Abstract
Background and Objectives
For the present study, we investigated the factors that influence the quality of standardized treatment for patients with post-cardiac arrest syndrome (PCAS) to improve the quality of PCAS treatment.
Subjects and Methods
We collected data on patients with cardiac arrest (CA) who were admitted to the intensive care units (ICUs) of 11 hospitals-Class II Grade A or above-in Suzhou from January to October 2013. Indexes of standardized treatment were observed within 72 hrs of CA. We analyzed monitoring techniques, monitoring frequency, ICU human and material resources, and intensivists' knowledge of PCAS treatment to explore how those factors affected the management of patients with PCAS.
Results
The bed/nurse ratio and the frequency with which core temperature was recorded correlated closely with the implementation of therapeutic hypothermia (TH) within 6 hrs of CA. The bed/doctor ratio and intensivists' knowledge about PCAS correlated closely with high-quality blood glucose control within 6 hrs of CA. Furthermore, the frequency with which core temperature was recorded was an independent factor influencing the quality of TH implementation, and the number times blood gas was analyzed was an independent factor influencing how well partial pressure of carbon dioxide was kept within the normal range in the 6 hrs after CA.
Post-cardiac arrest syndrome (PCAS) is a pathophysiological process of reperfusion injury following the restoration of spontaneous circulation (ROSC) after systemic ischemia caused by cardiac arrest (CA).1)2)3) Numerous studies have shown that early targeted therapies for blood pressure (BP), oxygen saturation (SPO2), partial pressure of carbon dioxide (PaCO2), glucose (Glu), and temperature (T) are closely correlated with outcomes in PCAS patients. Excessively high or low levels of these indices reduce patient survival or result in poor neurological outcomes.4)5)6)7) Our 2011 investigation on early targeted therapies in PCAS patients admitted to the intensive care units (ICUs) of 10 general hospitals in Suzhou found that the target achievement rate was low, and the overall level of standardized treatment was not high among PCAS patients.
Therefore, our research group developed the Early Standardized Treatment Program for PCAS Patients in the Suzhou Area, which has been implemented in the above-mentioned 10 hospitals and our hospital since 2013. In the present study, we investigated weaknesses in the implementation of the early standardized treatment program and explored the major factors that influence the quality of standardized care to provide clinical data for further improving the quality of treatment for PCAS patients and improving their outcomes.
This study was a multi-center retrospective cohort study. Subjects were patients with out-of-hospital or in-hospital CA who were admitted to the ICUs of 11 Class II Grade A or above general hospitals in the Suzhou area from January 1 to October 31, 2013, due to a sustained comatose state after ROSC by cardiopulmonary resuscitation (CPR). Inclusion criteria: 1) age ≥18 years; 2) suffered out-of-hospital or in-hospital CA and received CPR; 3) restored and maintained ROSC for at least 12 h; 4) had severe disturbance of consciousness (Glasgow score <8) after ROSC. Exclusion criteria: 1) presence of other causes of consciousness disturbance (e.g., severe traumatic brain injury, cerebrovascular accident); 2) endstage chronic diseases (e.g., cancer); 3) severe trauma (ISS score ≥16) or presence of massive hemorrhage (blood loss ≥1200 mL plus occurrence of hemorrhagic shock) and coagulopathy; 4) time elapsed from the onset of CA >24 h on ICU admission.
This study was accepted by the institutional review boards of Affiliated Kunshan Hospital of Nanjing University of Traditional Chinese Medicine and the Second Affiliated Hospital of Soochow University. We also received signed ethics approval from each patient.
In this study, we prepared relevant questionnaires, conducted a field investigation, examined instruments and equipment on site, assessed doctor knowledge, reviewed medical records, and collected early standardized treatment-related indices and key information about PCAS patients in the Suzhou area.
Patients' general information was collected in detail following the Utstein guidelines, including gender, age, underlying diseases, place and cause of CA, heart rate at initial monitoring, presence/absence of on-site CPR implementation by others (others CPR), and patient outcomes. Using the patients' progress notes and ICU records, we collected information on their standardized treatment following ROSC, including ways of monitoring key indices and monitoring and recording frequencies. Key indices were core temperatures (Tc, blood, vesical, and rectal temperatures), BP, SpO2, PaCO2, Glu, end-tidal partial pressure of carbon dioxide (EtCO2), central venous pressure (CVP), etc., for 72 h after ICU admission. In addition to analyzing data from the indices, we also assessed how well hospital staff monitored and controlled the indices (Table 1).
