Abstract
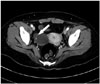
Paraneoplastic limbic encephalitis associated with ovarian teratoma has variable clinical manifestations, including hallucination, abnormal behavior, amnesia, mental change, fever, chorea and dystonia, and often has antibodies to N-methyl-D-aspartate receptor (NMDAR), however cases without tumor or antibodies to NMDAR have also been reported. Here, we describe a 35-year-old female who was initially misdiagnosed as schizophrenia because she presented with acute onset of psychiatric symptoms, including visual hallucination, abnormal behavior, confusion, and memory impairment. Three days after admission, she developed high fever refractory to antibiotics. Brain MRI and examination of cerebrospinal fluid were normal. Computerized tomography of the pelvis showed an ovarian teratoma. The patient showed complete improvement after surgical removal of the ovarian teratoma and steroid therapy. We suggest that physicians should consider the possibility of paraneoplastic limbic encephalitis in patients who present with acute onset of psychiatric symptoms with high fever or movement disorder.
Figures and Tables
References
1. Thieben MJ, Lennon VA, Boeve BF, Aksamit AJ, Keegan M, Vernino S. Potentially reversible autoimmune limbic encephalitis with neuronal potassium channel antibody. Neurology. 2004; 62:1177–1182.

2. Gultekin SH, Rosenfeld MR, Voltz R, Eichen J, Posner JB, Dalmau J. Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patients. Brain. 2000; 123(Pt 7):1481–1494.

3. Aydiner A, Gürvit H, Baral I. Paraneoplastic limbic encephalitis with immature ovarian teratoma--a case report. J Neurooncol. 1998; 37:63–66.
4. Cho HJ, Jo JW, Park KP, Kim DS, Park KH, Jung DS. A case of paraneoplastic limbic encephalitis associated with immature ovarian teratoma. J Korean Neurol Assoc. 2003; 21:647–650.
5. Lee HS, Kim SW, Chung SJ, Yoo HS, Lee PH, Choi SA. Anti-NMDA receptor encephalitis which has shown clinical symptoms of schizophrenia. J Korean Neurol Assoc. 2013; 31:115–117.
6. Granerod J, Crowcroft NS. The epidemiology of acute encephalitis. Neuropsychol Rehabil. 2007; 17:406–428.

7. Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010; 10:835–844.

8. Lee EM, Kang JK. Autoimmune encephalitis. J Neurocrit Care. 2013; 6:8–15.
9. Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008; 7:1091–1098.

10. Cakirer S. Paraneoplastic limbic encephalitis: case report. Comput Med Imaging Graph. 2002; 26:55–58.

11. Lennox BR, Coles AJ, Vincent A. Antibody-mediated encephalitis: a treatable cause of schizophrenia. Br J Psychiatry. 2012; 200:92–94.

12. Irani SR, Vincent A. NMDA receptor antibody encephalitis. Curr Neurol Neurosci Rep. 2011; 11:298–304.

13. Malter MP, Helmstaedter C, Urbach H, Vincent A, Bien CG. Antibodies to glutamic acid decarboxylase define a form of limbic encephalitis. Ann Neurol. 2010; 67:470–478.

14. Lai M, Hughes EG, Peng X, Zhou L, Gleichman AJ, Shu H, et al. AMPA receptor antibodies in limbic encephalitis alter synaptic receptor location. Ann Neurol. 2009; 65:424–434.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download