Abstract
Background and Objectives
Endomyocardial biopsy is obligatory during the first year after heart transplant (HTx) for the surveillance of acute rejection. Previous attempts using cardiac biomarkers for the detection of rejection failed to show enough evidence to substitute endomyocardial biopsy. Therefore, this study sought the possibility of using soluble ST2 (sST2), a novel cardiovascular marker, as a surrogate marker for acute allograft rejection after HTx.
Subjects and Methods
A total of 494 blood samples acquired at the time of endomyocardial biopsy were analyzed in 67 HTx cases from September 2006 to August 2014. Significant rejection was defined as International Society of Heart and Lung Transplant (ISHLT) score ≥2R and humoral rejection accompanied by hemodynamic instability.
Results
Twenty cases of HTx with 22 blood samples showed significant rejection in endomyocardial biopsy at 4.0 (2.0-9.0) months after HTx. The level of sST2 showed positive correlation with cardiac troponin I, and N-terminal pro-B-type natriuretic peptide (all p<0.001), and negative correlation with post-HTx months (p<0.001). The levels of sST2 according to the ISHLT scores were 36 (19-98), 28 (18-62), 15 (16-37), and 191 (85-343) ng/mL, consecutively 0R, 1R, 2R, and 3R+ (3R plus hemodynamically-unstable humoral rejection) (p=0.003). However, when we studied within-subject effects of sST2 using a mixed model, the sST2 level according to the predefined time point was not different according to the presence of significant rejection (p for interaction=0.94).
Thirty percent of heart transplant (HTx) recipients experience a rejection episode during the first year of HTx.1) Currently, periodic endomyocardial biopsy is the standard method for the surveillance of acute allograft rejection during the first 6 to 12 months after HTx (Level of recommendation IIa).2) According to the representative example of the biopsy schedule described in the guideline, a patient needs repeated endomyocardial biopsy for a total of 16 times during the first year after HTx.2) However, endomyocardial biopsy is an invasive procedure that requires the patient's hospitalization, and may also be accompanied by harmful complications such as traumatic tricuspid regurgitation. The patients, especially those with higher numbers of endomyocardial biopsy, have an increased risk of severe tricuspid regurgitation.3) The incidence of tricuspid regurgitation after HTx was not rare (7-24%),4) and tricuspid regurgitation of more than moderate degree is associated with worse outcome after HTx.5) Furthermore, the recent advance of immunosuppressive therapy has lowered the incidence of rejection episodes requiring additional intensive immunosuppressive treatment. According to the 2012 registry of the International Society for Heart and Lung Transplantation (ISHLT) data, more than 80 percent of endomyocardial biopsy episodes were enough to be observed without further intensive immunosuppressive therapy.1)
There has been an effort to predict acute allograft rejection noninvasively using various biomarkers. Repeated measurement of N-terminal pro-B-type natriuretic peptide (NT-proBNP) or C-reactive protein (CRP) has been reported to be ineffective in predicting acute cellular rejection.6) Meanwhile, high-sensitivity cardiac troponin I (hs-TnI) showed promising results with good correlation with acute cellular rejection.7)8) However, significant overlap of hs-TnI between two groups with or without acute allograft rejection as well as conflicting data of cardiac troponin T (TnT) prevents clinicians from adopting biomarkers as a full substitute for endomyocardial biopsy.6)7)8)
Soluble ST2 (sST2) is a novel cardiovascular marker associated with cardiac hypertrophy, fibrosis, and ventricular dysfunction.9) In the patients with heart failure or acute coronary syndromes, sST2 is a well-known powerful predictor for cardiovascular events.9)10)11) Even in subjects without structural heart disease, a higher level of sST2 was also associated with increased risk of death and heart failure events.12) Furthermore, sST2 has been reported to be associated with the severity of inflammation of cardiomyocytes in acute lymphocytic myocarditis.13) Therefore, in the present study, we investigated the possibility of using sST2 as a non-invasive marker to predict acute allograft rejection after HTx.
