Abstract
Background and Objectives
The earliest atrial (A)/ventricular (V) activation potential, or accessory pathway (AP) potential are commonly used as ablation targets for atrioventricular (AV) APs. However, these targets are sometimes ambiguous.
Subjects and Methods
We reviewed 119 catheter ablation cases in 112 patients diagnosed with orthodromic atrioventricular reentrant tachycardia (AVRT) or Wolff-Parkinson-White (WPW) syndrome. Local A/V amplitude potentials with the earliest activation or AP potential were measured shortly before achieving antegrade AP conduction block, ventriculoatrial block during right ventricle (RV) pacing, or AVRT termination with no AP conduction.
Results
APs were located in the left lateral (55.5%), left posterior (17.6%), left posteroseptal (10.1%), midseptal (1.7%), right posteroseptal (7.6%), right posterior (1.7%), and right lateral (5.9%) regions. The mean earliest activation time was 16.7±15.5 ms, mean A/V potential was 1.1±0.9/1.0±0.9 mV, and mean A/V ratio was 1.7±2.0. There was no statistically significant difference between the activation methods (antegrade vs. RV pacing vs. orthodromic AVRT) or AP locations (left vs. right atrium). However, when the local A/V ratio was divided into 3 groups (≤0.6, 1.0±0.3, and ≥1.4), the antegrade approach resulted in an A/V ratio greater than 1.0±0.3 (86.7%, p=0.007), and the orthodromic AVRT state resulted in a ratio of less than 1.0±0.3 (87.5%, p<0.001).
Atrioventricular (AV) accessory pathways (APs) mostly exist along the AV annulus, and atrioventricular reentrant tachycardia (AVRT) using these APs is a common form of paroxysmal supraventricular tachycardia (PSVT).1)2)3)4)5) Catheter ablation is currently the first-line therapy for symptomatic patients with AP-mediated tachycardia, and success rates are dependent on accurate localization of the APs.6)7) The commonly used methods for localization of the APs are targeting the earliest atrial (A) or ventricular (V) activation potentials, AP potentials, or retrograde A activation with the shortest ventriculoatrial (VA) interval.1)8)9) However, these methods are sometimes ambiguous because of signal noise or compound potentials, especially after several improper ablations.1) In some cases, catheter-induced mechanical trauma could mask all of the AP potentials.10) In addition, an A insertion point is different from the point of a V attachment by an oblique course of the AV APs to the AV groove, which makes it difficult to identify proper ablation sites: A, V side or in the middle of the AV groove.8)11)12)
The local A/V amplitude ratio has been used as a reference for guiding AV APs. Current criteria recommend an A electrogram amplitude of greater than 0.4 mV or an A/V amplitude ratio of 0.1 or greater during anterograde activation mapping, and the A≥V electrogram during ablation from the A aspect of the annulus.9) However, these recommendations are somewhat broad, and previous studies on the A/V ratio in ablation guidance are limited.13) Haissaguerre et al.14) conducted an overall comparison of electrograms at successful vs. unsuccessful sites and found no difference in the A/V ratio for manifest APs; nor did the A/V ratio influence the ablation results due to different A/V ratios based on the location of the APs.15) Additionally, a tachycardia state or pacing maneuver could influence the local A/V amplitude potentials. Thus, we analyzed the local A/V ratio using different activation methods or in various AP locations, and aimed to identify the optimal A/V ratio as an adjuvant marker for localization of the AV APs.
From January 2011 to March 2015, we reviewed 148 catheter ablation cases in 141 patients diagnosed with orthodromic AVRT or Wolf-Parkinson-White (WPW) syndrome. The study included a total of 119 cases in 112 patients. We excluded 29 cases due to poor recording (12 cases), patients being less than 18 years of age (6 cases), compound mixed multiple APs (6 cases), ablation during sinus rhythm for concealed APs (3 cases), and ablation failure (2 cases). Each patient who underwent electrophysiologic study (EPS) and catheter ablation provided written informed consent for the procedure, and the study protocol was reviewed and approved by the Institutional Review Board of Inje University.
