Abstract
Objectives
The aim of this study was to analyze the environmental and familial variables associated with attention-deficit/hyperactivity disorder (ADHD) in children and adolescents.
Methods
Children and adolescents aged 6-18 with in attention, hyperactivity, or impulsivity who visited the Department of Psychiatry at Soonchunhyang University Bucheon Hospital from April 2006 to April 2012, were interviewed for diagnosis of ADHD. Diagnostic and Statistical Manual of Mental Disorders, 4th edition symptom criteria for ADHD were assessed using a semi-structured interview, the schedule for affective disorders and schizophrenia for school-age children present and lifetime version (K-SADS-PL). Environmental and familial variables were obtained using questionnaires for parents.
Results
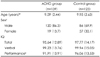
In total, 262 children and adolescents with ADHD (n=139) and control subjects (n=123) were recruited. In a multivariate logistic regression model, results of this study showed that maternal psychiatric problem during pregnancy, dystoia, forceps/vacuum use during delivery, and unplanned pregnancy were risk factors for ADHD.
Conclusion
Findings of this study showed an association of some prenatal factors (such as unplanned pregnancy or maternal psychiatric problem during pregnancy) and some perinatal factors (dystocia and forceps/vacuum use during delivery) with increased risk of ADHD. The identified risk factors are environmental, and therefore potentially preventable. Conduct of further prospective studies is needed in order to clarify the potential role of these risk factors for ADHD.
Figures and Tables
References
1. Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007. 164:942–948.

2. Popper CW, Gammon GD, West SA, Bailey CE. Hales RE, Yodofsky S, editors. Disorders usually first diagnosed in infancy, childhood or adolescence. Textbook of clinical psychiatry. 2003. 4th ed. Washington (DC): American Psychiatric Publishing Inc;833–974.
3. Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, et al. Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005. 57:1313–1323.

4. Freitag CM, Hänig S, Schneider A, Seitz C, Palmason H, Retz W, et al. Biological and psychosocial environmental risk factors influence symptom severity and psychiatric comorbidity in children with ADHD. J Neural Transm. 2012. 119:81–94.

5. Pineda DA, Palacio LG, Puerta IC, Merchán V, Arango CP, Galvis AY, et al. Environmental influences that affect attention deficit/hyperactivity disorder: study of a genetic isolate. Eur Child Adolesc Psychiatry. 2007. 16:337–346.

6. Milberger S, Biederman J, Faraone SV, Guite J, Tsuang MT. Pregnancy, delivery and infancy complications and attention deficit hyperactivity disorder: issues of gene-environment interaction. Biol Psychiatry. 1997. 41:65–75.

7. Kim BN. Pregnancy, delivery and perinatal risk factors associated with symptoms of attention deficit/hyperactivity disorder: community study. J Korean Neuropsychiatr Assoc. 2002. 41:263–273.
8. Kim JW. Environmental risk factors for attention deficit hyperactivity disorder and implications for clinical practice. J Korean Acad Child Adolesc Psychiatry. 2011. 22:10–15.

9. Biederman J, Milberger S, Faraone SV, Kiely K, Guite J, Mick E, et al. Family-environment risk factors for attention-deficit hyperactivity disorder. A test of Rutter's indicators of adversity. Arch Gen Psychiatry. 1995. 52:464–470.

10. Park S, Jeong HW, Kim BN, Cho SC, Kim JW, Shin MS, et al. Perinatal and developmental risk factors of ADHD children diagnosed with a structured interview. J Korean Acad Child Adolesc Psychiatry. 2012. 23:181–187.

11. Kim YS, Cheon KA, Kim BN, Yoo JH, Kim JW, So YK, et al. Kiddie-schedule for affective disorders and schizophrenia-present and lifetime version-Korean version (K-SADS-PL-K). 2003. Seoul: JungAng Moonwha Co.
12. Kwak GJ, Park HY, Kim CT. The Korean Wechsler Intelligence Scale for Children-III(K-WISC-III) Guide. 2001. Seoul: Doseochulpan Teuksugyoyuk.
13. Motlagh MG, Katsovich L, Thompson N, Lin H, Kim YS, Scahill L, et al. Severe psychosocial stress and heavy cigarette smoking during pregnancy: an examination of the pre- and perinatal risk factors associated with ADHD and Tourette syndrome. Eur Child Adolesc Psychiatry. 2010. 19:755–764.

