Abstract
Objectives
The aim of this study was to investigate the treatment effect and predictors of response of affect regulation group therapy (ARGT) delivered to a group of recently traumatized children.
Methods
A total of 464 school children, who had witnessed or confronted a tragic accident at school, were given a single-session of affect regulation group therapy, that which included psychoeducation and affect regulation elements from eye movement desensitization and reprocessing. Of 213 children whose with initial score of Subject Unit of Disturbance Scale (SUDS) score over 4, we compared pre- and post-treatment scores and performed conducted the responder vs. non-responder comparison. The pPost-traumatic disorder (PTSD) symptom scores measured by using Child Reaction to Traumatic Events Scale-Revised (CRTES-R), demographic variables, and clinical variables were considered.
Results
Affect regulation group therapy was effective for children who had experienced an acute traumatic event (t=16.3, p<0.001). Baseline SUDS score of for non-responder were was significantly higher (t=-2.89, p<0.001) and CRTES-R score approached a level of significance level (t=-1.72, p=0.09). However, results of logistic regression analysis identified showed that the pretreatment SUDS score was the only significant predictor of non-response.
Figures and Tables
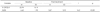
Table 4
Stepwise forward logistic regression analysis of affect regulation group therapy : responder* vs. non-responder category as dependent variable

Explanatory variables entered on step 1 : Baseline SUDS scores, Baseline K-CRTES-R scores. *: Those who showed more than 50% decrease in SUDS score after treatment. K-CRTES-R : Korean-Child Reaction to Traumatic Events Scale-Revised, SUDS : Subject Unit of Disturbance Scale, CI : Confidence interval
References
1. Brunello N, Davidson JR, Deahl M, Kessler RC, Mendlewicz J, Racagni G, et al. Posttraumatic stress disorder: diagnosis and epidemiology, comorbidity and social consequences, biology and treatment. Neuropsychobiology. 2001; 43:150–162.

2. American Psychiatric Association. Posttraumatic Stress Disorder. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington: American Psychiatric Association;1994. p. 424–429.
3. Stein BD, Jaycox LH, Kataoka S, Rhodes HJ, Vestal KD. Prevalence of child and adolescent exposure to community violence. Clin Child Fam Psychol Rev. 2003; 6:247–264.

4. Finkelhor D, Ormrod R, Turner H, Hamby SL. The victimization of children and youth: a comprehensive, national survey. Child Maltreat. 2005; 10:5–25.

5. Costello EJ, Erkanli A, Fairbank JA, Angold A. The prevalence of potentially traumatic events in childhood and adolescence. J Trauma Stress. 2002; 15:99–112.

6. Breslau N, Davis GC. Posttraumatic stress disorder in an urban population of young adults: risk factors for chronicity. Am J Psychiatry. 1992; 149:671–675.

7. Zehnder D, Landolt MA, Hornung R. [Early psychological interventions in children after trauma]. Prax Kinderpsychol Kinderpsychiatr. 2006; 55:675–692.
8. Zehnder D, Meuli M, Landolt MA. Effectiveness of a single-session early psychological intervention for children after road traffic accidents: a randomised controlled trial. Child Adolesc Psychiatry Ment Health. 2010; 4:7.

9. Stallard P, Velleman R, Salter E, Howse I, Yule W, Taylor G. A randomised controlled trial to determine the effectiveness of an early psychological intervention with children involved in road traffic accidents. J Child Psychol Psychiatry. 2006; 47:127–134.

10. Agorastos A, Marmar CR, Otte C. Immediate and early behavioral interventions for the prevention of acute and posttraumatic stress disorder. Curr Opin Psychiatry. 2011; 24:526–532.

11. Kornør H, Winje D, Ekeberg Ø, Weisaeth L, Kirkehei I, Johansen K, et al. Early trauma-focused cognitive-behavioural therapy to prevent chronic post-traumatic stress disorder and related symptoms: a systematic review and meta-analysis. BMC Psychiatry. 2008; 8:81.

12. Roberts NP, Kitchiner NJ, Kenardy J, Bisson JI. Systematic review and meta-analysis of multiple-session early interventions following traumatic events. Am J Psychiatry. 2009; 166:293–301.

13. van Emmerik AA, Kamphuis JH, Hulsbosch AM, Emmelkamp PM. Single session debriefing after psychological trauma: a meta-analysis. Lancet. 2002; 360:766–771.