All antiarrhythmic drugs were discontinued for at least five half-lives before the EPS and catheter ablation. All procedures were performed under the fasting, not-sedated state. After both femoral veins were cannulated percutaneously, two 6-French quadripolar catheters were inserted in the right ventricle (RV) apex and the His bundle region sequentially. A 7-French duo-decapolar catheter with 2-8-2 mm electrode spacing was placed in the coronary sinus (CS)/right atrium (RA) regions. Surface electrograms and intracardiac bipolar electrograms (filtered between 30 and 500 Hz) were simultaneously displayed and recorded on a digital electrophysiological recording system (CardioLab, Prucka Eng., Houston, TX, USA). A programmed stimulation protocol, including S1S2 and incremental stimulations, was respectively performed in the RV apex and the high RA to induce tachyarrhythmias until the effective refractory periods of the atrium and ventricle were achieved. If supraventricular tachycardia was not induced, programmed stimulations were repeated under intravenous infusion of isoproterenol (1 to 5 microgram/minute) to facilitate the induction of arrhythmias.
The ablation catheter was inserted via the right femoral vein and positioned in the tricuspid annulus for ablation of the right-sided AV APs, or in the mitral annulus via trans-septal puncture for the left-sided AV APs. All cases were performed using a long sheath (SR-0 for right sided APs and SL-1 for left sided APs, St. Jude Medical, St. Paul, MN) for better stability and good contact for mapping and ablation. Bipolar recordings on the ablation catheter were used for mapping and ablation, and ablation criteria for locating the target site of the AV APs were the site of the earliest V activation relative to the onset of the delta wave or AP potential during sinus rhythm for manifest APs, and the site of the earliest A activation or AP potential during orthodromic AVRT or RV pacing for concealed APs. For any ablation target, a similar local electrogram from the ablation catheter was maintained for at least 3 cycles to confirm electrical potentials and catheter stability. The most stable local A/V amplitude potentials with the earliest activation or AP potential were measured from the nadir to the peak at the ablation catheter shortly before achieving an antegrade AP conduction block, or VA block during RV pacing, or AVRT termination with no AP conduction (Fig. 1). For some cases with merged A and V potential, A or V extrastimuli were delivered to clearly reveal the activation component.13) A 4 mm non-irrigated deflectable ablation catheter (Biosense Webster, Diamond Bar, CA, USA) was used for the catheter ablation. In some refractory cases, a 3.5 mm irrigated deflectable ablation catheter (Thermocool®, Biosense Webster) was used. A radiofrequency (RF) application was set with target temperatures of 60℃ and maximum power outputs of 35-40 W for the non-irrigated catheter and 45℃ and 35 W for the irrigated catheter, respectively. If there were no signs of successful ablation within 15 seconds, RF energy was discontinued and another point for good potential was sought. When the delta wave was abolished or VA block was achieved, the energy was continued for 60-90 seconds. Successful ablation was defined as the elimination of antegrade/retrograde AP conduction and lack of induction of AVRT using these APs. After successful ablation, patients were observed for at least 30 minutes, and programmed electrical stimulation with or without isoproterenol infusion was repeated to induce supraventricular tachycardia prior to completing the procedure.
After ablation, patients underwent regular follow-ups at 3 to 6-month intervals without antiarrhythmic medications. Long-term efficacy was assessed on the basis of clinical symptoms, resting surface electrocardiograms and 24-hour Holter recording. An electrocardiogram was recorded whenever the patient experienced palpitations or previous arrhythmia-related symptoms.
Continuous variables were expressed as mean±standard deviation. Data were compared using the student's t-test or one-way ANOVA. Categorical variables, expressed as numbers and percentages, were compared using Chi-square or Fisher's exact test. For post hoc analysis, the Bonferroni correction was applied to adjust for multiple comparisons. All tests of significance were two-tailed, and a p value less than 0.05 was considered significant. All statistical analyses were performed using SPSS for Windows, version 17.0 (SPSS Inc., Chicago, IL, USA).
Baseline clinical characteristics of the study population are listed in Table 1. The mean age was 41.9±15.8 years, and most of the patients were male (69.6%). A WPW pattern was observed in 41 cases (36.6%) and the remaining cases were orthodromic AVRT using concealed APs. Two-dimensional echocardiography showed no anatomic or functional abnormalities, with the exception of one case of Ebstein's anomaly. The mean left ventricular ejection fraction was 62.4±5.0%, and the mean left atrial diameter was 33.9±4.3 mm. No complications occurred during the procedure in any of the cases. The mean follow-up period was 21.5±14.0 months, and four cases (3.3%) of orthodromic AVRT (left lateral [1], left posterior [2], and left posteroseptal AP [1]) recurred. Three cases had been ablated during RV pacing, and one case during an orthodromic AVRT state. Two cases were successfully re-ablated, and 2 cases refused additional EPS.
