Abstract
Background and Objectives
The clinical outcome of patient with an acute myocardial infarction (AMI) undergoing percutaneous coronary intervention (PCI), with or without achievement of target low density lipoprotein-cholesterol (LDL-C), has little known information. This study investigated if target LDL-C level (below 70 mg/dL) achievements in patients with AMI showed better clinical outcomes or not.
Subjects and Methods
Between May 2008 and September 2012, this study enrolled 13473 AMI patients in a large-scale, prospective, multicenter Korean Myocardial Infarction (KorMI) registry. 12720 patients survived and 6746 patients completed a 1-year clinical follow up. Among them 3315 patients received serial lipid profile follow-ups. Propensity score matching was applied to adjust for differences in clinical baseline and angiographic characteristics, producing a total of 1292 patients (646 target LDL-C achievers vs. 646 non-achievers). The primary end point was the composite of a 1-year major adverse cardiac event (MACE) including cardiac death, recurrent myocardial infarction (MI), target lesion revascularization (TLR) and coronary artery bypass grafting.
Results
After propensity score matching, baseline clinical and angiographic characteristics were similar between the two groups. Clinical outcomes of the propensity score matched patients who showed no significant differences in cardiac death (0.5% vs. 0.5%, p=1.000), recurrent MI (1.1% vs. 0.8%, p=0.562), TLR (5.0% vs. 4.5%, p=0.649), MACEs (6.5% vs. 5.9%, p=0.644) and stent thrombosis (2.5% vs. 1.9%, p=0.560).
Lots of studies have reported that the risk of cardiovascular (CV) events decreases with low density lipoprotein-cholesterol (LDL-C) reduction, and the risk of recurrent cardiovascular events and survival improvement in patients with acute myocardial infarction (AMI) is reduced by using statin.1)2) Therefore, statin is a class IA American College of Cardiology (ACC)/American Heart Association (AHA) recommendation for secondary prevention of atherosclerotic coronary heart disease.3)
In 2011, the European Atherosclerosis Society (EAS)/European Society of Cardiology (ESC) joint guidelines emphasized that LDL-C is still the most important marker to treat targets, regardless of LDL-C levels, with target LDL-C <70 mg/dL, statin therapy should be initiated after AMI,4)5) However, there are still arguments for the use of statin in low LDL-C patients; on the other hands, lots of hyperlipidemia patients with AMI in current practice do not attain the guideline-recommended target LDL-C level.6)7) In addition, the influence of the intensity of statin therapy as represented by the achieved level of LDL-C on cardiovascular outcomes in patients with AMI has not been fully evaluated.8)
Now, the clinical outcome of patients suffering from AMI undergoing percutaneous coronary intervention (PCI) with or without achievement of target LDL-C has little known information. This study investigated is target LDL-C level (below 70 mg/dL) achievements in patients with AMI showed better clinical outcomes or not.
The Korean Acute Myocardial Infarction Registry (KAMIR), is a prospective, open, observational, multicenter, online, nationwide registry of AMI, conducted from November 2005 to January 2008, and its successor, the Korean Myocardial Infarction (KorMI) registry, conducted from January 2008; these registries were supported by the Korean Working Group of Acute Myocardial Infarction. The aims and protocols of the registries have been published. The protocols of the two prospective cohorts were similar. Participating centers included 53 university or community hospitals that have high volumes of patients with facilities for primary PCI and onsite cardiac surgery. The study protocol was reviewed and approved by the institutional review board at each participating center. AMI was diagnosed by characteristic clinical presentations, serial changes on the electrocardiogram suggesting infarction or injury, and increase in cardiac enzymes. We analyzed baseline demographic characteristics, initial presentation, initial vital signs, electrocardiographic findings, results of laboratory tests, procedural data, and medications. Blood samplings for baseline laboratory tests, except for the lipid measurement, were collected at admission or before PCI. Patients were required to fasting overnight and the following day blood was sampled for lipid levels. The LDL-C levels were calculated by the Friedewald formula. Patients with a triglyceride (TG) level ≥400 mg/dL were excluded. A left ventricular ejection fraction was determined by 2-dimensional echocardiography. In-hospital complications and their management were also recorded. 12-month major adverse cardiac events (MACEs) were defined as the composite of a 1-year MACEs including cardiac death, recurrent myocardial infarction (MI), target lesion revascularization (TLR) and coronary artery bypass grafting (CABG). Follow up data were obtained by reviewing medical records and telephone interviews with patients. All data were recorded on an electronic Web page–based case-report form.
