Abstract
Background and Objectives
To compare clinical outcomes of staged versus "one-time" percutaneous coronary intervention (PCI) in intermediate to very high-risk patients with non–ST-segment elevation acute coronary syndromes (NSTE-ACS) and multivessel coronary disease (MVD).
Subjects and Methods
1531 NSTE-ACS patients with multivessel PCI and meeting the criteria of intermediate to very high risk were screened from a prospectively registered database obtained from General Hospital of Shenyang Military Region between 2008 and 2012. They were categorized into "one-time" PCI (n=859) and staged PCI (n=672) according to intervention strategy. The primary outcomes included a 3-year major adverse cardiac event (MACE), a composite of cardiac death, myocardial infarction (MI), and target vessel revascularization.
Results
At 3 years, no significant differences in MACE (20.8% vs. 19.7%, p=0.608) and cardiac death/MI (7.1% vs. 9.1%, p=0.129) were observed between the two groups. After propensity score matching, there was no statistical significance in MACE (18.9% vs. 21.8%, p=0.249); whereas cardiac death/MI was significantly lower in the staged PCI group (7.0% vs.11.1%, p=0.033). Ninety-day landmark analysis showed that the staged PCI group had a lower 90-day incidence of MACE (1.2% vs. 3.3%, p= 0.037) and cardiac death/MI (0.7% vs. 2.6%, p=0.031). For the 90-day to 3-year follow-up period, the incidences of MACE (17.9% vs. 19.1%, p=0.641) and cardiac death/MI (6.3% vs. 8.7%, p=0.191) were similar in both groups.
Non-ST-segment elevation acute coronary syndromes (NSTE-ACS) are the most frequent manifestation of acute coronary syndromes (ACS). Its morbidity and mortality stays high and even equal to those of patients with ST-segment elevation myocardial infarction (STEMI) during long-term follow-up.1)2) Current guidelines2)3) propose risk stratification for tailoring treatment in patients with NSTE-ACS. In patients with intermediate- to very high-risk NSTE-ACS, routine invasive diagnostics and treatments are recommended. Multivessel coronary disease (MVD), a leading pathological foundation of intermediate to very high risk clinical manifestation, accounts for approximately 30–40% NSTE-ACS cohorts overall and is usually treated with invasive interventions.4) The American College of Cardiology/American Heart Association guidelines provide a class IIb recommendation that multivessel percutaneous coronary intervention (PCI), in contrast to culprit-only PCI, might be reasonable in NSTE-ACS patients undergoing PCI (Level of Evidence: B).3) This recommendation is based on reports of studies suggesting that multivessel PCI is superior to culprit vessel only PCI in terms of repeat revascularization.5)6)7)8) However, there is still uncertainty as to whether non-culprit lesions should be treated at the time of culprit-lesion PCI for NSTE-ACS.3) In the present study, we sought to examine clinical outcomes of "one-time" versus staged multivessel stenting in intermediate to very high-risk NSTE-ACS patients with MVD.
Between November 2008 and November 2012, a total of 12047 unselected patients who had undergone a PCI were prospectively registered in the PCI database of General Hospital of Shenyang Military Region. The database contained comprehensive information including clinical and angiographic characteristics, treatment strategies and clinical outcomes. Eligible patients had at least one intermediate to very high risk criteria with indication for invasive management defined by the 2015 European Society of Cardiology (ESC) guidelines for the management of NSTE-ACS2); 3 types of very high-risk criteria include recurrent or ongoing chest pain refractory to medical treatment, and recurrent dynamic ST-T wave changes particularly with intermittent ST-elevation and acute heart failure; 3 types of high-risk criteria include rise or fall in cardiac troponin compatible with myocardial infarction (MI), dynamic ST- or T-wave changes and Global Registry of Acute Coronary Events (GRACE) score >140; 7 intermediate-risk criteria include diabetes mellitus, renal insufficiency (Estimated glomerular filtration rate [eGFR] < 60 mL/min/1.73 m2), left ventricular ejection fraction (LVEF) <40% or congestive heart failure, early post-infarction angina, prior PCI, prior coronary artery bypass graft (CABG) and GRACE risk score>109 and <140. Exclusion criteria were patients who had chronic total occlusion; patients who had procedural failure (i.e., technical failure), including staged PCI patients who had procedural failure during the index PCI and scheduled for staging; patients who had cardiac shock, haemodynamic instability, mechanical complications of MI or malignant ventricular arrhythmia; patients who had renal dialysis or a eGFR <30 mL/min/1.73 m2; staged PCI patients who had any major complication during the index procedure; patients who had a planned staged PCI >60 days. Our final population included 1531 patients from the database having NSTE-ACS with multivessel PCI (Fig. 1).
