Abstract
Objectives
There is evidence that Hypothalamic-Pituitary-Adrenocortical (HPA) system dysregulation plays a role in the pathophysiology of depression. However which psychiatric symptoms are related to HPA system dysregulation has not been studied well. The primary aim of this study was to investigate which symptom components of the Hamilton Depression Rating Scale (HAM-D) are related to HPA system dysregulation in Korean psychiatric outpatients. The secondary aim was to find other variables that have association with HAM-D components.
Methods
This study was a retrospective review of the charts of outpatients who first visited Samsung Medical Center Depression Clinic between July 2012 and October 2013. Among them those who checked the plasma cortisol level and HAM-D within one week of their first visit were selected. Fifty nine patients were selected. The HAM-D was divided into four components, including depression, anxiety, insomnia, and somatic components. Multiple regression of cortisol level was used for four subscales.
Results
Significant positive correlations were observed between the plasma cortisol level and depression component of HAM-D (beta=0.251, p=0.049). Age also showed negative correlation with the depression component of HAM-D (beta=-0.427, p=0.002). However anxiety, insomnia and somatic components of HAM-D did not show correlation with plasma cortisol level.
Figures and Tables
Fig. 1
Relationship between cortisol level and depression component of HAM-D. Cortisol : Square root transformation of raw cortisol level data, Depression : Depression component of HAM-D, HAM-D : Hamilton Depression Rating Scale.
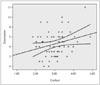
Table 2
Association between HAM-D depression component and plasma cortisol level by multiple linear regression analysis

References
1. Lépine JP, Briley M. The increasing burden of depression. Neuropsychiatr Dis Treat. 2011; 7:Suppl 1. 3–7.
2. Cho MJ, Park JI, Bae A, Bae JN, Sohn JW, Ahn JH, et al. The epidemiological survey of mental disorders in Korea [Internet]. Seoul: Seoul National University College of Medicine;2011. cited 2014 Oct 6. Available from: http://www.google.co.kr/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=1&ved=0CCIQFjAA&url=http%3A%2F%2Fstat.mw.go.kr%2Ffront%2Finclude%2Fdownload.jsp%3FbbsSeq%3D13%26nttSeq%3D18458%26atchSeq%3D3026&ei=shYqVJKXEoeE8gWkk4GADg&usg=AFQjCNGSD11Yht8HJQLZnkYnvaRS14aYlQ&bvm=bv.76477589,d.dGc&cad=rjt.
3. Akil HA, Morano MI. Stress. In : Bloom FE, Kupfer DJ, editors. Psychopharmacology: the fourth generation of progress. New York: Raven Press;1995. p. 773–785.
4. Chrousos GP, Gold PW. The concepts of stress and stress system disorders. Overview of physical and behavioral homeostasis. JAMA. 1992; 267:1244–1252.

5. Tafet GE, Idoyaga-Vargas VP, Abulafia DP, Calandria JM, Roffman SS, Chiovetta A, et al. Correlation between cortisol level and serotonin uptake in patients with chronic stress and depression. Cogn Affect Behav Neurosci. 2001; 1:388–393.

6. Burke HM, Davis MC, Otte C, Mohr DC. Depression and cortisol responses to psychological stress: a meta-analysis. Psychoneuroendocrinology. 2005; 30:846–856.

7. Keller J, Flores B, Gomez RG, Solvason HB, Kenna H, Williams GH, et al. Cortisol circadian rhythm alterations in psychotic major depression. Biol Psychiatry. 2006; 60:275–281.

8. Faraj BA, Olkowski ZL, Jackson RT. Expression of a high-affinity serotonin transporter in human lymphocytes. Int J Immunopharmacol. 1994; 16:561–567.

9. Faraj BA, Olkowski ZL, Jackson RT. Prevalence of high serotonin uptake in lymphocytes of abstinent alcoholics. Biochem Pharmacol. 1997; 53:53–57.

10. Pariante CM. The glucocorticoid receptor: part of the solution or part of the problem? J Psychopharmacol. 2006; 20:4 Suppl. 79–84.

11. Sapolsky RM. The possibility of neurotoxicity in the hippocampus in major depression: a primer on neuron death. Biol Psychiatry. 2000; 48:755–765.

12. Yeo HB, Kim L, Ham BJ, Shim SH, Kwon YJ, Jung HY, et al. Association between Somatic Component of the Hamilton Depression Rating Scale and the Plasma ACTH & Serum Cortisol Level in Korean Patients with Major Depressive Disorder. J Korean Soc Biol Ther Psychiatry. 2011; 17:205–210.
13. Shafer AB. Meta-analysis of the factor structures of four depression questionnaires: Beck, CES-D, Hamilton, and Zung. J Clin Psychol. 2006; 62:123–146.

14. Emedicine.medscape.com [homepage on the Internet] WebMD LLC c1994-2014. cited 2014 Oct 6. Available from: http://emedicine.medscape.com/article/2088826-overview.
15. Yehuda R, Teicher MH, Trestman RL, Levengood RA, Siever LJ. Cortisol regulation in posttraumatic stress disorder and major depression: a chronobiological analysis. Biol Psychiatry. 1996; 40:79–88.

16. Deuschle M, Schweiger U, Weber B, Gotthardt U, Körner A, Schmider J, et al. Diurnal activity and pulsatility of the hypothalamus-pituitary-adrenal system in male depressed patients and healthy controls. J Clin Endocrinol Metab. 1997; 82:234–238.

17. Nelson JC, Davis JM. DST studies in psychotic depression: a meta-analysis. Am J Psychiatry. 1997; 154:1497–1503.

18. Sachar EJ, Hellman L, Roffwarg HP, Halpern FS, Fukushima DK, Gallagher TF. Disrupted 24-hour patterns of cortisol secretion in psychotic depression. Arch Gen Psychiatry. 1973; 28:19–24.

19. Posener JA, DeBattista C, Williams GH, Chmura Kraemer H, Kalehzan BM, Schatzberg AF. 24-Hour monitoring of cortisol and corticotropin secretion in psychotic and nonpsychotic major depression. Arch Gen Psychiatry. 2000; 57:755–760.

20. Watson S, Gallagher P, Del-Estal D, Hearn A, Ferrier IN, Young AH. Hypothalamic-pituitary-adrenal axis function in patients with chronic depression. Psychol Med. 2002; 32:1021–1028.

21. Rybakowski JK, Twardowska K. The dexamethasone/corticotropin-releasing hormone test in depression in bipolar and unipolar affective illness. J Psychiatr Res. 1999; 33:363–370.

22. Strickland PL, Deakin JF, Percival C, Dixon J, Gater RA, Goldberg DP. Bio-social origins of depression in the community. Interactions between social adversity, cortisol and serotonin neurotransmission. Br J Psychiatry. 2002; 180:168–173.
23. Webster EL, Torpy DJ, Elenkov IJ, Chrousos GP. Corticotropin-releasing hormone and inflammation. Ann N Y Acad Sci. 1998; 840:21–32.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download