1. Ben-Chetrit E, Levy M. Familial Mediterranean fever. Lancet. 1998; 351:659–664. PMID:
9500348.
2. Stoffman N, Magal N, Shohat T, et al. Higher than expected carrier rates for familial Mediterranean fever in various Jewish ethnic groups. Eur J Hum Genet. 2000; 8:307–310. PMID:
10854115.
3. Touitou I. The spectrum of familial Mediterranean fever (FMF) mutations. Eur J Hum Genet. 2001; 9:473–483. PMID:
11464238.
4. Turesson C, Jarenros A, Jacobsson L. Increased incidence of cardiovascular disease in patients with rheumatoid arthritis: results from a community based study. Ann Rheum Dis. 2004; 63:952–955. PMID:
15051620.
5. Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006; 27:2588–2605. PMID:
17000623.
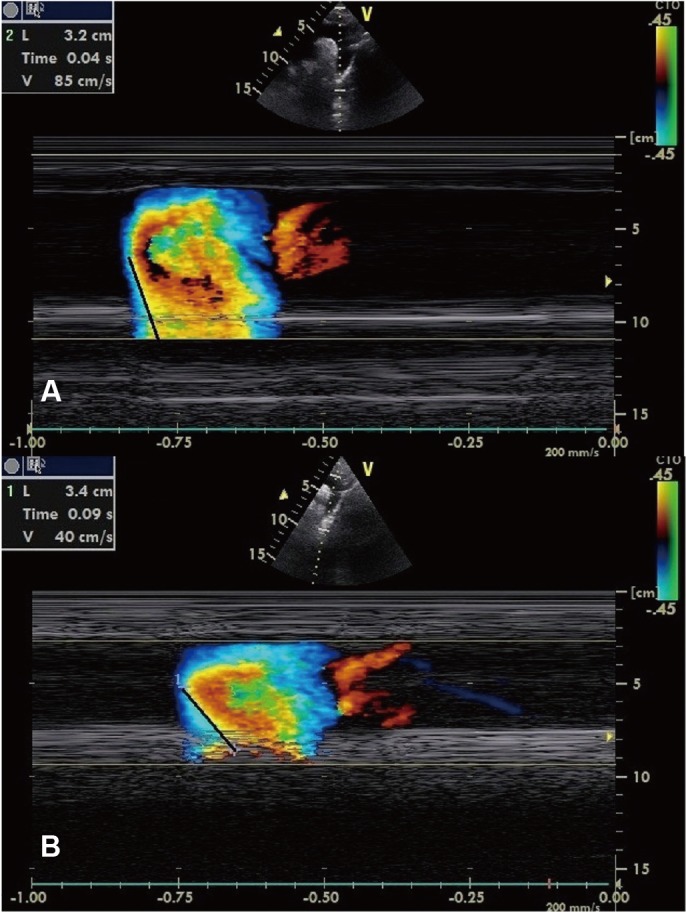
6. Simsek H, Sahin M, Gunes Y, Dogan A, Gumrukcuoglu HA, Tuncer M. A novel echocardiographic method for the detection of subclinical atherosclerosis in newly diagnosed, untreated type 2 diabetes. Echocardiography. 2013; 30:644–648. PMID:
23347332.
7. Sen T, Tufekcioglu O, Ozdemir M, et al. New echocardiographic parameter of aortic stiffness and atherosclerosis in patients with coronary artery disease: aortic propagation velocity. J Cardiol. 2013; 62:236–240. PMID:
23778004.
8. Livneh A, Langevitz P, Zemer D, et al. Criteria for the diagnosis of familial Mediterranean fever. Arthritis Rheum. 1997; 40:1879–1885. PMID:
9336425.
9. Akcay A, Acar G, Sayarlioglu M, et al. QT dispersion and transmural dispersion of repolarization in patients with familial Mediterranean fever. Mod Rheumatol. 2009; 19:550–555. PMID:
19578931.
10. Kaya EB, Yorgun H, Akdogan A, et al. Heart-rate recovery index is impaired in Behçet's disease. Tex Heart Inst J. 2009; 36:282–286. PMID:
19693299.
11. Rozenbaum M, Naschitz JE, Yudashkin M, et al. Cardiovascular autonomic dysfunction in familial Mediterranean fever. J Rheumatol. 2002; 29:987–989. PMID:
12022362.
12. Levy M, Ehrenfeld M, Levo Y, Fischel R, Zlotnick A, Eliakim M. Circulating immune complex in recurrent polyserositis. (Familial mediterranean fever periodic disease). J Rheumatol. 1980; 7:886–890. PMID:
7205826.