We collected basic information about the 11 hospitals' ICUs by field checking scheduling tables, instruments, and equipment, including the allocation of ICU human resources; the types, quantities, and properties of instruments and equipment required for standardized treatment; frequencies of instrument use by doctors (nurses); and whether the devices (technologies) were used for CPR patients (Table 2).
We assessed the knowledge of intensivists at all hospitals concerning PACS management using multi-time distribution of questionnaires, which were collected and quantified on site after completion (Table 3).
Medical staff allocation: In accordance with the specifications for ICU construction, a bed/doctor ratio ≥1:0.8 and nurse/bed ratio ≥1:2.5 are the basic requirements for ICU staffing.
Targets of key standardized treatment indices: mean arterial pressure (MAP) 65–100 mmHg, SPO2 ≥94%, PaCO2 35–45 mmHg, core temperatures 32–34℃, Glu 4.0–10.0 mmol/L. Achieving the 6 h standardized treatment target means that the patients reach the standardized targets for those key indices within 6 h after CA. TH target achievement within 72 h indicates that therapeutic hypothermia (TH) was implemented within 6–8 h after CA, with the target temperature, 32–34℃, reached and maintained for 12–24 h with a rewarming rate after discontinuation of TH of 0.25–0.5℃/h.
Definition and calculation of target achievement rate: The treatment target achievement rate refers to the number of times the parameters being monitored reached standardization requirements/total number of monitoring times×100%. The 6 h target achieved patient ratio after CA refers to the number of patients whose particular index reached the goal of standardized treatment within 6 h after CA/total number of patients×100%.
Statistical analysis was performed using the SPSS 19.0 software package (SPSS Inc., Chicago, IL, USA). Count data are expressed as rates and analyzed by χ2 test. Measurement data are expressed as means±standard deviations if distributed normally and as medians (interquartile ranges) if distributed abnormally. We used logistic regression analyses to assess which factors influence the quality of standardized treatment within 6 h following CA, including monitoring frequency, ICU bed/nurse ratio, bed/doctor ratio, and doctors' knowledge concerning standardized treatment (value was assigned as 1 if qualified and 0 if not qualified). Differences were considered statistically significant when p<0.05.
From January 1 to October 31, 2013, a total of 73 CA patients were admitted to the ICUs of the 11 general hospitals, of whom we included 52 in this study. In the end, 12 patients survived to hospital discharge, and 40 patients died (Fig. 1). As shown in Table 4, the survivor and death groups of patients did not differ statistically (p>0.05) in age, gender, underlying disease, CA incentives, arrhythmia, CPR or not, or time in the ICU. However, we did find a significant difference in the CA-ROSC time between the two groups (p<0.05).
Equipment allocation and usage: The ICUs of all 11 hospitals were equipped with multisystem monitors and bedside glucometers. 91% of the ICUs were equipped with invasive arterial pressure monitors, but among the 52 patients enrolled in this study, only 29% received invasive arterial pressure monitoring. All ICUs were equipped with temperature control devices, but only 52% of CA patients underwent core temperature monitoring, and 87% of patients received TH.
Monitoring and recording of key indices: We analyzed the monitoring (detection) and recording frequencies (per 24 h) of five key indices: Tc, BP, SpO2, PaCO2, and Glu. We found that the monitoring and recording frequencies for SpO2 and BP were 24 times/24 h; the median frequency of Tc recording was 18 (5–24) times/24 h; the median frequency of Glu detection and recording was 12 (6–12) times/24 h; and median frequency of PaCO2 detection was 2 (2–3) times/24 h (Table 5).
Target achievement rates of key indices within 6 h of CA: 92% of the 52 patients had their SpO2 up to treatment standards; the MAP target was reached in 67% of patients; the Glu target was reached in 29% of patients; the PaCO2 target was reached in 15% of patients; but only 14% of patients had up to standard Tc. Details are shown in Table 5.
72 h target achievement rates of key indices: the index closest to the targeted treatment standards (target achievement) was SpO2 (93.8%), followed by MAP and Glu (67.6% and 57.3%, respectively). PaCO2 and TH had the lowest target achievement rates, 35.3% and 19%, respectively. Details are shown in Table 5.
