Abstract
Background and Objectives
Genetic influence on T-wave peak to End (Tpe) time in patients with a first anterior acute myocardial infarction (AMI) is uncertain. A polymorphism in the angiotensin-II type 1 receptor (AT1R) gene was discovered recently. The polymorphism consists of an A or C variant, given three different possible genotypes: AA, AC, CC. The purpose of this study was to determine the effects of polymorphism of the AT1R gene polymorphism on Tpe after a first anterior AMI.
Subjects and Methods
The subjects were 142 patients (110 men, 32 women, 58±13 years) with a first anterior AMI; ten patients were excluded from this study. Based on the polymorphism of the AT1R gene, they were classified into two groups: Group 1 (AA genotype) of 91 patients and group 2 (AC and CC genotype) of 41 patients. A 12-lead resting ECG was recorded at admission to the coronary care unit in patients with anterior AMI and were manually measured with a ruler. QTc, QTd, QTcd, Tpe, Tpe/QT parameters were measured.
The renin angiotensin system (RAS) plays an important role in the regulation of physiological and pathophysiological responses such as arterial vasoconstriction, blood pressure, aldosterone production, cardiac fibrosis, cardiac hypertrophy and renal function.1)2) RAS are involved in many cardiovascular diseases. The renin-angiotensin system comprises a cascade of enzymatic reactions, which results in the production of angiotensin (AT) II from the angiotensinogen substrate. The physiological effects of angiotensin II are mediated by a final common pathway, through angiotensin II binding to specific receptors located on the cell membrane.3) Two isoforms of endothelial receptors for angiotensin II are known so far: AT1 and AT2. Most of their physiological effects are mediated by the activation of AT1-subtype receptors which activates several intracellular signaling pathways in vascular smooth muscle cells, cardiomyocytes, and the cardiac conduction system.4) Although a number of polymorphisms of the angiotensin-II type 1 receptor (AT1R) gene have been identified, one of the most widely studied is an A–C substitution at position 1166 (A/C1166).5)
Chronic angiotensin II stimulation was found to produce QT prolongation, this potentially functional variant may modulate repolarization parameters. Ventricular repolarization abnormalities play an important role in the occurrence of arrhythmia.6) QT dispersion, a marker of repolarization homogeneity, is considered a predictor of sudden cardiac death and mortality in patients with myocardial infarction. Despite some controversial data about the positive predictive value of increased QT dispersion, this ECG marker appears to be a powerful tool for risk stratification in patients with impaired left ventricular function after myocardial infarction.6)
The T wave is generated by myocardial voltage gradients during the repolarization phase of cardiomyocyte action potentials. QT interval is a measure of repolarization duration, but may not reveal other changes during the repolarization process. T-wave peak to T-wave end (TPE) interval measures terminal repolarization, and has experimentally been linked to arrhythmogenic repolarization dispersion in the myocardium.7) Recently, several studies reported improved QT dispersion after angiotensin II receptor blockade or angiotensin converting enzyme (ACE) inhibitor therapy in patients with myocardial infarction (MI), suggesting that angiotensin II may directly or indirectly modulate QT dispersion. Thus, it has been suggested that improvement of repolarization homogeneity may be one mechanism that confers prognostic benefits by ACE inhibitors.8)
The identification of an association between lethal arrhythmias and common genetic variants may have an important role in assisting in primary prevention as well as improving utilization of life-saving therapies.8) There have been several association studies of the polymorphism of AT1R (A/C1166) in clinical endpoints, such as MI, hypertension, aortic stiffness, and LV mass. The goal of this study was to investigate the relationship between QTc, QTd, QTcd, Tpe, Tpe/QT and AT1R gene polymorphism in patients with a first anterior acute myocardial infarction (AMI).
