Abstract
Background and Objectives
The aim of this study was to identify clinical, lesional, and procedural predictors for adverse outcomes of coronary angioplasty and stenting in coronary bypass candidates.
Subjects and Methods
This cohort study included 107 consecutive candidates for coronary artery bypass surgery who underwent percutaneous coronary intervention with multiple coronary stents between Jan 2004 and Dec 2011. The study endpoint was major adverse cardiovascular events (MACEs) including all-cause mortality, nonfatal myocardial infarction, repeat revascularization, and stent thrombosis. Follow up was from the date of index percutaneous coronary intervention to the date of the first MACE, date of death, or December 31, 2015, whichever came first.
Results
In this study (age 62.3±11.2 years, 86% male), 38 patients (36%) had MACE. Among baseline, angiographic, and procedural parameters, there were significant differences in lower left ventricular ejection fraction (LVEF) and worse renal function. In a Cox regression model, LVEF and chronic kidney disease (CKD) were significant predictors for MACE. After a multivariate adjustment, CKD remained a significant predictor of MACEs (hazard ratio: 2.97, 95% confidence interval: 1.50-5.90).
With the development of drug-eluting stents (DES), results of percutaneous coronary intervention (PCI) have improved significantly but remain strongly influenced by the severity and extent of multivessel coronary artery disease (CAD).123) This was clearly demonstrated in the SYNergy between PCI with TAXus and the cardiac surgery (SYNTAX) trial, an “all-comers study” that randomised patients with 3-vessel disease, including those with left main stenosis, to receive PCI with DES or coronary artery bypass graft (CABG).4)5) However, a recent published study of randomized comparison of coronary artery Bypass surgery and Everolimus-eluting Stent implantation in the Treatment of patients with multivessel coronary artery disease (BEST) trial showed better clinical outcomes for multivessel CAD patients treated with a newer generation of DES.6)
Due to the concern that some patients may not be good candidates for CABG because of advanced age or multiple comorbidities-or even because of patients' preferences-some patients with multivessel CAD are treated with PCI. Although several risk-stratification models have been suggested to predict early or long-term cardiovascular events after PCI, little is known about the predictor of adverse outcomes in coronary bypass candidates treated with PCI The objective of the present study was to identify clinical, lesional, and procedural predictors for adverse outcomes after PCI with multiple coronary stents in patients who are candidates for CABG.
In our cohort study between January 2004 and December 2011, 124 multivessel CAD patients who were candidates for CABG but received PCI with multiple coronary stents were enrolled. Making the decision to receive PCI instead of CABG may be either due to a physician's opinion that the patient is not a good candidate or because it is the patient's preference. Patients were excluded if 1) with cardiogenic shock before PCI, 2) had contraindications for dual antiplatelet therapy, 3) had been diagnosed with cancer before they received PCI, or 6) PCI details, or follow-up data were missing (Fig. 1).
Significant coronary lesions that required PCI were defined as those with a stenosis of ≥70% in a segment with a reference diameter of ≥2.0 mm as shown by quantitative coronary angiography. For patients who presented with myocardial infarction with ST elevation, the non-infarct-related lesions were treated by separate interventions within 3 months. All complex lesions, including left main lesions, bifurcation lesions, calcified lesions, long lesions, chronic total occlusion, and ostial lesions of the 3 major coronary arteries had been limited to be treated with DES. Because DES is not covered by Taiwan national insurance, other significant lesions may been treated by bare-metal stents (BMS) according to patient preferences and physician treatment practices. The types of DES implanted were as follows: 1) sirolimus-eluting stents; 2) paclitaxel-eluting stents; 3) everolimus-eluting stents; 4) biolimus A9-eluting stents; and 5) zotarolimus-eluting stents. The choice regarding the use of a specific type of DES was left to the operator's discretion. Sirolimus-eluting and paclitaxel-eluting stents are classified as a first generation DES. Procedural success was defined as a final diameter stenosis of <20% by quantitative coronary angiography (QCA) with normal flow according to the thrombolysis in myocardial infarction (TIMI)-3 criteria. Complete revascularization was defined as successful angiographic results in the major epicardial vessels and their major branches with a reference diameter of ≥2.0 mm, and it had intentionally been done. Follow-up coronary angiography was not routinely performed except for patients with recurrent angina, myocardial ischemia revealed by noninvasive stress tests, or left main CAD.