The 11 ICUs surveyed employed a total of 131 doctors and 326 nurses. These 11 ICUs had an average bed/nurse ratio of 1:1.9, and an average doctor/bed ratio of 1:0.77. Overall, the requirements of ICU construction specifications were not met.
We surveyed all 131 intensivists from the 11 hospitals. After excluding improperly completed forms, we analyzed 112 valid questionnaires, 85.5% of the total number of participants (112/131). The average score was 73.4 (full mark=100).
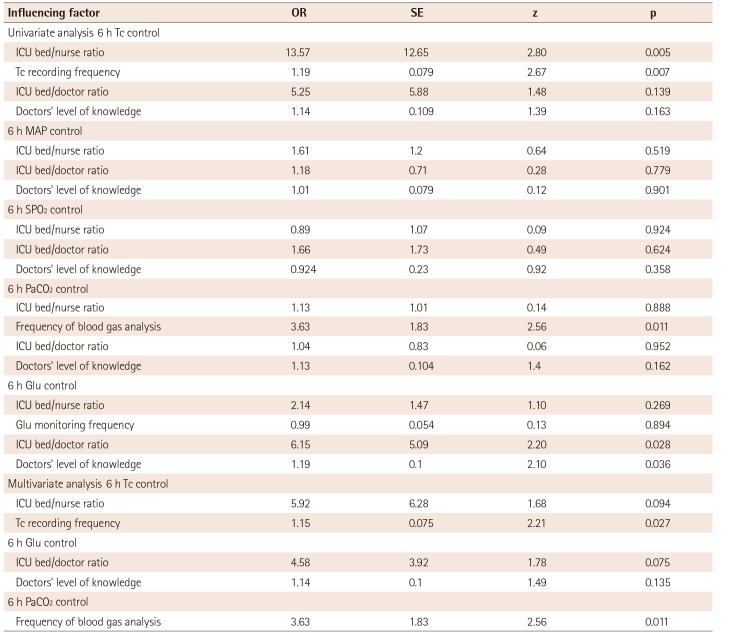
The ICU bed/nurse ratio and the Tc monitoring and recording frequency were major factors influencing the quality of TH implementation within 6 h of CA. The ICU bed/doctor ratio and doctors' relevant knowledge level were important factors influencing the quality of Glu control within 6 h of CA. Furthermore, the Tc monitoring and recording frequency was an independent factor influencing the quality of TH implementation within 6 h of CA, and the frequency of blood gas analysis was an independent factor influencing the quality of PaCO2 management within 6 h. Details are shown in Table 6.
With the gradual development of modern CPR technologies, the early success rate of CPR has been improving, but the prolonged, complete ischemia of vital organs caused by CA causes organisms enter a complex pathophysiological process after ROSC, leaving the proportion of patients who survive to be discharged from the hospital with good neurological recovery low.8)9) Standardized post-CA management has great significance for reducing early mortality, recovering neurological function, and improving the final outcomes for patients.10)11) Our earlier research showed that early target achievement rates for SpO2, MAP, PaCO2, and Glu were markedly higher in patients with good neurological outcomes than in those with poor neurological outcomes. We designed the present study to explore the factors that have influenced the control of key indices since the implementation of our standardized treatment program. The results show that the Tc monitoring and recording frequency is an independent factor influencing the quality of TH implementation within 6 h of CA, and the frequency of blood gas analysis is an independent factor influencing the quality of PaCO2 management within 6 h of CA.