We studied 142 consecutive patients (males 110, females 32; mean age 58±13 years, range 42-78) between March 2001 and December 2002, excluding ten patients. Patients were admitted to the coronary care unit with their first anterior AMI, defined as: (1) creatine kinase (CK) ≥210 IU and CK-myocardial band (MB) ≥20 IU; and (2) electrocardiographic evidence of MI (ST elevation ≥0.1 mV) in precordial leads (V1 through V6); and (3) typical chest pain. The patients were excluded if they fulfilled one of the following criteria: (1) history or ECG findings of previous MI, (2) previous coronary angioplasty or aortocoronary bypass surgery or (3) hypertensive or valvular heart disease (4) patients with a wide QRS complex with either right or left bundle branch block (5) atrial fibrillation. Ten patients were excluded because of ECG findings of previous MI (n=3), hypertensive heart disease (n=2), aortic stenosis (n=1), left bundle branch block (n=1), atrial fibrillation (n=3), leaving a total of 132 patients . The study protocol was approved by the departmental ethics committee, and informed consent was given by all patients. Based on the polymorphism of the AT1R gene, they were classified into two groups: Group 1 (AA genotype) of 91 patients and group 2 (AC and CC genotype) of 41 patients.
81% of patients were treated with thrombolytic therapy (streptokinase 1.5 million units/30 min or tissue type plasminogen activator 100 mg according to the accelerated protocol), acetylsalicylic acid-100 mg, beta-blocker (metoprolol 50-100 mg po) and intravenous nitroglycerin. ACE inhibitor (silazapril 2.5-5 mg) or angiotensin-receptor blocker (valsartan 80-160 mg) was added to the treatment in the first 24 h, if there was no contraindication.
Echocardiographic examinations were performed in all patients within 24 h of onset using a Vingmed CFM 800 system equipped with 3.5- and 2.5-MHz transducers. All examinations were performed using the parasternal longitudinal axis and apical 4-chamber windows in accordance with the recommendations of the American Echocardiography Committee.9) Using the parasternal long-axis view to assess the ventricular dimensions, the ejection fraction (EF) was calculated by the modified Simpson formula.
Genomic DNA was isolated from peripheral leukocytes using a commercially available kit. The A1166–C variant of AT1R was identified by polymerase chain reaction (PCR) and restriction fragment length polymorphism analysis, using the primers 5' -GCT TTG TCT TGT TGC AAA AGG-3' and 5'-CCC ACT CAA ACC TTT CAA-3' according to the PCR conditions described by Miller et al10) (Fig. 1).
All standard 12-lead ECGs were recorded at 25 mm/s speed and 10 mm/mv gain with Nihon Kohden ECG-9132K electrocardiograph (Nihon Kohden Corporation, Tokyo, Japan). A 12-lead resting ECG was recorded at admission in the coronary care unit for patients with an anterior AMI at the first six hours prior to the thrombolysis and then were manually measured with a ruler. All ECGs, were manually analyzed by 1 experienced cardiologist (Onder Ozturk) who was unaware of the clinical data. The QT interval was measured from the beginning of the QRS to the end of the T-wave. The end of the T-wave was defined as the point of return to the isoelectric line.11) In cases where the T-wave was interrupted by a U-wave, the end of the T-wave was defined as the nadir between the T- and U-waves. In instances where the T-wave could not be reliably determined due to extremely low voltage (<0.1 mV), measurement of QT interval was not established and consequently these leads were excluded from analysis. In order to exclude the effects of the heart rate (HR) on the QT interval, the QT interval was corrected according to the Bazett formula (QTc=QT/square root of RR interval). QTd was defined as the difference between the maximum and minimum QT intervals. TPE was measured with a ruler from the peak of the T-wave to its end;12) TPE was corrected for heart rate. The criteria to determine the endpoint of the T-wave were similar to the aforementioned criteria considered for the QT measurement.
Coronary angiograms were performed on 132 consecutive patients who were admitted to a coronary angiography laboratory with acute anterior MI. A cardiac catheterisation was performed according to routine procedures and coronary angiograms were recorded on CD, and analyzed.13) The coronary arteries were independently analyzed by 2 experienced cardiologists throughout the study who were unaware of the clinical and genetic data. Vessel diameters were assessed by caliper reading. CAD was defined as stenosis ≥50% in a major coronary artery or in a major branch. Severity of CAD was classified as 1-, 2-, or 3-vessel disease. The coronary artery disease extent score was defined by the number of coronary arteries exhibiting a stenosis >50% diameter reduction.
The data were analyzed statistically by computer software (SPSS version 11.0; Spss Inc., Chicago, IL, USA) and presented as mean±standard deviation. The genotypic distribution was tested by the Hardy-Weinberg equilibrium. A one-way ANOVA or chisquare test was used where appropriate to compare groups. A p value less than 0.05 was considered significant.
