Abstract
Coronary magnetic resonance angiography (CMRA) allows a noninvasive assessment of the coronary anatomy without exposing the patients to radiation. It is also superior to coronary computed tomography angiography (CCTA) for the evaluation of luminal narrowing in heavily calcified coronary segments. We report a case with triple-vessel disease, but it could not be accurately assessed by CCTA because of calcification and lack of a significant perfusion defect or myocardial scarring on cardiac magnetic resonance imaging (MRI). However, whole-heart CMRA performed as part of the cardiac MRI protocol demonstrated significant triple-vessel disease with left main involvement, confirmed by subsequent invasive angiography with a fractional flow reserve measurement.
While cardiac magnetic resonance imaging (MRI) has been used to evaluate the myocardium in terms of the myocardial function, perfusion, and viability, rather than coronary stenosis; coronary magnetic resonance angiography (CMRA) is currently considered a reliable imaging test for the evaluation of coronary anatomy.1) This paper reports a case with triple-vessel disease that could not be accurately assessed by coronary computed tomography angiography (CCTA) because of calcification, and without significant perfusion defects or scar changes observed on a cardiac MRI. However, whole-heart CMRA performed as part of the cardiac MRI protocol demonstrated significant triple-vessel disease with left main (LM) involvement, as confirmed by subsequent invasive angiography with a fractional flow reserve measurement.
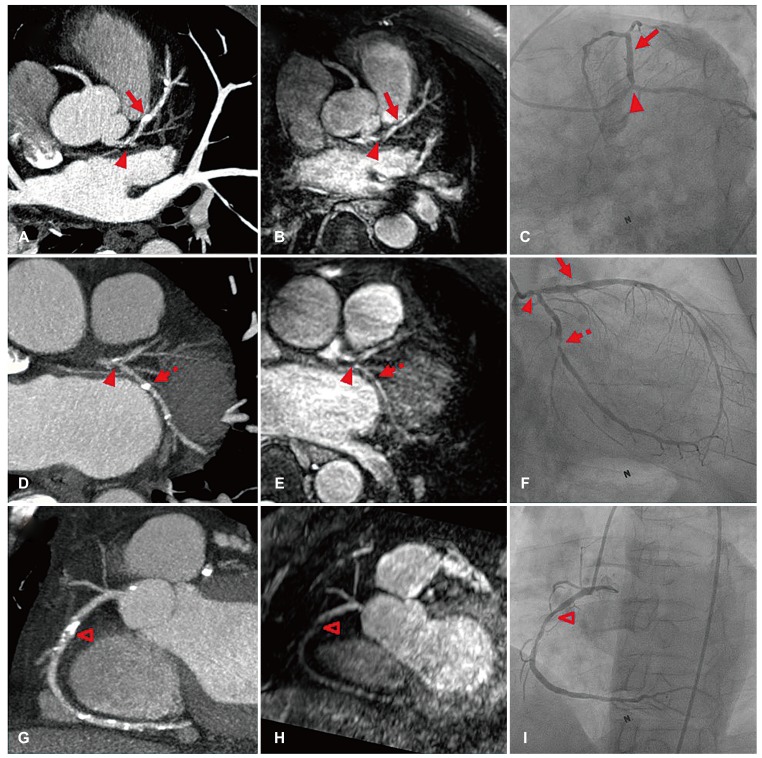
A 63-year-old man presented with a 1-month history of exertional chest pain. He had a history of hypertension, diabetes mellitus, dyslipidemia, and ischemic stroke. CCTA using a 256-slice multi-detector computed tomography scanner (Brilliance iCT; Philips Medical Systems, Best, Netherlands) showed multifocal stenoses in the LM bifurcation, proximal left anterior descending artery (LAD), proximal left circumflex artery (LCX), and mid right coronary artery (RCA) (Fig. 1A, D, G). While significant stenosis was suspected in the LM bifurcation, it was difficult to evaluate the stenosis severity of the LAD, LCX, and RCA because of heavy calcification.
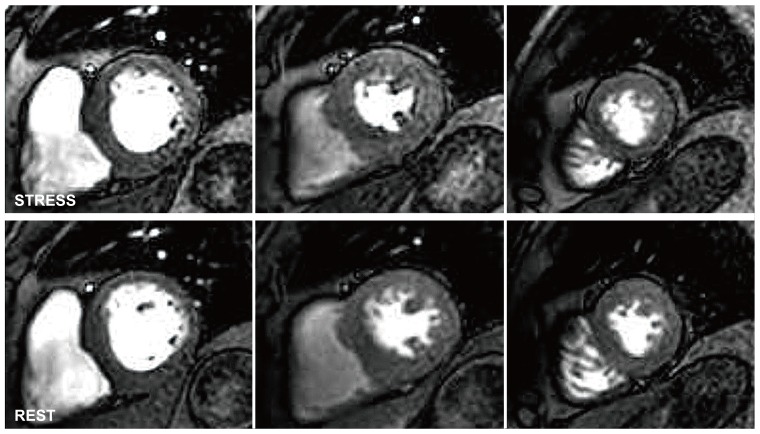
We subsequently performed a cardiac MRI using a 3-T MR system (Ingenia; Philips Medical Systems, Best, Netherlands) to evaluate myocardial ischemia and viability.2) Despite the multifocal stenoses of the coronary arteries observed on CCTA, neither evidence of inducible myocardial ischemia on adenosine stress myocardial perfusion MRI (Fig. 2) nor evidence of a myocardial scar on late gadolinium enhanced MRI was observed. However, when we performed a quantitative analysis of stress-rest images, the myocardial perfusion reserve indices for all segments were significantly decreased (range, 0.48-0.99), and the myocardial blood flow reserve estimated from the coronary sinus flow was only 1.4. Moreover, a non-contrast enhanced whole-heart CMRA demonstrated significant stenosis of the LM bifurcation (Fig. 1B). Calcified plaques in the proximal LCX and mid RCA were also identified as significant stenoses on CMRA (Fig. 1E, H), while the calcified plaque in the proximal LAD was indicated as an insignificant lesion (Fig. 1B).