Sixty-seven cases of HTx in Samsung Medical Center from September 2006 to August 2014 were included in this study. All of them agreed to provide their blood samples collected at the time of endomyocardial biopsy for the research with an informed consent form. The patients who did not agree were excluded. A total of 494 stored blood samples of 67 HTx cases were analyzed. The patients' clinical and laboratory findings were investigated retrospectively by reviewing the medical charts. The study protocol was approved by the Institutional Review Board of our institute (2014-12-111).
Endomyocardial biopsy was repeated based on the predefined protocol after HTx for the surveillance of acute allograft rejection in our center. In the early periods of the study, endomyocardial biopsy was performed at 2, 4, 8, 12, and 18 weeks, and 6, 9, 12, 18, and 24 months after HTx. In the later periods of the study beginning from August 2011, the routine surveillance beyond the first year of HTx was omitted. Since August 2011, the patients without evidence of allograft rejection at one year after the transplant did not undergo further endomyocardial biopsy routinely. Meanwhile, when HTx recipients experienced new-onset symptoms suggesting heart failure (dyspnea, fatigue, or syncope, etc.) without any explainable causes, an additional endomyocardial biopsy schedule was arranged at the time of symptoms. When significant rejection (≥ grade 2R) was detected pathologically in a biopsy specimen, follow-up biopsy was performed obligatorily 2 to 4 weeks after intensive immunosuppressive treatment. Endomyocardial biopsy was performed via a right internal jugular vein approach, and 5 to 7 specimens were acquired from the right ventricle each time.
The definition of acute allograft rejection follows the ISHLT guideline (0R to 3R).14) In this study, "any rejection" was defined as grading 1R or higher, and "significant rejection" was defined as a rejection grade of 2R or 3R. Additionally, sudden events of hemodynamic instability without any evidence of coronary ischemia were also included in the "significant rejection" grouping. Pathologically confirmed humoral rejection without hemodynamic significance was not considered as significant rejection.
All patients diagnosed with significant rejection were prescribed intensive immunosuppressive therapy including steroid pulse therapy. The protocol using steroid pulse in our center was comprised of 1000 mg of methylprednisolone every 24 hours for 3 days, and then administration of 1 mg/kg of prednisone per day for 3 days. After this was performed, a daily dose of prednisone was tapered by 5 mg every 3 days to reach a dose of 5-7.5 mg per day. In only one case, in which the patient had a body weight below 35 kg, was a lower dose of steroid used (500 mg of methylprednisolone once a day for 3 days) instead of 1000 mg of methylprednisolone.
If the patients were hemodynamically stable, a high dose of steroid was given only after the identification of pathologically significant rejection from a biopsy specimen. In those cases, the time interval between endomyocardial biopsy and intensive immunosuppressive therapy is 2-4 days. When HTx recipients were hemodynamically unstable, steroid pulse therapy was begun immediately after endomyocardial biopsy before the confirmation of pathological findings. If the biopsy specimen revealed acute humoral rejection by C4d special staining, rituximab of 375 mg/m2 of body surface area was administered every week for a period of 2-4 weeks. In some ISHLT 2R grade cases, steroid pulse therapy could be substituted by increasing the dose of mycophenolate from 1-1.5 g/day to 2 g/day. This kind of practice was allowed in the limited number of 2R cases that were stable without any symptoms. The patients taking higher mycophenolate as an intensive immunosuppressive therapy for the allograft rejection obligatorily had repeated endomyocardial biopsy after 2-4 weeks. If the repeated biopsy still showed significant rejection, steroid pulse therapy was performed right after the verification of significant rejection.
Blood samples were obtained by venipuncture at the time of endomyocardial biopsy and collected in a heparin tube. After centrifugation, plasma samples were stored at -80℃ in a refrigerator until analyzed. Blood samples were exposed to one freeze-thaw cycle before analysis. The sST2 levels were measured by personnel who were blinded to the clinical status of the patients, and were later matched with the medical information for each case. Serum sST2 concentration was measured by enzymelinked immunosorbent assay (ELISA) using Presage® ST2 (Critical Diagnostics, San Diego, CA, USA).