All patients were given oral loading doses of aspirin (300 mg) and clopidogrel (300-600 mg) prior to PCI, unless they had already received antiplatelet medication. Interventional procedures were performed according to standard techniques and interventional strategies rested on the operators. The choice between complete or incomplete revascularization was also at operators' discretion. The culprit lesion was identified by operators usually based on each patient's electrocardiogram, angiographic imaging, echocardiogram and, if available, intravascular ultrasound (IVUS) and optical coherence tomography (OCT). A lesion was considered a culprit on angiography if at least two of the following morphological features suggestive of acute plaque rupture were present: intraluminal filling defects consistent with thrombus, plaque ulceration, plaque irregularity, dissection or impaired flow.2)9)10)11) After the procedure, the use of aspirin lifelong was advised and clopidogrel was prescribed for 12 months. The study was approved by the hospital ethics committee and all patients gave written informed consent.
Clinical follow-up was performed via telephone or at an outpatient visit at 30 days, 6 months, and 12 months after the index procedure and annually until 3 years after the index procedure. Follow-up angiography was recommended to all patients 6 to 12 months after the index procedure, and repeat revascularization was performed, if clinically indicated.
The primary outcome was the incidence of major adverse cardiac events (MACE), defined as the composite of cardiac death, MI and target vessel revascularization (TVR) during 3-year follow-up. Secondary outcomes included MACE components, the composite of cardiac death or MI, definite/probable stent thrombosis, and any repeat revascularization.
MVD was defined as the presence of a significant atherosclerotic coronary artery stenosis (≥70% diameter stenosis) or a ≥50% stenosis of the left main coronary artery (left main disease) with additional significant stenosis (≥70% diameter stenosis) of at least one other coronary artery assessed visually during coronary angiography.12) Staged PCI is defined as the planned PCI of non-infarct vessel(s) within 60 days of the index PCI. eGFR was calculated from serum creatinine (sCr) concentrations using the modified glomerular filtration rate estimating the equation for Chinese patients with chronic kidney disease: eGFR (mL/min/1.73 m2)=175×(sCr)-1.234×(age)-0.179×(0.79 if patient is female).13) Anemia was defined as hemoglobin less than 12 g/dL for men or less than 11 g/dL for women.14) Early invasive intervention was defined as a coronary angiography performed within 24 h of hospital admission.2) Delayed invasive intervention was defined as a coronary angiography performed more than 24 h of hospital admission. Technical success was defined as the ability to cross an occluded or stenosed segment and successfully open the artery (restoration of thrombolysis in myocardial infarction [TIMI] flow grade 3) with a residual stenosis ≤30% by visual analysis. Cardiac death was defined as death that could not be attributed to a non-cardiac etiology. MI was defined as third universal definition of MI presented by The Third Global MI Task Force.15) TVR was determined as any repeated PCI or CABG to treat a previously stented vessel. Complete revascularization was defined when no visually estimated stenosis ≥50% for the left main and no stenosis ≥70% for other major arteries and/or their major branches at discharge. Stent thrombosis was classified as definite and probable according to definitions proposed by the Academic Research Consortium.16)
Continuous variables were expressed as mean±standard deviation (SD), and categorical variables were expressed as number and/or percentages. For group comparisons, Pearson chi-square test or Fisher's exact test was used for categorical variables. Student's unpaired t-test or the Mann-Whitney rank-sum test, as appropriate, was used for continuous variables. To minimize the influence of confounders on outcome, we used propensity score matching analysis. Patients who underwent staged PCI were matched in a 1:1 ratio with patients who underwent a "one-time" PCI using the nearest neighbor matching, which were based on all available variables listed in Tables 1 and 2 except GRACE Score, IVUS used, OCT used, contrast volume, length of hospital, medication at discharge and dual antiplatelet therapy (DAPT) duration. A difference of <10% was regarded as acceptable. Time to event data with estimated event rates calculated by Kaplan-Meier method were compared with the log-rank test. In addition, we performed Kaplan-Meier analyses at the landmark periods of 0 to 90 days and 90 days to 3 years to evaluate the effect of revascularization strategy on clinical outcomes at different time periods. All statistical tests were 2-tailed, and statistical analyses were performed with SPSS Ver. 20 software (SPSS Inc., Chicago, IL, USA).
