Abstract
Objectives
Previous studies have reported that symptoms of patients with major depressive disorder (MDD) are different according to age groups, and the Hamilton Depression Rating Scale (HDRS) is the most widely used measure to evaluate the symptoms of MDD. However, few previous studies have compared the symptoms of HDRS between the elderly and non-elderly groups.
Methods
The study population consisted of 574 subjects with MDD who were ≥18 years old, evaluated using the Mini International Neuropsychiatric Interview and 17 items of HDRS. Differences between two groups were analyzed using independent t-test. A multivariate logistic regression model was used to evaluate associations between age and 17 items from HDRS after controlling for gender, years of education, marital status, and employment status.
Results
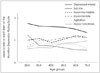
Among 574 patients with MDD, there were 80 elderly patients (age≥65) and 494 non-elderly patients (age between 18 and 64). Elderly patients had higher scores on item 5 (middle insomnia) (t=-2.271, p=0.024) and item 6 (late insomnia) (t=-2.280, p=0.023), whereas they had lower scores on item 1 (depressed mood) (t=2.860, p=0.004), item 3 (suicide) (t=2.258, p=0.024), and item 9 (agitation) (t=2.031, p=0.043), although no significant difference in the total HDRS scores was observed between elderly and non-elderly. Multivariate logistic regression showed significant association of elderly with hypochondriasis [adjusted odds ratio (AOR)=1.894, 95% confidence interval (CI) 1.01-3.56] and agitation (AOR=0.50, 95% CI 0.29-0.87).
Figures and Tables
References
1. Cho MJ, Park JI, Bae A, Bae JN, Sohn JW, Ahn JH, et al. The epidemiological survey of mental disorders in Korea [Internet]. Seoul: Seoul National University College of Medicine;2011. cited 2014 Oct 6. Available from: http://www.google.co.kr/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=1&ved=0CCIQFjAA&url=http%3A%2F%2Fstat.mw.go.kr%2Ffront%2Finclude%2Fdownload.jsp%3FbbsSeq%3D13%26nttSeq%3D18458%26atchSeq%3D3026&ei=shYqVJKXEoeE8gWkk4GADg&usg=AFQjCNGSD11Yht8HJQLZnkYnvaRS14aYlQ&bvm=bv.76477589,d.dGc&cad=rjt.
3. Sadock BJ, Sadock VA, Ruiz P. Kaplan and Sadock's Synopsis of Psychiatry: behavioral sciences/clinical psychiatry. 11th ed. Philadelphia, PA: Wolters Kluwer Health;2014.
4. Arai H, Ouchi Y, Yokode M, Ito H, Uematsu H, Eto F, et al. Toward the realization of a better aged society: messages from gerontology and geriatrics. Geriatr Gerontol Int. 2012; 12:16–22.

5. Lebowitz BD, Pearson JL, Schneider LS, Reynolds CF 3rd, Alexopoulos GS, Bruce ML, et al. Diagnosis and treatment of depression in late life. Consensus statement update. JAMA. 1997; 278:1186–1190.

6. Lyness JM, Cox C, Curry J, Conwell Y, King DA, Caine ED. Older age and the underreporting of depressive symptoms. J Am Geriatr Soc. 1995; 43:216–221.

7. Gottfries CG. Is there a difference between elderly and younger patients with regard to the symptomatology and aetiology of depression? Int Clin Psychopharmacol. 1998; 13:Suppl 5. S13–S18.

8. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, DC: American Psychiatric Association;2013.
9. VanItallie TB. Subsyndromal depression in the elderly: underdiagnosed and undertreated. Metabolism. 2005; 54:5 Suppl 1. 39–44.

10. Beheydt LL, Schrijvers D, Docx L, Bouckaert F, Hulstijn W, Sabbe B. Psychomotor retardation in elderly untreated depressed patients. Front Psychiatry. 2015; 5:196.

11. Shahpesandy H. Different manifestation of depressive disorder in the elderly. Neuro Endocrinol Lett. 2005; 26:691–695.
12. Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003; 160:1147–1156.

13. Tan LL, Ng LL, Tan S, Roy K, Brodaty H, Parker G. Depression in Singapore: failure to demonstrate an age effect on clinical features. Int J Geriatr Psychiatry. 2001; 16:1054–1060.

14. Hong SW, Lee DS, Jae YM, Jang SH, Choi JH, Jang YK, et al. Comparison of Depressive Symptoms of Major Depressive Disorder between Elderly and Non-Elderly Group in Busan City in South Korea. J Korean Soc Biol Ther Psychiatry. 2008; 14:58–63.
15. Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967; 6:278–296.

16. Hirschfeld RM, Williams JB, Spitzer RL, Calabrese JR, Flynn L, Keck PE Jr, et al. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000; 157:1873–1875.

17. Angst J, Adolfsson R, Benazzi F, Gamma A, Hantouche E, Meyer TD, et al. The HCL-32: towards a self-assessment tool for hypomanic symptoms in outpatients. J Affect Disord. 2005; 88:217–233.

18. Oh MY, Angst J, Sung TH, Lee EH, Hong KS, Lee DS, et al. Reliability and validity of the Hypomania Symptom Checklist-32 in Korea. Korean J Clin Psychol. 2009; 28:321–338.

19. Jon DI, Hong N, Yoon BH, Jung HY, Ha K, Shin YC, et al. Validity and reliability of the Korean version of the Mood Disorder Questionnaire. Compr Psychiatry. 2009; 50:286–291.

20. Salzman C. Pharmacologic treatment of depression in the elderly. J Clin Psychiatry. 1993; 54:Suppl. 23–28.
21. Livingston G, Watkin V, Milne B, Manela MV, Katona C. The natural history of depression and the anxiety disorders in older people: the Islington community study. J Affect Disord. 1997; 46:255–262.

22. Sloan EP, Flint AJ, Reinish L, Shapiro CM. Circadian rhythms and psychiatric disorders in the elderly. J Geriatr Psychiatry Neurol. 1996; 9:164–170.

23. Leblanc MF, Desjardins S, Desgagné A. The relationship between sleep habits, anxiety, and depression in the elderly. Nat Sci Sleep. 2015; 7:33–42.
24. Leblanc MF, Desjardins S, Desgagné A. Sleep cognitions associated with anxiety and depression in the elderly. Clin Interv Aging. 2015; 10:575–582.
25. Lôo H, Gallarda T, Fabre I, Olié JP. [Depression and aging]. Bull Acad Natl Med. 2004; 188:999–1007. discussion 1007-1010
26. DeLamater J, Karraker A. Sexual functioning in older adults. Curr Psychiatry Rep. 2009; 11:6–11.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download