Data are expressed as frequencies, means±standard deviations or median values with interquartile ranges. The presence of normal distribution in each variable was investigated with a Kolmogorov-Smirnov test. Because the sST2 levels did not follow normal distribution, the correlation between sST2 levels and other continuous variables including age, white blood cell (WBC) counts, lymphocyte counts, the level of serum creatinine, C-reactive protein (CRP), cTnI and NT-proBNP were tested by Spearman's correlation test. To identify the independent correlates with sST2, a multiple linear regression analysis was performed using statistically significant variables from a univariate Spearman's correlation test. Consequently, WBC counts, lymphocyte counts, serum creatinine, cTnI, NT-proBNP, and time after HTx were included in the multiple linear regression analysis. sST2 levels according to rejection grade were compared using a Mann-Whitney test or Kruskal-Wallis test where appropriate. The p value was corrected by multiplying by 6 after the Kruskal-Wallis test based on the Bonferroni principle to control the problem brought by multiple comparisons. To evaluate changes of sST2 at the specific times in each patient, one-way repeated measured analysis of variance was conducted. The association between sST2 and the presence of rejection was evaluated with repeated measures analysis using mixed modeling with sST2 as an outcome. When the patients had two episodes of significant rejection, first rejection episodes were chosen for within-subject analysis. Because two patients had significant rejection twice, twenty cases with significant rejection and measured sST2 were used in within-subject analysis excluding the repeated episodes in the two patients. In the patients with significant rejection, sST2 and NT-proBNP levels were compared with the Friedman test. A two-tailed p value of less than 0.05 was considered statistically significant. Statistical analyses were performed with statistical package IBM SPSS Statistics 20.0 software (IBM Inc., Chicago, IL, USA).
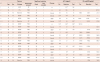
Sixty-seven HTx cases from 65 patients and their 494 blood samples were examined in this study. Among the 67 cases of HTx, 4 (6.0%) cases were retransplantation, and the other 63 (94.0%) cases were de novo HTx. Their mean age at HTx was 45.5±16.8 years, and 41 cases (61.2%) were male. Dilated cardiomyopathy was the most common etiology of heart failure (41 cases, 61.1%), followed by 7 cases of ischemic cardiomyopathy (10.4%), 6 cases of hypertrophic cardiomyopathy (9.0%), and 6 cases of valvular heart disease (9.0%). Other causes of heart failure included 4 cases of allograft rejection of a previously transplanted heart (6.0%), 1 case of myocarditis, 1 case of refractory ventricular tachycardia and 1 case of chemotherapy-induced cardiomyopathy. Initial immunosuppressive therapy included steroid in 67 cases (100%), cyclosporine in 21 cases (31.3%), tacrolimus in 46 cases (68.7%), and mycophenolate in 52 cases (77.6%). The median follow-up duration after HTx was 25.4 (14.7-54.8) months, and the number of repetitive endomyocardial biopsies per case is 7.4±1.9. Donor information was available in only 34 cases. The mean age of donors was 38.0±11.9 years, and 25 (73.5%) cases were male. The ischemic time before transplant was 184.0±55.8 minutes. Data regarding the characteristics of donors and recipients are summarized in Table 1.
The median value of sST2 in all 494 blood samples was 32.0 (18.8-82.0) ng/mL. The level of sST2 was positively correlated with WBC counts (r=0.50, p<0.001) as well as the level of cTnI (r=0.53, p<0.001) or NT-proBNP (r=0.61, p<0.001), and negatively correlated with time after HTx (r=-0.65, p<0.001) and lymphocyte counts (r=-0.44, p<0.001) (Table 2, Fig. 1 and 2A). Meanwhile, serum creatinine level showed only weak association with sST2 (r=-0.09, p=0.040). sST2 showed no statistical correlation with patients' age, CRP level or left ventricular ejection fraction (LVEF) measured using echocardiography. From multiple linear regression analysis, WBC counts, lymphocyte counts, cTnI and NT-proBNP remained as independent variables associated with sST2 (all p<0.001) with R2 value of 0.54 of the model (p<0.001).