The locations of the APs are described in Table 2. The most common AP location was the left lateral site (55.5%). The other AP locations were left posterior (17.6%), left posteroseptal (10.1%), right posteroseptal (7.6%), right lateral (5.9%), right posterior (1.7%), and midseptal (1.7%) sites. The AV APs were ablated using an antegrade approach referenced from the delta wave (15 cases, 12.6%), under the RV pacing (72 cases, 60.5%), and under the orthodromic AVRT state (32 cases, 26.9%).
The mean values of the electrical potentials are presented in Table 3. The mean earliest activation or AP potential was 16.7±15.5 ms (interquartile range, 7.0-20.0), which was measured from the delta wave for an antegrade approach or from the earliest A or AP potential of the local CS electrode during RV pacing or orthodromic AVRT state. The mean A and V potentials were 1.1±0.9 mV (interquartile range, 0.5-1.4) and 1.0±0.9 mV (interquartile range, 0.5-1.3), respectively. The mean A/V ratio was 1.7±2.0 (interquartile range, 0.5-2.0). Distributions of the A and V amplitude potentials are depicted in Fig. 2. When these values were compared based on the activation methods (antegrade vs. RV pacing vs. orthodromic AVRT), or the location of the APs (left vs. right atrium), there was no statistically significant difference.
However, when the local A/V ratio was divided into 3 groups (≤0.6, 1.0±0.3, and ≥1.4), the antegrade approach and orthodromic AVRT state showed a statistically significant difference, but post-hoc analysis by Bonferroni correction did not show a significant difference among the groups. For the antegrade approach, the ≥1.0±0.3 groups were statistically different from the less than 0.6 group (86.7% vs. 13.3%, p=0.007), and for the orthodromic AVRT state, the ≤1.0±0.3 groups were statistically different from the more than 1.4 group (87.5% vs. 12.5%, p<0.001). RV pacing or the location of the APs, which was divided by left/right side or subdivided by each AP location, showed no difference in the distribution of the local A/V ratio (Table 4).
The main findings of this study were as follows: 1) The mean local A and V potential were about 1.0 mV, and the mean A/V ratio was over 1.0. However, these values did not differ significantly based on activation methods (antegrade vs. RV pacing vs. orthodromic AVRT) or AP locations (left vs. right atrium). 2) When the local A/V ratio was divided into 3 groups (≤0.6, 1.0±0.3, and ≥1.4), the antegrade approach resulted in an A/V ratio greater than 1.0±0.3, and the orthodromic AVRT state resulted in a ratio of less than 1.0±0.3). 3) The A/V ratio differed based on the activation method, which could be a good adjuvant marker for targeting AV APs.
The conventional method for ablation of AV APs involves placing several multi-electrode catheters and an ablation catheter in different interest regions and ablating to target the earliest local activation. Newly adopted electroanatomic 3-dimensional (D) mapping systems, magnetic navigation and specialized multielectrode catheters, such as circular or multispline catheters facilitate the localization and ablation of arrhythmic foci with more precision.6)7) However, these techniques require increased financial costs, additional training, support, and procedure preparation time. Additionally, several studies have demonstrated that the ablation success rate when using the 3-D electroanatomic mapping system for PSVT is comparable to conventional approaches, even though using the 3-D mapping system showed significant reduction in fluoroscopy time.7) When considering these factors, the conventional approach is still the prime method for PSVT ablation.