There were no significant differences between groups in terms of age, hypertension, hypercholesterolemia, other factors of coronary artery disease or peak CK-MB concentrations (p>0.05). At baseline, blood pressure levels and heart rates, LVEF were similar in all groups (p>0.05) (Table 1). There were no significant differences between groups with regard to the treatments (thrombolytic agent, beta-blocker, nitrate, ACE inhibitor agents) (Table 2) (p>0.05).
Genetic analysis was performed in all 132 patients. Analysis of AT1R polymorphism showed that 91 patients (68.9%) belonged to the AA genotype (Group 1), 41 (31.1%) to the AC and CC genotype (Group 2). The observed prevalence of the AT1R genotypes agreed with the frequencies predicted by the Hardy-Weinberg equilibrium (Table 3). Myocardial infarction patients with the AT1RG AC/CC genotype showed significantly longer QTc, QTd, QTcd, Tpe, Tpe/QT than myocardial infarction patients with the AT1R AA genotype (Table 4). Multivariate linear regression analysis in which AT1R gene polymorphism, gender, age, BMI, LVEF, and the presence of hypertension at baseline were included showing that the AT1R gene polymorphisms and LVEF were the only significant determinant (p<0.05) for the magnitude of QTc, QTd, QTcd, Tpe, Tpe/QT prolongation in the AT1R AC/CC genotype. Therefore, AT1R gene polymorphism and LVEF could significantly predict the magnitude of repolarization parameters (Table 5). Intraobserver variability of QTd is 3.2 ms and Tpe is 3.8 ms.
The coronary artery disease extent score was significantly greater in patients who have AGTR1 AC/CC genotype than AGTR1 AA genotypes. The coronary artery disease extent score was significantly higher in patients who have AT1R AC/CC genotypes (1.93±0.82) than AT1R AA genotype (1.41±0.58) (p<0.05). Residual ischemia was not significantly different between AT1R AC/CC genotypes (38%) and AT1R AA genotype (35%) (p>0.05).
Changes in QTd have been shown to follow the spontaneous or induced dynamicity of the pathological process in some cardiac diseases. Several factors have demonstrated to cause prolongation of QT parameters; for example, medications and myocardial ischemia have been reported as risk factors.14) In addition, LVMI and LV hypertrophy (LVH) were associated with a change in the QT interval and QTd in previous large cross-sectional studies.15) Prolongation of QT dispersion is frequently observed with left ventricular dilatation, low ejection fraction, and extensive cardiac scarring after myocardial infarction and is thought to indicate reduced repolarization homogeneity of a diseased heart.16)17)18) The identification of an association between lethal arrhythmias and common genetic variants may have an important role in assisting in primary prevention as well as improving utilization of life-saving therapies.8)19)
Our study shows that the AT1R AC/CC genotype conferred an increased risk of repolarization abnormality in a patient with AMI. Here we present data suggesting that genetic factors may also affect repolarization parameters. This data emphasizes the potential role of the renin angiotensin system in the morphological and electrophysiological remodelling process of the heart. Our results are consistent with the study of Anvari et al. Anvari et al. found that patients with coronary artery disease and left ventricular dysfunction carrying ACE D and AT1 C alleles are at an increased risk for developing malignant ventricular arrhythmias.8)
Previous studies demonstrated that the AT1R gene polymorphism may affect cardiac dilatation and hypertrophy in myocardial infarction or untreated hypertensive patients.20)21) Post myocardial infarction remodelling and left ventricular hypertrophy are known to reflect cellular hypertrophy and interstitial fibrosis, that subsequently may result in prolonged action potential duration, QT interval duration and QT dispersion, as well as an increased risk of malignant arrhythmias.7)22) Interestingly, Blanco RR et al. demonstrated that the AT1R-1166 CC genotype is associated with increased intracardiac defibrillator therapies in patients with chronic HF. These individuals with the AT1R-1166 CC genotype was subsequently associated with an increased risk for malignant ventricular arrhythmias, as recorded by the implantable cardioverter defibrillator.23) Based on our findings one could speculate that prolongation of QTc, QTd, QTcd, Tpe, Tpe/QT may be one mechanism causing such an association of malignant arrhythmias with a genetic variation of the renin angiotensin system.
