP, et al. Anxiety as a predictor and outcome variable in the multimodal treatment study of children with ADHD (MTA). J Abnorm Child Psychol. 2000; 28:527–541.
81. Sciberras E, Mulraney M, Anderson V, Rapee RM, Nicholson JM, Efron D, et al. Managing anxiety in children with ADHD using cognitive-behavioral therapy: a pilot randomized controlled trial. J Atten Disord. 2015; 05. 04. [Epub]. DOI: 10.1177/1087054715584054.

82. Maric M, van Steensel FJ, Bögels SM. Parental involvement in CBT for anxiety-disordered youth revisited: family CBT outperforms child CBT in the long term for children with comorbid ADHD symptoms. J Atten Disord. 2015; 03. 09. [Epub]. DOI: 10.1177/1087054715573991.

83. Klein RG, Mannuzza S, Olazagasti MA, Roizen E, Hutchison JA, Lashua EC, et al. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012; 69:1295–1303.

84. Cao F, Bitan T, Chou TL, Burman DD, Booth JR. Deficient orthographic and phonological representations in children with dyslexia revealed by brain activation patterns. J Child Psychol Psychiatry. 2006; 47:1041–1050.

85. Richlan F. Developmental dyslexia: dysfunction of a left hemisphere reading network. Front Hum Neurosci. 2012; 6:120.

86. Yoo HK, Jung J, Lee EK, Kang SH, Park EH, Choi I. Standardization of the comprehensive learning test-reading for the diagnosis of dyslexia in Korean children and adolescents. J Korean Acad Child Adolesc Psychiatry. 2016; 27:109–118.

87. Jung JS, Lee CH, Jang HJ, Kwak SS. Comprehensive literacy program for Korean dyslexics. Seoul: Goodteacher;2014.
88. Shaywitz BA, Shaywitz SE, Blachman BA, Pugh KR, Fulbright RK, Skudlarski P, et al. Development of left occipitotemporal systems for skilled reading in children after a phonologically- based intervention. Biol Psychiatry. 2004; 55:926–933.

89. Keulers EH, Hendriksen JG, Feron FJ, Wassenberg R, Wuisman-Frerker MG, Jolles J, et al. Methylphenidate improves reading performance in children with attention deficit hyperactivity disorder and comorbid dyslexia: an unblinded clinical trial. Eur J Paediatr Neurol. 2007; 11:21–28.

90. Grizenko N, Bhat M, Schwartz G, Ter-Stepanian M, Joober R. Efficacy of methylphenidate in children with attention-deficit hyperactivity disorder and learning disabilities: a randomized crossover trial. J Psychiatry Neurosci. 2006; 31:46–51.
91. Wietecha L, Williams D, Shaywitz S, Shaywitz B, Hooper SR, Wigal SB, et al. Atomoxetine improved attention in children and adolescents with attention-deficit/hyperactivity disorder and dyslexia in a 16 week, acute, randomized, double-blind trial. J Child Adolesc Psychopharmacol. 2013; 23:605–613.

92. Rothenberger A, Roessner V, Banaschewski T, Leckman JF. Co-existence of tic disorders and attention-deficit/hyperactivity disorder-recent advances in understanding and treatment. Eur Child Adolesc Psychiatry. 2007; 16:Suppl 1. 1–4.

93. Leckman JF, Riddle MA, Hardin MT, Ort SI, Swartz KL, Stevenson J, et al. The Yale Global Tic Severity Scale: initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adolesc Psychiatry. 1989; 28:566–573.

94. Chung SJ, Lee JS, Yoo TI, Koo YJ, Jeon SI, Kim BS, et al. Development of the Korean Form of Yale Global Tic Severity Scale: a validity and reliability study. J Korean Neuropsychiatr Assoc. 1998; 37:942–951.
95. Cohen SC, Mulqueen JM, Ferracioli-Oda E, Stuckelman ZD, Coughlin CG, Leckman JF, et al. Meta-analysis: risk of tics associated with psychostimulant use in randomized, placebo-controlled trials. J Am Acad Child Adolesc Psychiatry. 2015; 54:728–736.

96. Bloch MH, Panza KE, Landeros-Weisenberger A, Leckman JF. Meta-analysis: treatment of attention-deficit/hyperactivity disorder in children with comorbid tic disorders. J Am Acad Child Adolesc Psychiatry. 2009; 48:884–893.

97. Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin Psychol Rev. 2011; 31:328–341.

98. Wilens TE, Martelon M, Joshi G, Bateman C, Fried R, Petty C, et al. Does ADHD predict substance-use disorders? A 10-year follow-up study of young adults with ADHD. J Am Acad Child Adolesc Psychiatry. 2011; 50:543–553.

99. Knecht C, de Alvaro R, Martinez-Raga J, Balanza-Martinez V. Attention-deficit hyperactivity disorder (ADHD), substance use disorders, and criminality: a difficult problem with complex solutions. Int J Adolesc Med Health. 2015; 27:163–175.

100. Yoo HJ, Cho SC, Ha J, Yune SK, Kim SJ, Hwang J, et al. Attention deficit hyperactivity symptoms and internet addiction. Psychiatry Clin Neurosci. 2004; 58:487–494.

101. Bae S, Han DH, Kim SM, Shi X, Renshaw PF. Neurochemical correlates of internet game play in adolescents with attention deficit hyperactivity disorder: a proton magnetic resonance spectroscopy (MRS) study. Psychiatry Res. 2016; 254:10–17.

102. Han DH, Kim SM, Bae S, Renshaw PF, Anderson JS. Brain connectivity and psychiatric comorbidity in adolescents with internet gaming disorder. Addict Biol. 2015; 12. 22. [Epub]. DOI: 10.1111/adb.12347.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download