14. O'Connor TG, Heron J, Golding J, Beveridge M, Glover V. Maternal antenatal anxiety and children's behavioural/emotional problems at 4 years. Report from the Avon Longitudinal Study of Parents and Children. Br J Psychiatry. 2002. 180:502–508.
15. Grizenko N, Fortier ME, Zadorozny C, Thakur G, Schmitz N, Duval R, et al. Maternal Stress during Pregnancy, ADHD Symptomatology in Children and Genotype: Gene-Environment Interaction. J Can Acad Child Adolesc Psychiatry. 2012. 21:9–15.
16. Van den Bergh BR, Mulder EJ, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: links and possible mechanisms. A review. Neurosci Biobehav Rev. 2005. 29:237–258.

17. Kim HW, Cho SC, Kim BN, Kim JW, Shin MS, Kim Y. Perinatal and familial risk factors are associated with full syndrome and subthreshold attention-deficit hyperactivity disorder in a korean community sample. Psychiatry Investig. 2009. 6:278–285.

18. Field T, Diego M, Dieter J, Reif MH, Schanberg S, Kuhn C, et al. Prenatal depression effects on the fetus and the newborn. Infant Behav Dev. 2004. 27:216–229.

19. Seckl JR, Holmes MC. Mechanisms of disease: glucocorticoids, their placental metabolism and fetal 'programming' of adult pathophysiology. Nat Clin Pract Endocrinol Metab. 2007. 3:479–488.

20. Plotsky PM, Cunningham ET Jr, Widmaier EP. Catecholaminergic modulation of corticotropin-releasing factor and adrenocorticotropin secretion. Endocr Rev. 1989. 10:437–458.

21. Lee SH, Shin DW, Stein MA. Increased cortisol after stress is associated with variability in response time in ADHD children. Yonsei Med J. 2010. 51:206–211.

22. Hedegaard M, Henriksen TB, Secher NJ, Hatch MC, Sabroe S. Do stressful life events affect duration of gestation and risk of preterm delivery? Epidemiology. 1996. 7:339–345.

23. Yanikkerem E, Ay S, Piro N. Planned and unplanned pregnancy: effects on health practice and depression during pregnancy. J Obstet Gynaecol Res. 2013. 39:180–187.

24. Hayatbakhsh MR, Najman JM, Khatun M, Al Mamun A, Bor W, Clavarino A. A longitudinal study of child mental health and problem behaviours at 14 years of age following unplanned pregnancy. Psychiatry Res. 2011. 185:200–204.

25. Sprich-Buckminster S, Biederman J, Milberger S, Faraone SV, Lehman BK. Are perinatal complications relevant to the manifestation of ADD? Issues of comorbidity and familiality. J Am Acad Child Adolesc Psychiatry. 1993. 32:1032–1037.

26. Hynd GW, Hern KL, Novey ES, Eliopulos D, Marshall R, Gonzalez JJ, et al. Attention deficit-hyperactivity disorder and asymmetry of the caudate nucleus. J Child Neurol. 1993. 8:339–347.

27. Castellanos FX, Giedd JN, Marsh WL, Hamburger SD, Vaituzis AC, Dickstein DP, et al. Quantitative brain magnetic resonance imaging in attention-deficit hyperactivity disorder. Arch Gen Psychiatry. 1996. 53:607–616.

28. Thakur GA, Sengupta SM, Grizenko N, Schmitz N, Pagé V, Joober R. Maternal smoking during pregnancy and ADHD: a comprehensive clinical and neurocognitive characterization. Nicotine Tob Res. 2013. 15:149–157.

29. Huizink AC, Mulder EJ. Maternal smoking, drinking or cannabis use during pregnancy and neurobehavioral and cognitive functioning in human offspring. Neurosci Biobehav Rev. 2006. 30:24–41.

30. Knopik VS, Sparrow EP, Madden PA, Bucholz KK, Hudziak JJ, Reich W, et al. Contributions of parental alcoholism, prenatal substance exposure, and genetic transmission to child ADHD risk: a female twin study. Psychol Med. 2005. 35:625–635.

31. Mitchell RJ, Brewster D, Campbell H, Porteous ME, Wyllie AH, Bird CC, et al. Accuracy of reporting of family history of colorectal cancer. Gut. 2004. 53:291–295.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download