For targeting AV APs, the methods using the earliest A or V activation potentials, AP potentials, or retrograde A activation with the shortest VA interval are time-oriented AP searching methods. On the contrary, methods using the local A/V amplitude potential or A/V ratio are location-oriented methods.1)8)9) However, the usefulness of the local A/V amplitude potential or A/V ratio is limited. At the beginning of RFCA, the local A/V ratio is variable (0.05-6), and deemed as unimportant for localization of the AV APs.13) In a comparison study of electrograms at successful vs. unsuccessful sites, Haissaguerre et al.14) found that there was no difference in the local A/V ratio (1.3±1.5 vs 1.2±1.6) in patients with manifest AP, and the local A/V ratio did not influence ablation results owing to different A/V ratios depending on the location of the APs.15) Later, Cappato et al.16) demonstrated that an A/V ratio of ≥0.1 was observed significantly more often in successful, compared to unsuccessful pulses for the manifest left free-wall AP patients (47 of 49 vs. 32 of 52; p<0.001). They also suggested recording of a presumed AP potential, A/V ratio of at least 0.10, an A-V interval of no more than 40 ms, and delta V interval of no more than 0 ms were successful ablation markers of V insertion of the AP of manifest left free-wall AP patients. In cases where a delta V interval was greater than 10 ms, an A/V ratio of more than 0.33 could be helpful for ablation of the AP at the A insertion.16) These result suggest that rather than using the local A/V ratio as a sole marker, it should be combined with the different markers for successful ablation for manifest left free-wall APs. With the current criteria, the recommendation is for an A electrogram amplitude of greater than 0.4 mV, or an A/V amplitude ratio of at least 0.1 during anterograde activation mapping, and an A≥V electrogram during ablation from the A aspect of the annulus.9) However, these recommendations are somewhat broad. For example, among all of the cases in the current study, including those with concealed retrograde activation, the range of the local A/V amplitude was 0.1-6.7 mV/0.1-5.2 mV, respectively, and the A/V ratio was 0.1-13.4. All data are compatible with the current criteria, which paradoxically suggest that these current criteria need to be more specific.
The local A/V ratio could be used for judging the catheter position whether it is close to the A or V side. Guo et al.13) suggested that a local A/V ratio of 1:1 is empirically defined as amenable to RF ablation for right AP targets in patients with a normal heart structure. Although a local A/V ratio close to 1 would probably be optimal, the stable position of the catheter was very dependent on the AP location, so that it could be on the A or V side of the annulus.15) In our cases, the antegrade approach showed an A/V ratio greater than 1.0±0.3 (86.7%, p=0.007), and the orthodromic AVRT state produced a ratio of less than 1.0±0.3 (87.5%, p<0.001). On the contrary, the RV pacing state showed no difference in the distribution of the local A/V ratio. Some factors could affect these results, such as catheter stability or, depending on heart rate, the A/V electrical characteristics. During sinus rhythm or the stable pacing state, the ablation catheter could be positioned more stably and, ideally, at the A/V ratio close to 1:1 on the AV groove. On the contrary, during a fast heart rate such as AVRT, stabilization of the catheter is relatively difficult and pointing to the V side might be more stable considering sequential V to A contraction. Further experimental studies are required to verify this. Additionally, we could not find any difference in the local A/V ratio based on the left/right A location or subdivided by each AP location, which suggests that the local A/V ratio could be applied anywhere along the AV groove when searching for the AV APs.
Although using these conventional searching methods for AV APs, some cases are resistant to ablation due to their relationship to an epicardial course, a wide AP insertion, or an embedded pathway in an adverse location relative to the AV groove.16) Mont et al.17) suggested that a large local A/V ratio and the occurrence of early conduction block in the AP are the best predictors of successful RFCA using a single catheter approach for left-sided APs. Long et al.18) addressed the importance of mapping on the A side when ablating an A insertion away from the AP mitral annulus. In such cases, searching for the bigger A/V ratio site could be a good option, but this was not tested in this study.
This study had some limitations. It was a non-randomized, retrospective study, and the sample was relatively small. However, included cases were ablated by targeting the earliest A/V activation potential or AP potential, and were not intended for measuring the A/V ratio. Additionally, our measured values were in accord with data reported by previous studies. Thus, the inclusion of these cases increased the likelihood of objectively measuring the local A/V ratio. Further, we did not confirm exact AP locations using a 3D electroanatomic mapping system. This means that the electrically and fluoroscopically-guided A or V positons for the AP could be different from the actual A or V positon. Although the local A/V ratio has been used since the beginning of RFCA, the usefulness and application of the ratio is limited due to its vaguely defined characteristics. The results of different A/V ratios based on activation methods could be useful markers for RFCA of AV APs in different clinical situations.
The mean local A/V potential and ratio did not differ significantly based on activation method (antegrade vs. RV pacing vs. orthodromic AVRT) or AP location (left vs. right atrium). However, different A/V ratios based on activation methods (≥1.0±0.3 in the antegrade approach and ≤1.0±0.3 in the orthodromic AVRT state) could be good adjuvant markers for targeting AV APs. A randomized, large-scale, prospective multicenter trial is needed to confirm these outcomes.