Data regarding the demographics, clinical, angiographic, and procedural characteristics, and outcomes were collected from the electronic medical records system of the hospital, supplemented by information from patients and their physicians. Chronic kidney disease (CKD) stage ≥3 was defined as an estimated glomerular filtration rate (eGFR) of <60 mL/min/1.73 m2, which was calculated by a 4-variable modification of diet in a Renal Disease study equation.7) The SYNTAX score was calculated to estimate the complexity of the patient's CAD.8) The subjects were divided into 2 groups: those who had major adverse cardiovascular events (MACEs) and those who did not. The primary end-point was the incidence of MACEs during follow-ups, defined as the composite of all-cause mortality, nonfatal myocardial infarction (MI), repeat revascularization, or stent thrombosis. The diagnosis of MI was defined according to the American College of Cardiology criteria.9) Stent thrombosis was defined as definite or probable according to the Academic Research Consortium definitions.10) Subjects were followed up from the date of index PCI to the date of the first MACE, date of death, or December 31, 2015, whichever came first. The study conformed to the principles outlined in the Declaration of Helsinki. The research protocol was approved by the local Institutional Review Board.
Continuous variables were summarized as mean±standard deviation if normally distributed and as a median and interquartile range if non-normally distributed. Continuous variables were compared using Student's t-test. Categorical variables (presented as absolute values and percentages) were compared using the chi-square test (or Fisher's exact test when indicated). The data were collected at baseline and during follow-ups. Significant factors (p<0.05) were included in the Cox regression analysis, which was used to evaluate time-to-event associations with MACEs. Kaplan-Meier curves were plotted, and the log-rank test was used to compare differences between groups. For all analyses, a p<0.05 was considered to be statistically significant. Statistical analysis was performed using the Statistical Package for Social Sciences statistical software, version 19 for Windows (SPSS Inc., Chicago, IL, USA).
Among 107 study patients, 38 patients had experienced MACEs and 69 patients had no MACEs during follow-ups in the present study. The MACE rate was 36%, and the composite MACEs included 9 deaths, 28 repeated revascularizations, and 1 stent thrombosis. Baseline characteristics for patients of the study are shown in Table 1. The mean age was 62.3±11.2 years. No significant differences were found in age, sex, smoking, hypertension, diabetes mellitus, dyslipidemia, old MI, history of CABG, low density cholesterol (LDL-C), total cholesterol, and discharge medications including aspirin, clopidogrel, angiotensin-converting-enzyme inhibitor/angiotensin II receptor blockers, or beta-blockers between the event and no event groups. There were significant differences in left ventricular ejection fraction (LVEF), serum creatinine, and eGFR. Patients who experienced MACE had a lower LVEF (53.8±15.4% vs. 59.6±13.1%, p=0.049) and worse renal function (serum creatinine: 2.2±2.8 vs. 1.2±1.3 mg/dL, p=0.016; eGFR: 62.7±32.3 vs. 76.0±24.6 mL/min/1.73 m2, p=0.019) than did patients without MACEs.
Table 2 shows the QCA and PCI data. We compared angiographic lesion characteristics, including bifurcation lesions, chronic total occlusions, ostial lesions, left main artery involvement, SYNTAX score, and number of vessels showing CAD between patients with and without MACEs. The procedural details including number, length, diameter, and type of stent (DES or BMS) were also analyzed. All of these angiographic and procedural characteristics did not differ significantly between patients with and without MACEs.
In a Cox regression analysis, LVEF and CKD stage ≥3 were significant predictors for MACEs. After an adjustment, only CKD stage ≥3 remained an independent predictor of MACEs (HR: 2.97, 95% CI: 1.50-5.90) (Table 3). Kaplan-Meier curves were plotted and showed a higher MACE rate in patients with CKD than without CKD (Fig. 2).
The current study shows that in patients with multivessel CAD treated with coronary stenting, CKD stage ≥3 was the independent prognostic predictor for MACE.