14. Rose S, Bisson J, Wessely S. A systematic review of single-session psychological interventions ('debriefing') following trauma. Psychother Psychosom. 2003; 72:176–184.

15. van der Kolk BA, Pelcovitz D, Roth S, Mandel FS, McFarlane A, Herman JL. Dissociation, somatization, and affect dysregulation: the complexity of adaptation of trauma. Am J Psychiatry. 1996; 153:7 Suppl. 83–93.

16. Silva RR, Cloitre M, Davis L, Levitt J, Gomez S, Ngai I, et al. Early intervention with traumatized children. Psychiatr Q. 2003; 74:333–347.

17. Kim BN, Kim JW, Kim HW, Shin MS, Cho SC, Choi NH, et al. A 6-month follow-up study of posttraumatic stress and anxiety/depressive symptoms in Korean children after direct or indirect exposure to a single incident of trauma. J Clin Psychiatry. 2009; 70:1148–1154.

18. Jeong Y, Kim D, Bae H, Kim SH, Go B, Kim SH. Factorial validity and psychometric properties of the Korean version of the children's response to traumatic events scale-revised in recently traumatized school children. J Korean Neuropsychiatr Assoc. 2012; 51:185–191.

19. Chen Y, Fortson BL, Lai Y, Lee Y. Psychometric properties of the Chinese version of the Child's Reaction to Traumatic Events Scale. In : Poster presented at 24th International Society for Traumatic Stress Studies Annual Meeting; 2008 Nov 13-15; Chicago, USA. 2008.
20. Kim D, Bae H, Park YC. Validity of the subjective Units of Disturbance Scale in EMDR. J EMDR Res Pract. 2008; 2:57–62.

21. Shapiro F. Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols, and Procedures. 2nd ed. New York: Guilford Press;2001.
22. Jarero I, Artigas L, Hartung J. EMDR integrative group treatment protocol: a postdisaster trauma intervention for children and adults. Traumatology. 2006; 12:121–129.

23. Omaha J. Psychotherapeutic Interventions for Emotion Regulation: EMDR and Bilateral Stimulation for Affective Management. New York: W.W. Norton & Company Inc.;2004. p. 211–239.
24. TF-CBT Web: a web-based learning course for trauma-focused cognitive-behavioral therapy. Medical University of South Carolina;c2005. cited 2013 Sep 13. Available from http://tfcbt.musc.edu.
25. Cloitre M, Stovall-McClough KC, Nooner K, Zorbas P, Cherry S, Jackson CL, et al. Treatment for PTSD related to childhood abuse: a randomized controlled trial. Am J Psychiatry. 2010; 167:915–924.

26. Hizli FG, Taskintuna N, Isikli S, Kilic C, Zileli L. Predictors of posttraumatic stress in children and adolescents. Child Youth Serv Rev. 2009; 31:349–354.

27. Kinzie JD, Goetz RR. A century of controversy surrounding posttraumatic stress stress-spectrum syndromes: the impact on DSM-III and DSM-IV. J Trauma Stress. 1996; 9:159–179.

28. Roemer L, Orsillo SM, Borkovec TD, Litz BT. Emotional response at the time of a potentially traumatizing event and PTSD symptomatology: a preliminary retrospective analysis of the DSM-IV Criterion A-2. J Behav Ther Exp Psychiatry. 1998; 29:123–130.

29. Brewin CR, Andrews B, Rose S. Fear, helplessness, and horror in posttraumatic stress disorder: investigating DSM-IV criterion A2 in victims of violent crime. J Trauma Stress. 2000; 13:499–509.

30. Taylor S, Fedoroff IC, Koch WJ, Thordarson DS, Fecteau G, Nicki RM. Posttraumatic stress disorder arising after road traffic collisions: patterns of response to cognitive-behavior therapy. J Consult Clin Psychol. 2001; 69:541–551.

31. Berntsen D, Johannessen KB, Thomsen YD, Bertelsen M, Hoyle RH, Rubin DC. Peace and war: trajectories of posttraumatic stress disorder symptoms before, during, and after military deployment in Afghanistan. Psychol Sci. 2012; 23:1557–1565.
32. Verlinden E, Schippers M, Van Meijel EP, Beer R, Opmeer BC, Olff M, et al. What makes a life event traumatic for a child? The predictive values of DSM-Criteria A1 and A2. Eur J Psychotraumatol. 2013; 4.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download