Data are expressed as a mean±SD and frequencies are expressed as percentages. Propensity score matching to adjust for potential biases and confounding was applied to adjust for differences in clinical baseline and angiographic characteristics, producing a total of 1292 patients (646 target LDL-C achievers vs. 646 non-achievers). In the propensity-matched cohort, all comparisons between the two groups were tested using a paired t-test for continuous variables and Mc Nemar test for categorical variables. A probability value of p<0.05 was considered significant. All statistical analyses were performed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA).
The flow of subjects through the study is shown in Fig. 1. Between January 2008 and September 2012, 13473 patients were enrolled in the KorMI, with a final diagnosis of AMI. There were 753 (5.6%) hospital deaths; therefore, a total of 12720 patients survived and 6746 patients completed a 1-year clinical follow up. Among them 3315 patients received an LDL-C follow up. Propensity score matching was applied to adjust for differences in clinical baseline and angiographic characteristics, producing a total of 1292 patients (646 target LDL-C achievers vs. 646 non-achievers). After propensity score matching, baseline clinical and angiographic characteristics were similar between the two groups (Table 1). Baseline LDL-C was 120.9±28.6 mg/dL in target LDL-C achievers and 120.5±32.8 mg/dL in non-achievers, respectively.
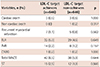
The LDL-C target achiever's LDL-C level was 56.8±9.5 mg/dL and nonachiever's LDL-C was 96.3±24.3 mg/dL, respectively (Table 2). Total cholesterol (121.8±19.4 mg/dL vs. 163.1±29.8 mg/dL, p=0.0001), TG (127.7±94.6 mg/dL vs. 143.7±79.0 mg/dL, p=0.001) were different significantly but not different in high density lipoprotein-cholesterol (HDL-C) (42.3±16.8 mg/dL vs. 43.3±12.5 mg/dL, p=0.276). There were 3 (0.5%) cardiac deaths, 7 (1.1%) recurrent myocardial infarctions, 32 (5.0%) TLRs, 14 (2.2%) target vessel revascularizations (TVR), 1 (0.2%) CABG, and 15 (2.5%) stent thromboses in LDL-C target achievers Results for LDL-C non-achievers included 3 (0.5%) cardiac deaths, 1 (0.2%) non-cardiac deaths, 5 (0.8%) recurrent MIs, 29 (4.5%) TLRs, 8 (1.2%) TVRs, 1 (0.2%) CABGs, and 12 (1.9%) stent thromboses. Clinical outcomes of the propensity score matched two groups showed no significant differences in cardiac deaths (0.5% vs. 0.5%, p=1.000), recurrent MIs (1.1% vs. 0.8%, p=0.562), TLRs (5.0% vs. 4.5%, p=0.649), MACEs (6.5% vs. 5.9%, p=0.644) and stent thromboses (2.5% vs. 1.9%, p=0.560, Table 3).
Elevation of total cholesterol and LDL-C has received the most attention, particularly because it can be modified by lifestyle changes and drug therapies. Significant associations between higher total cholesterol and LDL-C levels and a higher incidence of cardiovascular events have been repeatedly published.9)10)11) Meta-analyses of many trials show a clear dose-dependent relative reduction in cardiovascular disease with LDL-C lowering.12)13)14) Every 1.0 mmoL/L reduction in LDL-C is associated with a corresponding 20-25% reduction in cardiovascular mortality and non-fatal myocardial infarction.14)15)16)17)18) More recently, trials have confirmed that lowering LDL-C to <1.8 mmoL/L (70 mg/dL) is associated with the lowest risk of recurrent cardiovascular events in secondary prevention populations. Therefore, LDL-C is a cornerstone of secondary prevention and reporting evidence-based approached to risk reduction after an AMI. Based on the results from the TNT and other randomized controlled studies, “the lower, the better” hypothesis has been widely advocated with regard to optimal treatment LDL-C levels in patients with coronary artery disease.1) However, it has not yet been proven whether a lower level of LDL-C itself was the predominant mechanism of better outcomes in the atorvastatin 80 mg group of the TNT study.1)
Statin, by decreasing LDL-C, reduces cardiovascular morbidity and mortality as well as the need for coronary artery interventions. Statin effectively reduces LDL-C by 50% also seems to halt progression or even contribute to regression of coronary atherosclerosis. Experimental studies have demonstrated that statin therapy decreases the extent of myocardial necrosis, preserves myocardial viability, and results in increased ventricular function in models of myocardial ischemia reperfusion injury. Statins' cardioprotective effect after AMI during long-term treatment can be partly explained by their pleiotropic effects, such as anti-inflammatory, antiplatelet, and antithrombotic properties, and improvements in endothelial function. It is obvious that statin therapy with its LDL-C lowering effect provides clinical benefits in the secondary prevention for AMI patients. However, a considerable number of untreated patients with AMI are still eligible for statin therapy.19)20)21)22)23) There are still arguments of the use of statin in having patients with a low LDL-C.24)25)
The main finding of this study is that achieved target LDL-C levels <70 mg/dL were not associated with a lower risk for cardiovascular events as compared with target LDL-C non-achievers. Although the nonachiever's LDL-C levels are relatively low (96.3±24.3 mg/dL) and 78.8% of patients use statin, we can suggest that just a low LDL-C level itself, regardless use of statin, is not always related to better clinical outcomes, suggesting that the LDL-C level itself might not critically influence the risk for cardiovascular events. Thus, “the lower the better” may not be always applicable. It also might be possible that even with less LDL-C reduction, the pleiotropic effects of the statin influenced the risk reduction even in the LDL-C ≥70 mg/dL group. We do not currently know the specific threshold level of LDL-C above which the high level of LDL-C level itself can be an independent risk factor for future cardiovascular events.26)27)28) This study may suggest that LDL-C levels ≥70 mg/dL might not be a risk for future cardiovascular events. And “makes LDL-C lower with statin” should be always addressed in secondary prevention, however more intensive LDL-C lowering may not be recommended just only based on LDL-C level.