With respect to TH, which had the lowest target achievement rate in this study, a retrospective study in California, USA, showed that between 1999 and 2008, only 11.3% (47/419) of hospitals used TH, and 0.4% (204/46833) of PCAS patients received TH; of those, TH implemented between 2006 and 2008 accounted for 87.3% (178/204) of cases, indicating a significantly higher implementation rate after the introduction of CPR guidelines than before.12)13) A physician questionnaire in the USA in 2005 on the reasons for the low target achievement rate in TH revealed that 87% of physicians had never used TH technology, with the main reasons cited being lack of evidence (49%), lack of an advanced cardiac life support application process (32%), and equipment limitations and technological difficulties (28%).14)15)
Based on the existing literature and guidelines and taking into account the specific circumstances of the Suzhou area, we have reached a consensus on the treatment indications, start time, hypothermic approaches, target temperature, hypothermic rate, and shivering prevention measures in TH. In this study, we found a significantly higher TH achievement rate than we found before standardization (TH achievement=5% in 2011). Nonetheless, the current rate remains unsatisfactory at only 19%. Our univariate analysis demonstrated that doctors have a basically unified understanding of TH management, but that knowledge is not significantly correlated with the quality of 6 h Tc control. The ICU bed/nurse ratio is a major factor influencing the quality of 6 h Tc control. In addition, the OR value of the bed/doctor ratio is high, indicating a certain correlation with insufficient staffing, which should be improved. Our multivariate analysis shows that the Tc monitoring and recording frequency is an independent factor influencing the quality of Tc control within 6 h of CA, which makes sense because only by timely monitoring and recording can deviations be discovered and adjusted. Another study by our research group also found that recording the temperature every 15 min using a special temperature record form, the “Cerebral Resuscitation Monitoring Record,” significantly improved the quality of TH.
Bedside arterial blood gas analysis has been widely implemented in the majority of ICUs; fast and timely PaCO2 detection is the most direct and effective means of assessing pulmonary ventilation function. In this study, we found that PaCO2 control rates within 6 h and 72 h following CA are low (15% and 35%), and the median frequency of PaCO2 detection is twice/24h. Detection frequency is an independent factor influencing the quality of PaCO2 control within 6 h. Arterial blood gas analysis is an invasive procedure that is not continuously operable, which affects both the detection frequency and control rate. Research has shown that collecting EtCO2 data, which requires a noninvasive, continuous monitoring approach, can guide ventilation therapy for ROSC patients and assess therapeutic efficacy. But we found in this study that the implementation rate of EtCO2 monitoring was only 15% (8/52), and among the monitored patients, only 20% (88/435) had readings within the normal range (35–45 mmHg).
This study has the following limitations: 1) due to its short duration, retrospective nature, and small number of patients enrolled, we could not analyze indices according to different outcomes; 2) the comprehensiveness and representativeness of the questionnaire item “Doctors' level of standardized PCAS treatment-related knowledge” needs further evaluation.
Acknowledgements
We would like to thank the 9 hospitals of this research group for their support and help: First Affiliated Hospital of Soochow University, Suzhou Municipal Hospital, Suzhou Hospital of Traditional Chinese Medicine, Changshu No. 1 People's Hospital, Changshu No. 2 People's Hospital, First People's Hospital of Kunshan, Taicang First People's Hospital, Wujiang First People's Hospital, and Zhangjiagang First People's Hospital. This work was supported by the Suzhou Social Development Foundation (SYS201063).
References
1. Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002; 346:557–563. PMID: 11856794.
2. Oddo M, Schaller MD, Feihl F, Ribordy V, Liaudet L. From evidence to clinical practice: effective implementation of therapeutic hypothermia to improve patient outcome after cardiac arrest. Crit Care Med. 2006; 34:1865–1873. PMID: 16715035.
3. Balan IS, Fiskum G, Hazelton J, Cotto-Cumba C, Rosenthal RE. Oximetry-guided reoxygenation improves neurological outcome after experimental cardiac arrest. Stroke. 2006; 37:3008–3013. PMID: 17068310.
4. Peberdy MA, Callaway CW, Neumar RW, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010; 122(18 Suppl 3):S768–S786. PMID: 20956225.
5. Coles JP, Fryer TD, Coleman MR, et al. Hyperventilation following head injury: effect on ischemic burden and cerebral oxidative metabolism. Crit Care Med. 2007; 35:568–578. PMID: 17205016.
6. Aufderheide TP. The problem with and benefit of ventilations: should our approach be the same in cardiac and respiratory arrest? Curr Opin Crit Care. 2006; 12:207–212. PMID: 16672778.
7. Karanjia N, Geocadin RG. Post-cardiac arrest syndrome: update on brain injury management and prognostication. Curr Treat Options Neurol. 2011; 13:191–203. PMID: 21249482.
8. Losert H, Sterz F, Roine RO, et al. Strict normoglycaemic blood glucose levels in the therapeutic management of patients within 12h after cardiac arrest might not be necessary. Resuscitation. 2008; 76:214–220. PMID: 17870226.