References
1. Chen SA, Tai CT. Ablation of atrioventricular accessory pathways: current technique-state of the art. Pacing Clin Electrophysiol. 2001; 24:1795–1809. PMID: 11817815.
2. Liu E, Shehata M, Swerdlow C, et al. Approach to the difficult septal atrioventricular accessory pathway: the importance of regional anatomy. Circ Arrhythm Electrophysiol. 2012; 5:e63–e66. PMID: 22715241.
3. Wang L, Yao R. Radiofrequency catheter ablation of accessory pathway-mediated tachycardia is a safe and effective long-term therapy. Arch Med Res. 2003; 34:394–398. PMID: 14602506.
4. Dagres N, Clague JR, Kottkamp H, Hindricks G, Breithardt G, Borggrefe M. Radiofrequency catheter ablation of accessory pathways. Outcome and use of antiarrhythmic drugs during follow-up. Eur Heart J. 1999; 20:1826–1832. PMID: 10581141.
5. Scheinman M, Calkins H, Gillette P, et al. NASPE policy statement on catheter ablation: personnel, policy, procedures, and therapeutic recommendations. Pacing Clin Electrophysiol. 2003; 26:789–799. PMID: 12698688.
6. Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. Heart Rhythm. 2016; 13:e92–135. PMID: 26409097.
7. Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. Heart Rhythm. 2016; 13:e136–e221. PMID: 26409100.
8. Iturralde P, Guevara-Valdivia M, Rodríguez-Chávez L, Medeiros A, Colin L. Radiofrequency ablation of multiple accessory pathways. Europace. 2002; 4:273–280. PMID: 12134973.
9. Issa ZF, Miller JM, Zipes DP. Atrioventricular reentrant tachycardia. In : Issa ZF, Miller JM, Zipes DP, editors. Clinical arrhythmology and electrophysiology: a companion to braunwald's heart disease. 2nd ed. Philadelphia: Elsevier Sanders;2012. p. 411–467.
10. Han S, Miller JM. Pacemap of delta wave for successful ablation of traumatized atrioventricular accessory pathway. Heart Rhythm. 2012; 9:1321–1323. PMID: 22406146.
11. Otomo K, Gonzalez MD, Beckman KJ, et al. Reversing the direction of paced ventricular and atrial wavefronts reveals an oblique course in accessory AV pathways and improves localization for catheter ablation. Circulation. 2001; 104:550–556. PMID: 11479252.
12. Morady F. Catheter ablation of supraventricular arrhythmias: state of the art. J Cardiovasc Electrophysiol. 2004; 15:124–139. PMID: 15028093.
13. Guo XG, Liu XU, Zhou GB, Ma J, Ouyang F, Zhang S. Frequency of fractionated ventricular activation and atrial/ventricular electrogram amplitude ratio at successful ablation target of accessory pathways in patients with Ebstein's anomaly. J Cardiovasc Electrophysiol. 2015; 26:404–411. PMID: 25546726.
14. Haissaguerre M, Fischer B, Warin JF, Dartigues JF, Lemétayer P, Egloff P. Electrogram patterns predictive of successful radiofrequency catheter ablation of accessory pathways. Pacing Clin Electrophysiol. 1992; 15(11 Pt 2):2138–2145. PMID: 1279615.
15. Haïssaguerre M, Dartigues JF, Warin JF, Le Metayer P, Montserrat P, Salamon R. Electrogram patterns predictive of successful catheter ablation of accessory pathways. Value of unipolar recording mode. Circulation. 1991; 84:188–202. PMID: 2060095.
16. Cappato R, Schlüter M, Mont L, Kuck KH. Anatomic, electrical, and mechanical factors affecting bipolar endocardial electrograms. Impact on catheter ablation of manifest left free-wall accessory pathways. Circulation. 1994; 90:884–894. PMID: 8044960.
17. Mont L, Schlüter M, Gürsoy S, Siebels J, Kuck KH. The predictors of success in the radiofrequency ablation of left accessory pathways using the single-catheter technic. Rev Esp Cardiol. 1993; 46:745–751. PMID: 8290777.