When we selected sST2 at a specific time point after HTx (0.5, 1, 2, 3, 6, 9, and 12 months) in accordance with the predefined biopsy protocol, 381 samples in 67 HTx cases were available. sST2 levels at each time point were 155±12, 116±12, 46±7, 34±4, 31±4, 21±2 and 19±2 ng/mL, respectively (p<0.001) (Fig. 2B).
Of the entire population of 494 samples, 166 (33.6%) and 25 (5.1%) samples were matched with pathologic results showing any rejection and significant rejection, respectively; 328 (66.4%) samples of 0R, 141 (28.5%) samples of 1R, 19 (3.8%) samples of 2R, 3 (0.6%) samples of 3R and 3 (0.6%) samples of hemodynamically unstable humoral rejection. The ST2 level was statistically different according to the grades of acute rejection (36 [19-98], 28 [18-62], 15 [16-37], and 191 [85-343] ng/mL, in rejection grades of 0R, 1R, 2R, and 3R+ [3R plus hemodynamically unstable humoral rejection], respectively p=0.003) (Fig. 3A). The median value of sST2 was found to be different only between the 2R and 3R+ groups (corrected p=0.038). When sST2 was dichotomously analyzed according to the presence of significant rejection, there was no significant difference (32 [19-81] and 27 [16-94] ng/mL, p=0.72) (Fig. 3B). When the same analysis was performed divided by pre-and post-90 days after HTx, the sST2 level was not different statistically; pre-90 days (93 [47-155], 63 [30-132], 96 [82-110], and 105 [221-337] ng/mL, consecutively 0R to 3R+, p=0.09) and post-90 days (23 [15-34], 14 [20-28], 19 [15-31], and 191 [65-319] ng/mL, consecutively 0R to 3R+, p=0.052) (Fig. 4)
A total of 58 (86.7%) HTx patients experienced any acute allograft rejection first at 1.8 (0.4-3.4) months after HTx. Among them, first significant allograft rejection occurred in 20 (29.9%) cases at 4.0 (2.0-9.0) months after HTx. The baseline clinical characteristics of the two groups with or without significant rejection were not significantly different for recipient age, etiology of heart failure or initial immunosuppressive agents (Supplementary Table 1 in the online-only Data Supplement). There was only a higher tendency of second HTx in the group with significant rejection (3 [15%] vs. 1 [2.1%], p=0.08). When we studied within-subject effects of sST2 using a mixed model, the sST2 level according to the predefined time point was not different according to the presence of significant rejection (p for interaction=0.94). The result was the same when we selected cases only after 90 days of HTx (p for interaction=0.74). The level of sST2 before, at the time of, and after treatment of acute significant rejection, were available in 16, 18 and 17 patients among 20 cases experiencing significant rejection. Overall, sST2 at the pre- and post-rejection periods were not different statistically (32 [19-57], 24 [12-45], and 18 [15-50] ng/mL, before, at the time of, and after treatment of acute significant rejection, respectively, p=0.87) (Fig. 5A). The change in sST2 levels were also analyzed after categorization according to postoperative days; ≤90 days (Fig. 5B) and >90 days (Fig. 5C). There were no statistical difference in sST2 levels at the pre- and post-rejection periods in the early postoperative period (109 [74-173], 74 [30-173], and 31 [17-213] ng/mL, p=0.31) or late postoperative period (19 [14-31], 29 [12-32], and 50 [17-107] ng/mL, p=0.16). When we drew lines connecting the dots belonging to the same individual, the level of sST2 was not consistently decreased after the treatment of rejection, regardless of pathological improvement. Similarly, NT-proBNP showed no statistical difference according to time frame of significant rejection (770 [405-6435], 1683 [268-6882], and 827 [246-1195] pg/mL, p=0.51, respectively).
Detailed information for 20 cases with significant rejection are presented in Table 3. In a large portion of cases (11/20, 55.0%), the patients were treated with steroid pulse therapy. Among them, only one case (case #10) failed to recover and needed retransplantation. Among 6 cases treated with increasing doses of mycophenolate, one case (case #17) sustained significant rejection on follow-up biopsy and had subsequent steroid pulse therapy. Among 20 cases with significant rejection, 5 (29.4%) cases at pre-rejection, 10 (55.6%) cases at rejection, and 8 (40.0%) cases at the postrejection period showed sST2> two standard deviations at the same time point after HTx, the values of which were elicited from all 381 samples. Those cases are marked with asterics in Table 3.