Although coronary revascularization is an effective strategy to reduce cardiac mortality and improve outcomes compared to medical treatment for CKD patients with CAD,11)12) the Arterial Revascularization Therapies Study noted poor outcomes among patients with CKD and multivessel CAD treated with CABG or PCI.13) Previous studies showed that patients with CKD may have higher levels of oxidative stress, systemic inflammation, or endothelial dysfunction. These pathophysiological features can contribute to accelerated atherosclerosis and probably lead to a higher rate of MACEs.14151617) We confirmed the findings of previous studies that CKD significantly increased the risk of adverse events after coronary revascularization,13) and Left ventricular dysfunction is a predictor of adverse outcomes after PCI.18) In our study, LVEF was also significantly prognostic in a univariate analysis but was not significant after adjustment. A possible explanation is that most of our study patients had a normal or mildly impaired LVEF (57.4±15.1%), which may have attenuated the prognostic power of LVEF in our analysis.
DES has been shown to be superior to BMS in reducing the rate of coronary restenosis and repeated target vessel revascularization, even for patients with CKD.19) In our study patients, some of them had been treated with a hybrid of DES and BMS implantation. However, no differences between these 2 types of stents were found in this study. Patients with and without adverse events received an equal number of DES and BMS. The total length of BMS did not differ significantly between groups. The possible explanation is that BMS had not been implanted in the complex lesional sites which may affect outcomes according to our treatment strategy.
In the present study, after comparison with other factors, we found that CKD was the strongest predictor of adverse outcomes for patients treated with coronary stenting. Our findings may have important implications. First, according to the results of SYNTAX trial, CABG has been recommended as the preferred revascularization strategy, particularly in patients with complex coronary lesions.4) However, the recent published study of a BEST trial showed showing better clinical outcomes for multivessel CAD patients treated with newer generation of DES.6) There might be more multivessel CAD patients without excessive operative risk treated with coronary stenting in the future. Therefore, to identify the prognostic predictors for multivessel CAD patients treated with coronary stents is important. Second, the majority of randomized trials including both SYNTAX and BEST trials had been excluding patients with progressive renal dysfunction. Our data had offered a realistic view of what is observed in the clinic, especially for the CKD patients.
The strengths of this study include the comprehensive data of clinical, lesional, and procedural characteristics, and approximately 98% of outcome ascertainment. The high follow-up rate may be due to patients with severe CAD who were candidates for CABG, undergoing clinical follow-ups in quick succession, which might have influenced physicians' attention, and patients' compliance. There are some limitations to the present study. First, apart from the intrinsic limitations associated with a retrospective and single-center study, the small sample size may had some influences for the analysis. For example, the predictive value of traditional factors for adverse outcomes such as diabetes mellitus, LVEF, SYNTAX score, and BMS stent was not observed. Only CKD was significantly prognostic in the analysis. In other words, CKD may be the strongest prognostic predictor for multivessel CAD patients treated with coronary stents. Second, the study period spans 8 years. Therefore, the bias of advances in medical practice may also affect our analysis. For example, the utilization of intravascular ultrasound examination, rotational atherectomy, and intervention techniques had changed over time. Third, we did not perform a routine angiographic follow-up and the retrospectively observational nature of our study; we did not have sufficient follow-up parameters in QCA that perhaps could have identified other lesional characteristics as independent variables in the model and may have supported the inclusion of other end points.
In conclusion, CKD seems to be the strongest prognosticator for coronary bypass candidates who were treated with coronary angioplasty and stenting. Additional prospective, randomized, and even functional flow reserve-based interventions for patients with complex CAD lesions should evaluate this hypothesis.
Figures and Tables
Fig. 1
Flow chart of enrollment. CAD: coronary artery disease, CABG: coronary artery bypass graft, PCI: percutaneous coronary intervention.

Fig. 2
Kaplan-Meier analysis for event-free survival in patients with or without CKD. CKD: chronic kidney disease.