There are several potential limitations of our study. First, our analyses depended on patients who participated in serial laboratory studies which could make them less representative of the general AMI patients. Second, we were unable to examine long term adherence to specific medications prescribed at the time of discharge and we couldn't analyze according to the specific statin type, dose, and lower-cost but, generic statins were also used.
In conclusion, in this propensity-matched comparison, target LDL-C (below 70 mg/dL) achievement in AMI patients undergoing PCI did not show the better clinical outcomes.
Figures and Tables
Fig. 1
Patients disposition. AMI: acute myocardial infarction, KorMI: Korean Myocardial Infarction, LDL-C: low density lipoprotein-cholesterol.

Table 1
Baseline characteristics

Values presented as mean±standard deviation or number (%). LDL-C: low density lipoprotein-cholesterol, IHD: ischemic heart disease, CAD: coronary artery disease, SBP: systolic blood pressure, DBP: diastolic blood pressure, HR: heart rate, HDL-C: high density lipoprotein-cholesterol, STEMI: ST-elevation myocardial infarction, NSTEMI: non ST-elevation myocardial infarction, PCI: percutaneous coronary intervention, ACEi: angiotensin converting enzyme inhibitor, ARB: angiotensin receptor blocker, CCB: calcium channel blocker
Table 2
One year follow up lipid profile
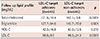
Table 3
Cumulative clinical outcomes and stent thrombosis up to 1-year
References
1. LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005; 352:1425–1435.
2. Schwartz GG, Olsson AG, Ezekowitz MD, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. JAMA. 2001; 285:1711–1718.
3. Canadian Cardiovascular Society; American Academy of Family Physicians; American College of Cardiology, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008; 51:210–247.
4. Catapano AL, Reiner Z, De Backer G, et al. ESC/EAS Guidelines for the management of dyslipidaemias The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Atherosclerosis. 2011; 217:3–46.
5. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol. 2004; 44:720–732.
6. Martin SS, Gosch K, Kulkarni KR, et al. Modifiable factors associated with failure to attain low-density lipoprotein cholesterol goal at 6 months after acute myocardial infarction. Am Heart J. 2013; 165:26–33.e3.
7. Lee JH, Yang DH, Park HS, et al. Korea Acute Myocardial Infarction Registry Investigators. Suboptimal use of evidence-based medical therapy in patients with acute myocardial infarction from the Korea Acute Myocardial Infarction Registry: prescription rate, predictors, and prognostic value. Am Heart J. 2010; 159:1012–1019.
8. Natsuaki M, Furukawa Y, Morimoto T, et al. Intensity of statin therapy, achieved low-density lipoprotein cholesterol levels and cardiovascular outcomes in Japanese patients after coronary revascularization. Perspectives from the CREDO-Kyoto registry cohort-2. Circ J. 2012; 76:1369–1379.
9. Morrissey RP, Diamond GA, Kaul S. Statins in acute coronary syndromes: do the guideline recommendations match the evidence? J Am Coll Cardiol. 2009; 54:1425–1433.
10. Law MR, Wald NJ, Thompson SG. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ. 1994; 308:367–372.
11. Briel M, Schwartz GG, Thompson PL, et al. Effects of early treatment with statins on short-term clinical outcomes in acute coronary syndromes: a meta-analysis of randomized controlled trials. JAMA. 2006; 295:2046–2056.