The sST2 level after HTx was correlated with time after transplant, WBC count, lymphocytes count, cTnI and NT-pro BNP. However, correlations with pathologically confirmed ISHLT rejection score were not observed after control of the time after HTx. Many cases showing significant rejection were not accompanied by significant elevation in sST2 above two standard deviations of the same time point after HTx.
Noninvasive methods to detect allograft rejection after HTx using biomarkers have been studied several times. Measurement of NT-proBNP, TnT, CRP, or combinations of NT-proBNP and CRP failed to prove clinical usefulness in predicting acute allograft rejection after HTx.6)15) Battes et al. studied NT-proBNP or CRP using 1136 blood samples taken at the time of endomyocardial biopsies in 77 HTx cases.6) The level of NT-pro BNP and CRP were high immediately after the surgery and decreased to reach steady status at 12 weeks post-transplantation. However, repeated measurement of NT-pro BNP or CRP was ineffective in predicting acute cellular rejection both in the early periods and late periods after HTx. Meanwhile, high-sensitivity cardiac hs-TnI has been reported to have good correlation with acute cellular rejection.7)8) Patel et al.7) analyzed 418 serum samples of 35 HTx recipients and reported that the median value of hs-TnI was significantly high in the group with acute rejection, and that a cutoff point 0.015 ng/mL of cTnI could discriminate acute rejection with 94% sensitivity and a 99% negative predictive value. However, significant overlap was noted when hs-TnI was re-categorized by ISHLT grade. Similarly, in the recent study using 252 samples in 59 HTx cases, the absolute value of hs-TnI was not found to be different according to the presence of acute rejection.8) Although the median value of cTnI in the samples with acute cellular rejection was higher than the samples without acute rejection, a statistical difference was not observed. Reflecting all these clinical data, current guidelines recommend that routine noninvasive testing modalities including cardiac troponin I or T cannot substitute endomyocardial biopsy in adult HTx recipients (Level of recommendation III).2)
The role of sST2 as a biomarker to predict acute rejection after HTx has been investigated previously.16)17) Pascual-Figal et al.16) reported that sST2 levels were increased as compared with the pre-rejection period, and decreased again after treatment of acute rejection. However, they did not include the patients without acute rejection after HTx. Instead, the samples before and after rejection were utilized as a control group. In our study, both groups with or without rejection were included, and the data of the patients with rejection were compared with those of the patients without rejection. In the present study, a statistical difference was observed in the sST2 level according to the grades of the allograft rejection. However, correcting for confounding factors of the time after HTx, a statistical difference was not found. More recently, Mathews et al. reported that a higher level of sST2 (>600 pg/mL) could discriminate graft rejection with an area under the curve of 0.72±0.05 in pediatric HTx patients.17) However, they had higher rates of rejection events, and included a large proportion of acute humoral rejection among the significant rejection group. Similarly in our study, the level of antibody-mediated rejection was higher than others (#1, 2, and 7 in Table 3). Over 40% of patients (especially cases with acute cellular rejection) maintained sST2 levels in the range of 2 standard deviations calculated by the patients without acute rejection. On the other hand, sST2 can be affected by other cardiovascular and inflammatory conditions. As the IL-33/ST2 signaling pathway also involves T helper type 2 cell differentiation,18) it is not unusual that sST2 was higher in the cases with systemic infection or inflammation.19) The correlation of sST2 level and WBC/lymphocyte counts that appeared in our study also supports the possible correlation between inflammation and sST2 levels. Accordingly, sST2 was reported to be increased in chronic obstructive lung disease, asthma, pulmonary embolism, pulmonary hypertension, and alcohol abuse in other previous studies.19) Some extreme cases of sST2 levels in our data (arrows in Fig. 3B) also reflected critical events that occurred within several days; 1) generalized seizure suspected to have resulted from posterior reversible encephalopathy syndrome, 2) ischemic injury that appeared in endomyocardial biopsy, and 3) septic shock two days after endomyocardial biopsy. Because HTx recipients are susceptible to complications by multiple comorbidities in the early periods of HTx, sST2 is expected to have a limited role in predicating acute rejection specifically.