Table 1
Baseline characteristics
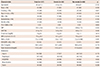
Values are presented as mean±standard deviation or number (%). DM: diabetes mellitus, MI: myocardial infarction, CABG: coronary artery bypass graft, SBP: systolic blood pressure, LVEF: left ventricular ejection fraction, GFR: glomerular filtration rate, HbA1c: hemoglobin A1c, CKD: chronic kidney disease, LDL-C: low-density lipoprotein cholesterol, ACEI: angiotensin-converting enzyme inhibitor, ARB: angiotensin receptor blocker
Table 2
Angiographic and procedural characteristics
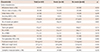
Table 3
Cox-regression hazard ratio in univariate and multivariate analyses to predict major adverse cardiovascular events for 2 years

References
1. Onuma Y, Wykrzykowska JJ, Garg S, et al. 5-Year follow-up of coronary revascularization in diabetic patients with multivessel coronary artery di sease: i nsights from ARTS (arterial revascularization therapy study)-II and ARTS-I trials. JACC Cardiovasc Interv. 2011; 4:317–323.
2. Serruys PW, Onuma Y, Garg S, et al. 5-Year clinical outcomes of the ARTS II (Arterial Revascularization Therapies Study II) of the sirolimus-eluting stent in the treatment of patients with multivessel de novo coronary artery lesions. J Am Coll Cardiol. 2010; 55:1093–1101.
3. Serruys PW, Ong AT, Morice MC, et al. Arterial revascularisation therapies study part ii-sirolimus-eluting stents for the treatment of patients with multivessel de novo coronary artery lesions. EuroIntervention. 2005; 1:147–156.
4. Mohr FW, Morice MC, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013; 381:629–638.
5. Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009; 360:961–972.
6. Park SJ, Ahn JM, Kim YH, et al. Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med. 2015; 372:1204–1212.
7. Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006; 145:247–254.
8. Sianos G, Morel MA, Kappetein AP, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005; 1:219–227.
9. Cannon CP, Battler A, Brindis RG, et al. American college of cardiology key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes. a report of the american college of cardiology task force on clinical data standards (Acute coronary syndromes writing committee). J Am Coll Cardiol. 2001; 38:2114–2130.
10. Mauri L, Hsieh WH, Massaro JM, Ho KK, D'Agostino R, Cutlip DE. Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med. 2007; 356:1020–1029.
11. Reddan DN, Szczech LA, Tuttle RH, et al. Chronic kidney disease, mortality, and treatment strategies among patients with clinically significant coronary artery disease. J Am Soc Nephrol. 2003; 14:2373–2380.
12. Hemmelgarn BR, Southern D, Culleton BF, et al. Survival after coronary revascularization among patients with kidney disease. Circulation. 2004; 110:1890–1895.
13. Ix JH, Mercado N, Shlipak MG, et al. Association of chronic kidney disease with clinical outcomes after coronary revascularization: the Arterial Revascularization Therapies Study (ARTS). Am Heart J. 2005; 149:512–519.
14. Panichi V, Migliori M, De Pietro S, et al. C reactive protein in patients with chronic renal diseases. Ren Fail. 2001; 23:551–562.
15. Sarnak MJ, Coronado BE, Greene T, et al. Cardiovascular disease risk factors in chronic renal insufficiency. Clin Nephrol. 2002; 57:327–335.
16. Navab KD, Elboudwarej O, Gharif M, et al. Chronic inflammatory disorders and accelerated atherosclerosis: chronic kidney disease. Curr Pharm Des. 2011; 17:17–20.
17. Polonsky TS, Bakris GL. Chronic kidney disease: a coronary heart disease equivalent? Lancet. 2012; 380:783–785.
18. Holper EM, Blair J, Selzer F, et al. The impact of ejection fraction on outcomes after percutaneous coronary intervention in patients with congestive heart failure: an analysis of the national heart, lung, and blood institute percutaneous transluminal coronary angioplasty registry and dynamic registry. Am Heart J. 2006; 151:69–75.
19. Tomai F, Ribichini F, De Luca L, et al. Randomized comparison of xience v and multi-link vision coronary stents in the same multivessel patient with chronic kidney disease (Renal-Des) study. Circulation. 2014; 129:1104–1112.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download