18. Long DY, Dong JZ, Sang CH, et al. Ablation of left-sided accessory pathways with atrial insertion away from the mitral annulus using an electroanatomical mapping system. J Cardiovasc Electrophysiol. 2013; 24:788–792. PMID: 23581615.
Fig. 1
The measurement of local A/V ratio for orthodromic atrioventricular reentrant tachycardia using a concealed left lateral AP. (A) AP potential was recorded simultaneously at the ablation catheter and the local CS (1, 2) electrode. Shortly before achieving ventriculoatrial block during right ventricular pacing, the most stable local A/V amplitude potentials with the earliest activation or AP potential were measured at the ablation catheter, for which the values were 1.0/1.2 mV, respectively, and the A/V ratio was 0.8. From top to bottom: surface leads II, aVF, V1, HRA (1: distal, 3: proximal side), CS (1, 2: distal, 9, 10: proximal), RVa d, ABL (D, P). (B) The ablation catheter position during ablation targeting the AP in left anterior oblique view (30 degree) and (C) right anterior oblique view (30 degree). A/V: atrial/ventricular, AP: accessory pathway, CS: coronary sinus, HRA: high right atrium, RVa d: right ventricle apex distal, ABL: ablation, D: distal, P: proximal.
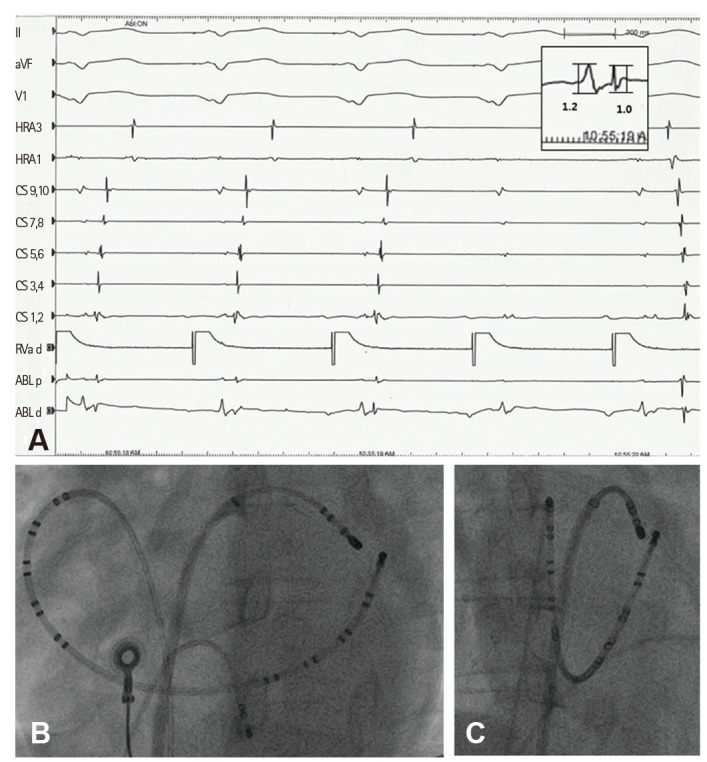
Fig. 2
Boxplot of atrial and ventricular amplitude potentials. Each potential was recorded from an ablation catheter at the successful ablation site. I bars represent 95% confidential intervals. Black circles indicate outliers and a star indicates extreme values for outliers.