There are several limitations in this study. First, as a retrospective study, not all of the included patients have consecutive samples to present sequential change in sST2 after HTx, and there were missing values at certain time points after HTx. Nonetheless, we included 67 HTx cases with 494 samples; these numbers are quite comparable to those of previous retrospective studies.6)7)8)15)16) Second, because the presence of acute rejection was detected by endomyocardial biopsy surveillance, the follow-up duration of the included patients had limited time duration of 1-2 years after HTx. Hence, development of chronic vasculopathy or overall long-term cardiovascular mortality after HTx cannot be investigated. Like the general population without cardiovascular disease,12) sST2 may be associated with long-term cardiovascular outcome rather than acute allograft rejection developed in the early periods after HTx. Further studies are needed to confirm these possibilities. Additionally, the number of acute rejection cases was too small to understand the role of certain biomarkers fully; 20 patients with 22 blood samples (29.9% of total patients and 4.5% in total blood samples), even though the incidence rate was quite comparable with the rates of previous reports (37% of the patients).7) A larger number of subjects would definitely be required to obtain an adequate number of acute rejection episodes.
Although sST2 is known as a promising predictor for cardiovascular events, its role in HTx patients in predicting acute allograft rejection seems to be limited. Further prospective studies including larger populations with longer follow-up duration are needed in order to figure out the further clinical implications of sST2 in HTx recipients.
Figures and Tables
Fig. 1
Scattered plots showing correlation of sST2 with other continuous variables. (A) WBC count, (B) lymphocytes count, (C) cardiac troponin I (cTnI), and (D) NT-proBNP. WBC: white blood cell, NT-proBNP: N-terminal pro-B-type natriuretic peptide.

Fig. 2
Scatter plots of sST2 values according to the time after heart transplant. (A) sST2 measured in entire population of 494 blood samples (B) sST2 measured in 381 samples at the specific time point after heart transplant (0.5, 1, 2, 3, 6, 9, and 12 months). Median value and interquartile range of sST2 are presented as horizontal lines in whisker form. Some extreme cases of sST2 levels (arrows in Fig. 2B) reflected critical events other than acute allograft rejection that occurred within several days; 1) generalized seizure suspected as posterior reversible encephalopathy syndrome (PRES), 2) ischemic injury noted in endomyocardial biopsy, and 3) septic shock.

Fig. 3
Scattered plots of sST2 grouped by the rejection grades of concomitant endomyocardial biopsy. (A) sST2 categorized by groups according to International Society of Heart and Lung Transplant (ISHLT) rejection score. (B) sST2 categorized by the presence of significant rejection. Median value of sST2 in each group is marked with a horizontal line.

Fig. 4
Scatter plots of sST2 grouped by the pathologic grades of concomitant endomyocardial biopsy. (A) early (≤90 days) and (B) late (>90 days) periods after heart transplant. Median value of sST2 in each group is marked with a horizontal line. ISHLT: International Society of Heart and Lung Transplant.

Fig. 5
Scattered plots of sST2 measured at pre-rejection, at the time of rejection, and after a treatment of significant rejection. (A) Overall patients. (B) Early (≤90 days) and (C) later (>90 days) postoperative days. Measurement values of each individual case were connected by a line.

Table 1
Baseline characteristics of study cases (n=67)

Table 2
Correlates with sST2 in entire population of samples (N=494)

Table 3
Case summaries of the subjects having significant rejection after heart transplant
*Indicates sST2 values above 2 standard deviations derived from entire population of all 494 blood samples at the same time point. F: female, M: male, ICMP: ischemic cardiomyopathy, CTx: chemotherapy induced cardiomyopathy, DCMP: dilated cardiomyopathy, HCMP: hypertrophic cardiomyopathy, P: prednisolone, M: mycophenolate, C: cyclosporine, K: tacrolimus, H: humoral rejection, R: rituximab, MMF: increasing dose of mycophenolate to 2 g/day
Acknowledgments
This study was supported by the fund from the Korean Society of Cardiology (201402-02).