9. Cueni-Villoz N, Devigili A, Delodder F, et al. Increased blood glucose variability during therapeutic hypothermia and outcome after cardiac arrest. Crit Care Med. 2011; 39:2225–2231. PMID: 21705888.
10. Soar J, Nolan JP. Mild hypothermia for post cardiac arrest syndrome. BMJ. 2007; 335:459–460. PMID: 17823147.
11. Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002; 346:549–556. PMID: 11856793.
12. Abella BS, Rhee JW, Huang KN, Vanden Hoek TL, Becker LB. Induced hypothermia is underused after resuscitation from cardiac arrest: a current practice survey. Resuscitation. 2005; 64:181–186. PMID: 15680527.
13. Tran BP, McGuire CV, Maloney MA. Use of mild therapeutic hypothermia improves outcomes in cardiac arrest. JAAPA. 2010; 23:43–48. PMID: 20232725.
14. Liu L, Zhu J, Yang L, Zhang Y. Neurological outcomes of patients admitted to the intensive care unit for cardiac arrest. Chin Med J (Engl). 2014; 127:3024–3026. PMID: 25131245.
15. Jena AB, Romley JA, Newton-Cheh C, Noseworthy P. Therapeutic hypothermia for cardiac arrest: real-world utilization trends and hospital mortality. J Hosp Med. 2012; 7:684–689. PMID: 23023977.
Fig. 1
Flow chart of patient inclusion and outcomes. CA: cardiac arrest, ICU: intensive care unit, ROSC: restoration of spontaneous circulation, GCS: glasgow coma scale.