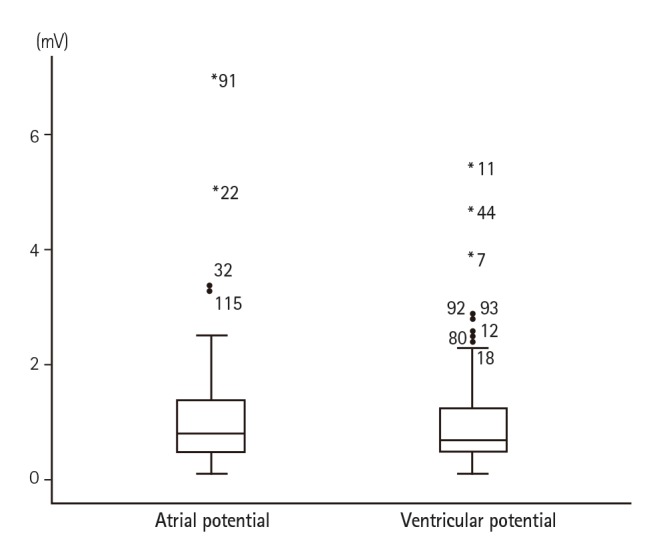
Table 1
Study population baseline characteristics
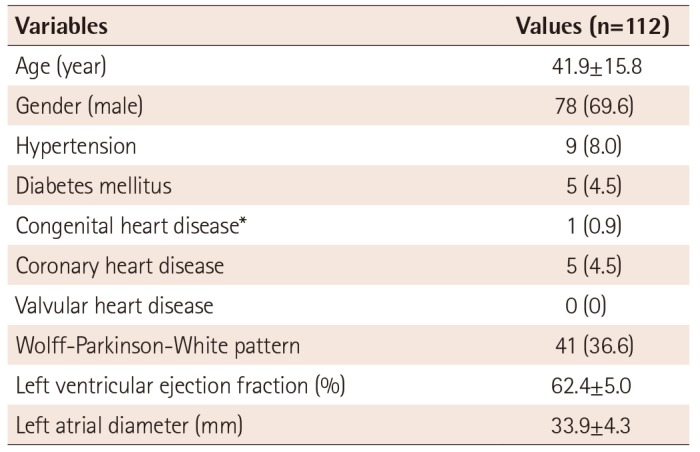
Table 2
Location of accessory pathways and rhythm status during catheter ablation
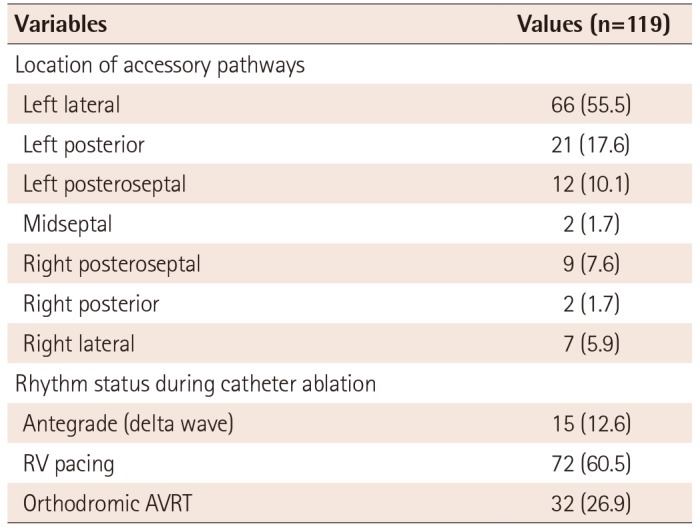
Table 3
Comparison of electrical potential amplitude by activation method or location of accessory pathways
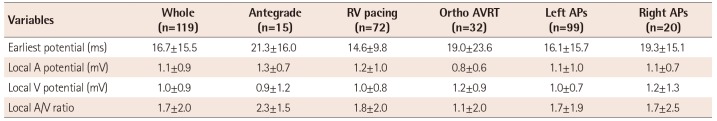
Table 4
Comparison of local A/V ratio by activation methods and location of accessory pathways (n=119)
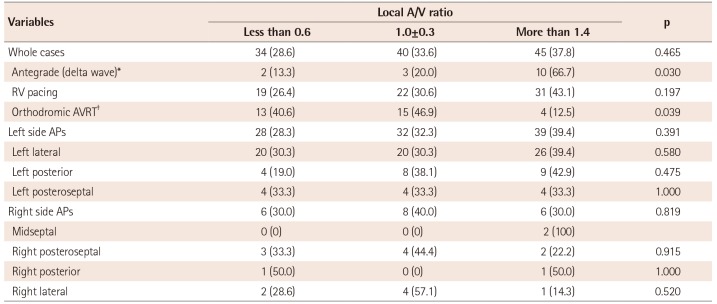
Values are presented as n (%). *Post-hoc analysis using the Bonferroni correction showed no statistically significant difference among the groups.
However, the ≥1.0±0.3 groups were statistically different from the less than 0.6 group (p=0.007). †Post-hoc analysis using the Bonferroni correction showed no statistically significant difference among the groups. However, the ≤1.0±0.3 groups were statistically different from the more than 1.4 group (p<0.001). A: atrial, APs: accessory pathways, AVRT: atrioventricular reentrant tachycardia, RV: right ventricle, V: ventricular




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download