References
1. Stehlik J, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: 29th official adult heart transplant report--2012. J Heart Lung Transplant. 2012; 31:1052–1064.
2. Costanzo MR, Dipchand A, Starling R, et al. The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. J Heart Lung Transplant. 2010; 29:914–956.
3. Nguyen V, Cantarovich M, Cecere R, Giannetti N. Tricuspid regurgitation after cardiac transplantation: how many biopsies are too many? J Heart Lung Transplant. 2005; 24:7 Suppl. S227–S231.
4. Wong RC, Abrahams Z, Hanna M, et al. Tricuspid regurgitation after cardiac transplantation: an old problem revisited. J Heart Lung Transplant. 2008; 27:247–252.
5. Marelli D, Esmailian F, Wong SY, et al. Tricuspid valve regurgitation after heart transplantation. J Thorac Cardiovasc Surg. 2009; 137:1557–1559.
6. Battes LC, Caliskan K, Rizopoulos D, et al. Repeated measurements of NT-pro-B-type natriuretic peptide, troponin T or C-reactive protein do not predict future allograft rejection in heart transplant recipients. Transplantation. 2015; 99:580–585.
7. Patel PC, Hill DA, Ayers CR, et al. High-sensitivity cardiac troponin I assay to screen for acute rejection in patients with heart transplant. Circ Heart Fail. 2014; 7:463–469.
8. Ahn KT, Choi JO, Lee GY, Park HD, Jeon ES. Usefulness of high-sensitivity troponin I for the monitoring of subclinical acute cellular rejection after cardiac transplantation. Transplant Proc. 2015; 47:504–510.
9. Januzzi JL Jr. ST2 as a cardiovascular risk biomarker: from the bench to the bedside. J Cardiovasc Transl Res. 2013; 6:493–500.
10. Januzzi JL Jr, Rehman S, Mueller T, van Kimmenade RR, Lloyd-Jones DM. Importance of biomarkers for long-term mortality prediction in acutely dyspneic patients. Clin Chem. 2010; 56:1814–1821.
11. Shimpo M, Morrow DA, Weinberg EO, et al. Serum levels of the interleukin-1 receptor family member ST2 predict mortality and clinical outcome in acute myocardial infarction. Circulation. 2004; 109:2186–2190.
12. Wang TJ, Wollert KC, Larson MG, et al. Prognostic utility of novel biomarkers of cardiovascular stress: the Framingham Heart Study. Circulation. 2012; 126:1596–1604.
13. Kim BS, Jeon ES. Soluble ST2; predictive biomarkers of clinical presentation and mechanical circulation support in fulminant myocarditis. Korean Circ J. 2014; 322:Abstract.
14. Stewart S, Winters GL, Fishbein MC, et al. Revision of the 1990 working formulation for the standardization of nomenclature in the diagnosis of heart rejection. J Heart Lung Transplant. 2005; 24:1710–1720.
15. Arora S, Gullestad L, Wergeland R, et al. Probrain natriuretic peptide and C-reactive protein as markers of acute rejection, allograft vasculopathy, and mortality in heart transplantation. Transplantation. 2007; 83:1308–1315.
16. Pascual-Figal DA, Garrido IP, Blanco R, et al. Soluble ST2 is a marker for acute cardiac allograft rejection. Ann Thorac Surg. 2011; 92:2118–2124.
17. Mathews LR, Lott JM, Isse K, et al. Elevated ST2 distinguishes incidences of pediatric heart and small bowel transplant rejection. Am J Transplant. 2016; 16:938–950.
18. Kakkar R, Lee RT. The IL-33/ST2 pathway: therapeutic target and novel biomarker. Nat Rev Drug Discov. 2008; 7:827–840.
19. Ciccone MM, Cortese F, Gesualdo M, et al. A novel cardiac biomarker: ST2: a review. Molecules. 2013; 18:15314–15328.
Supplementary Materials
The online-only Data Supplement is available with article at http://dx.doi.org/10.4070/kcj.2016.46.6.811.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download