The precise mechanism that links AT1R gene polymorphism and QT dispersion and Tpe are unclear. Also a possible physiological mechanism of the presence of a C allele in the AT1R gene polymorphism has not been clarified. Several G protein coupled receptors exhibit a down regulation due to increased agonist stimulation. Miller et.al have suggested that the C allele of the AT1R gene polymorphism is related to augmented angiotensin II activity.24) Enhanced local angiotensin formation may induce cellular hypertrophy and may modulate cardiac remodelling and fibrosis. This process ultimately may increase the action potential duration in some cardiac areas and, thus, prolong QT dispersion.7) This hypothesis is in agreement with data from pharmacological intervention studies demonstrating a decrease in QT dispersion after angiotensin II blockade or ACE inhibitor therapy.25)26)
There are, however, some limitations of this study that should be noted. As the AT1R CC genotype homozygotes are infrequent in the general population, large study groups are required to establish significant associations with diseased phenotypes. Lack of data on relation between the repolarization abnormalities (QTd, Tpe, etc.) and their clinical outcomes (ventricular arrhythmia or sudden cardiac death) are limitations of the present study.
In conclusion, our data provide evidence for an association of the AT1R gene polymorphism and the QTd, Tpe in patients with a first anterior acute myocardial infarction. Therefore, we suggested significantly prolonged QTd and Tpe in patients with AT1R AC/CC gene polymorphism. However, further studies are required to establish a relation.
Figures and Tables
Fig. 1
Gel electrophoresis of the AT1R polymorphism. 0: a DNA size marker (100bp),1: AA, 2: CC, 3: AA, 4: AC, 5: CC, 6: CC, 7: AA, 8: CC, 9: CC, 10: AA, 11: AA, 12: AC, 13: AA, 14: AC, 15: AA, 16: AA, 17: AA.

Table 1
General characteristics of the patients groups according to A/C1166 genotype
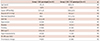
Table 2
Medical treatment of the patients groups according to A/C1166 genotype
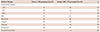
Table 3
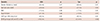
Angiotensin II type 1 receptor (A/C1166) genotype distribution and Allele frequency in patients
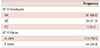
| Frequency | |
|---|---|
| AT1R Genotypes | |
| AA | 91 (68.9) |
| AC | 28 (21.2) |
| CC | 13 (9.9) |
| AT1R Alleles | |
| A allele | 210 (79.5) |
| C allele | 54 (20.4) |
Table 4
Electrocardiographic parameters data of the patients groups according to A/C1166 genotype
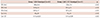
Table 5
Multiple linear regression analysis of factors with potential influence on QT dispersion and Tpe in myocardial infarction patients (n=132)
References
1. Laragh JH. Renin-angiotensin-aldosterone system for blood pressure and electrolyte homeostasis and its involvement in hypertension, in congestive heart failure and in associated cardiovascular damage (myocardial infarction and stroke). J Hum Hypertens. 1995; 9:385–390.
2. Aoki S, Mukae S, Itoh S, et al. The genetic factor in acute myocardial infarction with hypertension. Jpn Circ J. 2001; 65:621–626.
3. De Gasparo M, Catt KJ, Inagami T, Wright JW, Unger T. International Union of Pharmacology. XXIII. The angiotensin II receptors. Pharmacol Rev. 2000; 52:415–472.
4. Araújo MA, Menezes BS, Lourenço C, Cordeiro ER, Gatti RR, Goulart LR. The A1166C polymorphism of the angiotensin II type-1 receptor in acute myocardial infarction. Arq Bras Cardiol. 2004; 83:409–413.
5. Ozturk O, Ozturk U, Bilici A. The effect of angiotensin II type-1 receptor gene polymorphisms on doppler blood flow parameters of carotid and brachial arteries in patients with myocardial infarction. Echocardiography. 2006; 23:536–541.
6. Jeron A, Hengstenberg C, Engel S, et al. The D-allele of the ACE polymorphism is related to increased QT dispersion in 609 patients after myocardial infarction. Eur Heart J. 2001; 22:663–668.
7. Porthan K, Marjamaa A, Viitasalo M, et al. Relationship of common candidate gene variants to electrocardiographic T-wave peak to T-wave end interval and T-wave morphology parameters. Heart Rhythm. 2010; 7:898–903.
8. Anvari A, Türel Z, Schmidt A, et al. Angiotensin converting enzymeand angiotensin II receptor 1polymorphism in coronary disease and malignant ventricular arrhythmias. Cardiovasc Res. 1999; 43:879–883.