Invasive coronary angiography revealed critical stenoses in the LM bifurcation, proximal LCX, and mid RCA, whereas that in the proximal LAD appeared insignificant (Fig. 1C, F, I). The fractional flow reserve values of the LAD, LCX, and RCA were 0.50, 0.59, and 0.81, respectively. Considering that stress perfusion MRI did not demonstrate a significant perfusion defect despite the presence of hemodynamically significant stenosis and impaired perfusion reserve, taken together, the findings indicated a balanced three-vessel coronary artery disease (CAD). Thus, a percutaneous coronary intervention to the LM bifurcation, proximal LCX, and mid RCA was performed.
Assessment of the coronary arteries by cardiac MRI is challenging, owing to the small size of the vessels and the complex motions caused by cardiac contractions and respiration.2) However, in the past decades, considerable technical advances have been made, and the imaging time, success rate, and diagnostic accuracy of CMRA have steadily improved.2)3) Moreover, CMRA allows a noninvasive assessment of the coronary anatomy without exposing the patients to radiation, and is superior to CCTA for the evaluation of luminal narrowing in heavily calcified coronary segments.1) In the present case, a whole-heart CMRA was useful in determining the significance of coronary stenoses that cannot be assessed by CCTA because of coronary calcification.4)5) Moreover, the patient's condition might have been missed without CMRA, since myocardial perfusion MRI failed to detect a significant triple-vessel disease. This is an unusual case since myocardial perfusion MRI is known to be less susceptible to balanced ischemia (a false negative finding), owing to its high spatial resolution.6) Quantitative myocardial perfusion analysis showed a significantly decreased myocardial perfusion reserve index in the present case. However, quantitative analysis is not routinely performed in our daily clinical practice and is largely confined to the research field, since it is still laborious and time-consuming. Considering that CMRA can be easily performed as part of comprehensive cardiac MRI examinations, this case highlights the value of CMRA for the detection and evaluation of CAD. The incorporation of CMRA with cine, stress perfusion, and late gadolinium-enhanced MRI allows a comprehensive assessment of CAD by combining functional and anatomic evaluations.
Acknowledgments
This case report was supported by a Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2014R1A1A3051343).
References
1. Sakuma H. Coronary CT versus MR angiography: the role of MR angiography. Radiology. 2011; 258:340–349. PMID: 21273518.
2. Yoon YE, Hong YJ, Kim HK, et al. 2014 Korean guidelines for appropriate utilization of cardiovascular magnetic resonance imaging: a joint report of the Korean society of cardiology and the Korean society of radiology. Korean Circ J. 2014; 44:359–385. PMID: 25469139.
3. Kato S, Kitagawa K, Ishida N, et al. Assessment of coronary artery disease using magnetic resonance coronary angiography: a national multicenter trial. J Am Coll Cardiol. 2010; 56:983–991. PMID: 20828652.
4. Schuijf JD, Achenbach S, de Feyter PJ, Bax JJ. Current applications and limitations of coronary computed tomography angiography in stable coronary artery disease. Heart. 2011; 97:330–337. PMID: 21258119.
5. Schroeder S, Achenbach S, Bengel F, et al. Cardiac computed tomography: indications, applications, limitations, and training requirements: report of a writing group deployed by the working group nuclear cardiology and cardiac CT of the European society of cardiology and the European council of nuclear cardiology. Eur Heart J. 2008; 29:531–556. PMID: 18084017.
6. Chung SY, Lee KY, Chun EJ, et al. Comparison of stress perfusion MRI and SPECT for detection of myocardial ischemia in patients with angiographically proven three-vessel coronary artery disease. AJR Am J Roentgenol. 2010; 195:356–362. PMID: 20651190.
Supplementary Materials
The online-only Data Supplements are available with this article
at http://doi.org/10.4070/kcj.2016.0288.
Fig. 1
CCTA, CMRA, and invasive CAG findings. CCTA revealed multifocal coronary artery disease in the left main bifurcation (A, D, arrowheads), proximal left anterior descending artery (A, arrow), proximal left circumflex artery (D, dotted arrow), and mid right coronary artery (G, open arrowhead). Although the CCTA evaluation of the stenosis severity was limited because of calcification (A, D, G), whole-heart CMRA demonstrated significant stenoses of the left main bifurcation (B, E, arrowheads), proximal left circumflex artery (E, dotted arrow), and mid right coronary artery (H, open arrowhead). On the other hand, the calcified plaque in the proximal left anterior descending artery was indicated as an insignificant lesion on CMRA (B, arrow). Good agreement was observed between CMRA and subsequent CAG (C, F, I). CCTA: coronary computed tomography angiography, CMRA: coronary magnetic resonance angiography, CAG: coronary angiography.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download