13. Roman MJ, Shanker BA, Davis A, et al. Prevalence and correlates of accelerated atherosclerosis in systemic lupus erythematosus. N Engl J Med. 2003; 349:2399–2406. PMID:
14681505.
14. Thenappan T, Ali Raza J, Movahed A. Aortic atheromas: current concepts and controversies-a review of the literature. Echocardiography. 2008; 25:198–207. PMID:
18269565.
15. Caliskan M, Gullu H, Yilmaz S, et al. Impaired coronary microvascular function in familial Mediterranean fever. Atherosclerosis. 2007; 195:e161–e167. PMID:
17673217.
16. Celermajer DS, Sorensen KE, Bull C, Robinson J, Deanfield JE. Endothelium-dependent dilatation in the systemic arteries of asymptomatic subjects relates to coronary risk factors and their interaction. J Am Coll Cardiol. 1994; 24:1468–1474. PMID:
7930277.
17. Demiralp E, Kardesoglu E, Kiralp MZ, et al. Aortic elasticity in patients with ankylosing spondylitis. Acta Cardiol. 2004; 59:630–634. PMID:
15636447.
18. Bicer A, Acikel S, Kilic H, et al. Impaired aortic elasticity in patients with psoriasis. Acta Cardiol. 2009; 64:597–602. PMID:
20058504.
19. Wright CI, Brouwer-de Cock KA, Kroner CI, Hoeks AP, Draijer R. The relation of arterial stiffness to endothelial function in healthy subjects. Physiol Meas. 2007; 28:573–582. PMID:
17470989.
20. Duprez DA, Cohn JN. Arterial stiffness as a risk factor for coronary atherosclerosis. Curr Atheroscler Rep. 2007; 9:139–144. PMID:
17877923.
21. Fazio GP, Redberg RF, Winslow T, Schiller NB. Transesophageal echocardiographically detected atherosclerotic aortic plaque is a marker for coronary artery disease. J Am Coll Cardiol. 1993; 21:144–150. PMID:
8417055.
22. Güneş A, Güntekin Ü, Yıldız S, et al. Association of aortic flow propagation velocity with ankle-brachial blood pressure index in patients with hypertension: an observational study. Anadolu Kardiyol Derg. 2012; 12:568–573. PMID:
22877895.
23. Güneş Y, Tuncer M, Yildirim M, Güntekin U, Gümrükçüoğlu HA, Şahin M. A novel echocardiographic method for the prediction of coronary artery disease. Med Sci Monit. 2008; 14:MT42–MT46. PMID:
18758427.
24. Yiu KH, Yeung CK, Chan HT, et al. Increased arterial stiffness in patients with psoriasis is associated with active systemic inflammation. Br J Dermatol. 2011; 164:514–520. PMID:
21039409.
25. Mäki-Petäjä KM, Hall FC, Booth AD, et al. Rheumatoid arthritis is associated with increased aortic pulse-wave velocity, which is reduced by anti-tumor necrosis factor-alpha therapy. Circulation. 2006; 114:1185–1192. PMID:
16952987.
26. Yildiz M, Masatlioglu S, Seymen P, Aytac E, Sahin B, Seymen HO. The carotid-femoral (aortic) pulse wave velocity as a marker of arterial stiffness in familial Mediterranean fever. Can J Cardiol. 2006; 22:1127–1131. PMID:
17102830.
27. Berkun Y, Padeh S, Reichman B, et al. A single testing of serum amyloid a levels as a tool for diagnosis and treatment dilemmas in familial Mediterranean fever. Semin Arthritis Rheum. 2007; 37:182–188. PMID:
17512038.
28. Yildirim K, Uzkeser H, Keles M, et al. Relationship between serum interleukin-1beta levels and acute phase response proteins in patients with familial Mediterranean fever. Biochemia Med (Zagreb). 2012; 22:109–113.
29. Ossareh S, Alaei A, Saedi D. Carotid intima-media thickness in maintenance hemodialysis patients: role of cardiovascular risk factor. Iran J Kidney Dis. 2011; 5:169–174. PMID:
21525576.
30. Ugurlu S, Seyahi E, Cetinkaya F, Ozbakir F, Balci H, Ozdogan H. Intima-media thickening in patients with familial Mediterranean fever. Rheumatology (Oxford). 2009; 48:911–915. PMID:
19478036.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download