9. Hamon M, Amant C, Bauters C, et al. Association of angiotensin converting enzyme and angiotensin II type 1 receptor genotypes with left ventricular function and mass in patients with angiographically normal coronary arteries. Heart. 1997; 77:502–505.
10. Miller SA, Dykes DD, Polesky HF. Simple salting out procedure for extraction DNA from human nucleoted cells. Nucleic Acids Res. 1988; 16:1215–1219.
11. Malik M, Batchvarov VN. Measurement, interpretation and clinical potential of QT dispersion. J Am Coll Cardiol. 2000; 36:1749–1766.
12. Lin TH, Chiu HC, Su HM, et al. D-allele of ACE polymorphism is associated with increased magnitude of QT dispersion prolongation in elderly Chinese: 4-year follow-up study. Circ J. 2007; 71:39–45.
13. Jeunemaitre X, Ledru F, Battaglia S, et al. Genetic polymorphisms of the renin-angiotensin system and angiographic extent and severity of coronary artery disease: the CORGENE study. Hum Genet. 1997; 99:66–73.
14. Eslami V, Safi M, Taherkhani M, Adibi A, Movahed MR. Evaluation of QT, QT dispersion, and T-wave peak to end time changes after primary percutaneous coronaryintervention in patients presenting with acute T-elevation myocardial infarction. J Invasive Cardiol. 2013; 25:232–234.
15. Oikarinen L, Nieminen MS, Viitasalo M, et al. Relation of QT interval and QT dispersion to echocardiographic left ventricular hypertrophy and geometric pattern in hypertensive patients: The LIFE study The Losartan Intervention For Endpoint Reduction. J Hypertens. 2001; 19:1883–1891.
16. Day CP, McComb JM, Campbell RW. QT dispersion: an indication of arrhythmia risk in patients with long QT intervals. Br Heart J. 1990; 63:342–344.
17. Endoh Y, Kasanuki H, Ohnishi S, Uno M. Unsuitability of corrected QT dispersion as a marker for ventricular arrhythmias and cardiac sudden death after acute myocardial infarction. Jpn Circ J. 1999; 63:467–470.
18. Fujimoto S, Uemura S, Tomoda Y, et al. Effects of exercise training on the heart rate variability and QT dispersion of patients with acute myocardial infarction. Jpn Circ J. 1999; 63:577–582.
19. Takezako T, Zhang B, Serikawa T, Fan P, Nomoto J, Saku K. The D allele of the angiotensin-converting enzyme gene and reperfusioninduced ventricular arrhythmias in patients with acute myocardial infarction. Jpn Circ J. 2001; 65:603–609.
20. Gubaev KI, Nasibullin TR, Zakirova AN, Mustafina OE. Association of polymorphic markers I/D of gene ACE and A1166C of gene AT2R1 with ischemic chronic heart failure in the Russian and Tatar populations of Bashkortostan Republic. Genetika. 2006; 42:1712–1717.
21. Jin Y, Kuznetsova T, Thijs L, et al. Association of left ventricular mass with the AGTR1 A1166C polymorphism. Am J Hypertens. 2012; 25:472–478.
22. De Sutter J, Tavernier R, Van De Wiele C, et al. QT dispersion is not related to infarct size or inducibility in patients with coronary artery disease and life threatening ventricular arrhythmias. Heart. 1999; 81:533–538.
23. Blanco RR, Austin H, Vest RN, et al. Angiotensin receptor type 1 single nucleotide polymorphism 1166A/C is associated with malignant arrhythmias and altered circulating miR-155 levels in patients with chronic heart failure. J Card Fail. 2012; 18:717–723.
24. Miller JA, Thai K, Scholey JW. Angiotensin II type 1 receptor gene polymorphism predicts response to losartan and angiotensin II. Kidney Int. 1999; 56:2173–2180.
25. Spargias KS, Lindsay SJ, Hall AS, Cowan JC, Ball SG. Ramipril reduces QT dispersion in patients with acute myocardial infarction and heart failure. Am J Cardiol. 1999; 83:969–971.
26. Karpanou EA, Vyssoulis GP, Psichogios A, et al. Regression of left ventricular hypertrophy results in improvement of QT dispersion in patients with hypertension. Am Heart J. 1998; 136:765–768.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download