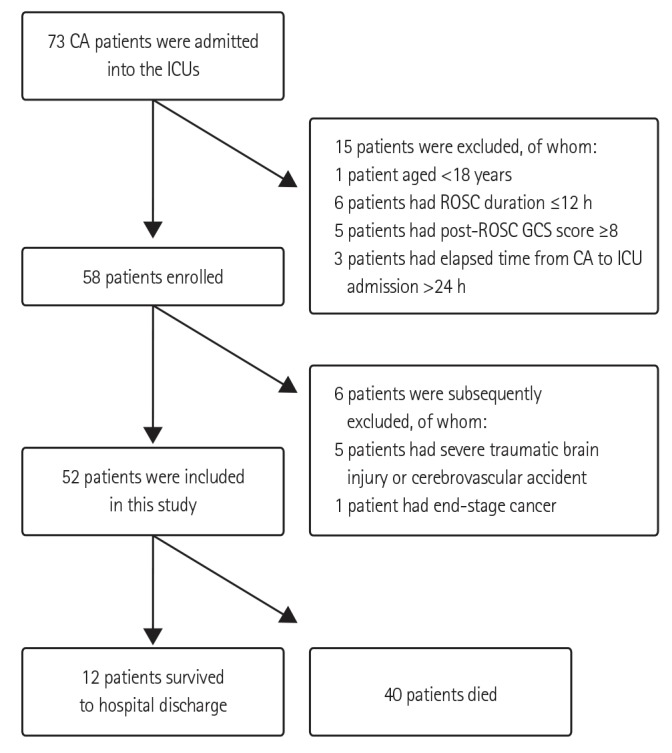
Table 1
Hemodynamic early goals and measures (reach the standards as soon as possible, within six hours of ICU admission)
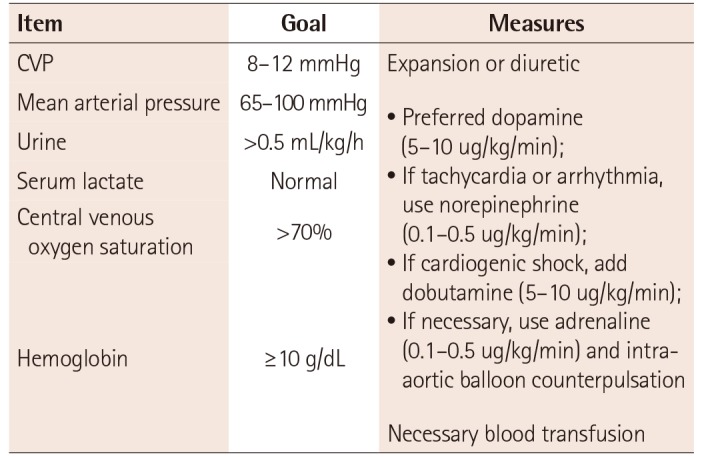
Table 2
Objectives and measures for gas exchange (reach standard as soon as possible, within six hours of ICU admission)
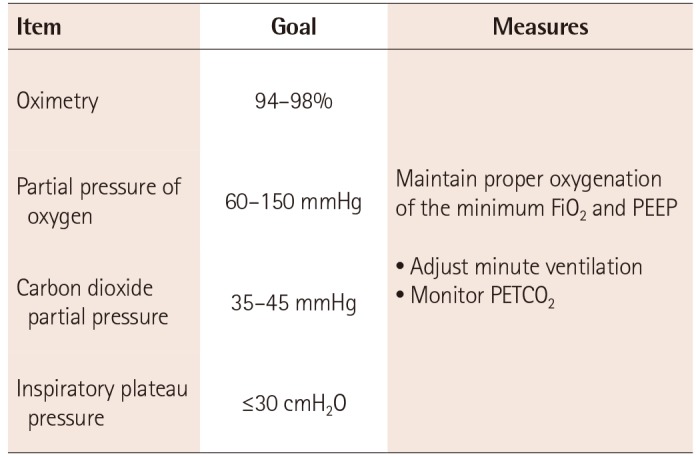
Table 3
Therapeutic hypothermia
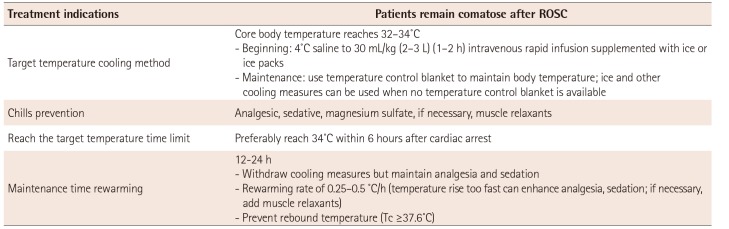
Table 4
General data of the two groups
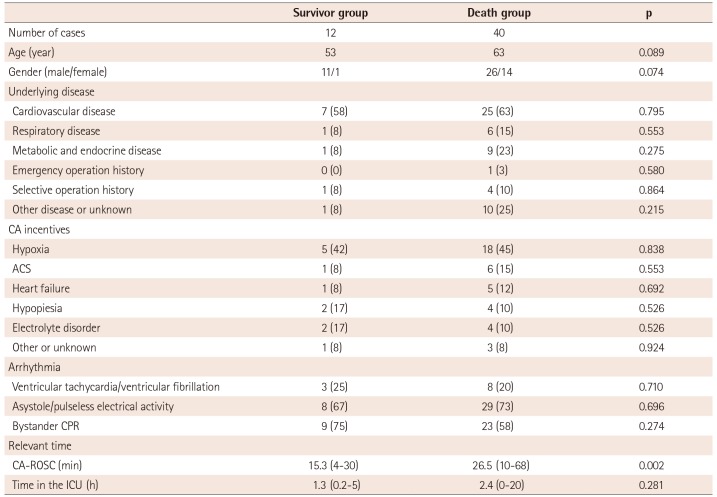
Table 5
Equipment allocation, technology implementation, and target achievement information for standardized treatment of PCAS patients
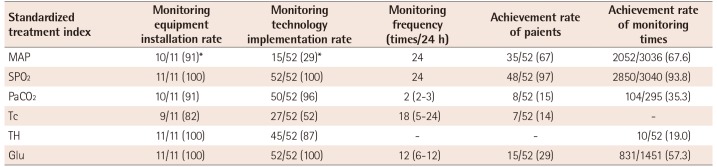
Values are presented as rate (%). *Invasive arterial pressure monitoring. PCAS: post-cardiac arrest syndrome, MAP: mean arterial pressure, SPO2: saturation of peripheral oxygen, PaCO2: partial pressure of carbon dioxide in arterial blood, Tc: core temperature, TH: therapeutic hypothermia, Glu: fingertip capillary blood glucose
Table 6
Analysis of factors influencing the quality of early standardized treatment in PCAS patients




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download