12. Cholesterol Treatment Trialists' (CTT) Collaboration. Baigent C, Blackwell L. CTT) Collaboration, Baigent C, Blackwell L, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010; 376:1670–1681.
13. Brown BG, Stukovsky KH, Zhao XQ. Simultaneous low-density lipoprotein-C lowering and high-density lipoprotein-C elevation for optimum cardiovascular disease prevention with various drug classes, and their combinations: a meta-analysis of 23 randomized lipid trials. Curr Opin Lipidol. 2006; 17:631–636.
14. LaRosa JC, He J, Vupputuri S. Effect of statins on risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA. 1999; 282:2340–2346.
15. Lenderink T, Boersma E, Gitt AK, et al. Patients using statin treatment within 24 h after admission for ST-elevation acute coronary syndromes had lower mortality than non-users: a report from the first Euro Heart Survey on acute coronary syndromes. Eur Heart J. 2006; 27:1799–1804.
16. Stenestrand U, Wallentin L. Swedish Register of Cardiac Intensive Care (RIKS-HIA). Early statin treatment following acute myocardial infarction and 1-year survival. JAMA. 2001; 285:430–436.
17. Bybee KA, Wright RS, Williams BA, Murphy JG, Holmes DR Jr, Kopecky SL. Effect of concomitant or very early statin administration on in-hospital mortality and reinfarction in patients with acute myocardial infarction. Am J Cardiol. 2001; 87:771–774.
18. Walter DH, Fichtlscherer S, Britten MB, Auch-Schwelk W, Schächinger V, Zeiher AM. Benefits of immediate initiation of statin therapy following successful coronary stent implantation in patients with stable and unstable angina pectoris and Q-wave acute myocardial infarction. Am J Cardiol. 2002; 89:1–6.
19. Karlson BW, Nicholls SJ, Lundman P, Palmer MK, Barter PJ. Achievement of 2011 European low-density lipoprotein cholesterol (LDL-C) goals of either <70 mg/dl or ≥ 50% reduction in high-risk patients: results from VOYAGER. Atherosclerosis. 2013; 228:265–269.
20. Davidson MH, Maki KC, Pearson TA, et al. Results of the National Cholesterol Education (NCEP) Program Evaluation ProjecT Utilizing Novel E-Technology (NEPTUNE) II survey and implications for treatment under the recent NCEP Writing Group recommendations. Am J Cardiol. 2005; 96:556–563.
21. Santos RD, Waters DD, Tarasenko L, et al. L-TAP 2 Investigators. Low- and high-density lipoprotein cholesterol goal attainment in dyslipidemic women: The Lipid Treatment Assessment Project (L-TAP) 2. Am Heart J. 2009; 158:860–866.
22. Melloni C, Shah BR, Ou FS, et al. Lipid-lowering intensification and low-density lipoprotein cholesterol achievement from hospital admission to 1-year follow-up after an acute coronary syndrome event: results from the Medications ApplIed aNd SusTAINed Over Time (MAINTAIN) registry. Am Heart J. 2010; 160:1121–1129.
23. Baessler A, Fischer M, Huf V, et al. Failure to achieve recommended LDL cholesterol levels by suboptimal statin therapy relates to elevated cardiac event rates. Int J Cardiol. 2005; 101:293–298.
24. Wiviott SD, Cannon CP, Morrow DA, et al. Can low-density lipoprotein be too low? The safety and efficacy of achieving very low low-density lipoprotein with intensive statin therapy: a PROVE IT-TIMI 22 substudy. J Am Coll Cardiol. 2005; 46:1411–1416.
25. Hayward RA, Hofer TP, Vijan S. Narrative review: lack of evidence for recommended low-density lipoprotein treatment targets: a solvable problem. Ann Intern Med. 2006; 145:520–530.
26. Lee JH, Park SH, Yang DH, et al. Korea Acute Myocardial Infarction Registry Investigators. Threshold level of low-density lipoprotein cholesterol for the short-term benefit of statin therapy in the acute phase of myocardial infarction. Clin Cardiol. 2012; 35:211–218.
27. Teramoto T, Nakaya N, Yokoyama S, et al. Association between lowering low-density lipoprotein cholesterol with pravastatin and primary prevention of cardiovascular disease in mild to moderate hypercholesterolemic Japanese. J Atheroscler Thromb. 2010; 17:879–887.
28. Itakura H, Kita T, Mabuchi H, et al. Relationship between coronary events and serum cholesterol during 10 years of low-dose simvastatin therapy: long-term efficacy and safety in Japanese patients with hypercholesterolemia in the Japan Lipid Intervention Trial (J-LIT) Extension 10 Study, a prospective large-scale observational cohort study. Circ J. 2008; 72:1218–1224.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download