"One-time" PCI was performed in 56.1% (859/1531), and the remaining 43.9% (672/1531) had staged PCI (Of these, 80.7% [542/672] had staged non-culprit intervention during the same hospitalization and 19.3% [130/672] had planned staged non-culprit procedures after hospital discharge). The median delay of the staged PCI was 5 days (interquartile rang [IQR], 3-9 days). As noted in Tables 1 and 2, male, previous MI, triple-vessel disease, and current smoking were associated with more staging. The volume of contrast media utilized during the index procedure in the staged PCI group was smaller (200 mL [IQR, 150-220 mL] vs. 200 mL [IQR, 200-300 mL], p<0.001) though the total volume utilized in the initial procedure plus staged procedure was greater (400 mL [IQR, 310-500 mL] vs. 200 mL [IQR, 200-300 mL], p<0.001). Medications at discharge were similar between both groups. Most patients took dual antiplatelet therapy (DAPT), which was consistent with the standard recommendation. After propensity matching, there were no statistically significant differences in preselected variables between the two groups.
As noted in Table 3, Fig. 2A and Fig. 3A, MACE occurred in 132 patients (20.8%) in the staged group and 162 patients (19.7%) in the "one-time" group during 3-year follow-up (p=0.608). Rates of each component of 3-year cumulative MACE were similar between both groups. The estimated 3-year composite rate of cardiac death or MI was 7.1% in the staged PCI group compared with 9.1% in the "one-time" PCI group (p=0.129). In addition, no significant differences in the 3-year rates of any revascularization (22.3% vs. 18.6%, p= 0.083) and definite/probable stent thrombosis (1.3% vs. 1.9%, p=0.295) were observed.
After generating a propensity score, 420 of the 672 patients who underwent staged PCI were matched with a patient, respectively, who underwent a "one-time" PCI. There were no differences in preselected variables for the propensity matched subjects (Table 1, 2). As noted in Table 3, Fig. 2B and Fig. 3B, at 3 years, there were no differences in MACE (18.9% vs. 21.8%, p=0.249); whereas there was a significantly lower incidence of cardiac death or MI (7.0% vs. 11.1%, p=0.033). The risk for cardiac death in the staged PCI group tended to be lower (2.5% vs. 4.8%, p=0.067). Other clinical outcomes including MI (5.0% vs. 7.7%, p=0.162), TVR (14.9% vs. 14.5%, p=0.971), any revascularization (20.3% vs. 20.4%, p=0.888), and definite/probable stent thrombosis (1.2% vs. 2.2%, p=0.280) were not significantly different between the two study groups.
The results of the 90-day landmark analysis for propensity score matched patients were shown in Tables 3 and 4, Fig. 2D and Fig. 3D. The staged PCI group showed a lower 90-day incidence of MACE (1.2% vs. 3.3%, p=0.037), mainly due to a lower composite rate of cardiac death or MI (0.7% vs. 2.6%, p=0.031). The 90-day rates of MI did not differ significantly between the 2 study groups, but it presented a trend in favor of staged PCI (0.7% vs. 2.1%, p=0.081). For the 90-day to 3-year follow-up period, both the incidences of MACE (17.9% vs. 19.1%, p=0.641) and the composite of cardiac death or MI (6.3% vs. 8.7%, p=0.191) were similar between the two groups. Cardiac death, TVR, any revascularization and definite/probable stent thrombosis did not differ significangtly between the two groups at the landmark period of 0 to 90 days and 90 days to 3 years.
To our knowledge, this is the first study to examine the efficacy of staged versus "one-time" approach in intermediate to very high-risk NSTE-ACS patients with multivessel PCI. Main findings of this study were as follow: in intermediate to very high-risk NSTE-ACS patients with multivessel disease, staged PCI was associated with a lower composite rate of cardiac death or MI compared with "one-time" PCI strategy. This benefit of staged PCI was more apparent in the early period after procedures, rather than middle-late period.
Clinicians are often faced with the decision of whether to treat the nonculprit lesions during the index procedure or to treat it at a later time.17) Hannan et al. compared the "one-time" complete revascularization in the index admission versus PCI of the culprit lesion only with staged non-culprit PCI for complete revascularization in a subsequent admission among patients with NSTE-ACS and MVD.18) At 3 years, no significant difference in all-cause mortality was observed between the two groups. However, the staged PCI group did not include the patients who underwent a staged intervention during the same hospitalization. Furthermore, it is yet unknown whether it was different in all-cause mortality between the two groups after exclusions of low risk patients.
In the current observational study, the superiority of staged PCI strategy over "one-time" PCI strategy in terms of the composite of cardiac death or MI was presented, especially in the early period after PCI. There are some potential pitfalls of "one-time" multivessel PCI approach. First, NSTE-ACS patients are in a heightened thrombotic and inflammatory state.19)20)21)22) "One-time" multivessel PCI can lead to prolongation of procedure time, exposure to a higher radiation dose23) and larger volume of contrast agents during the index procedure compared to staged revascularization. This may result in an increased number of complications such as periprocedural MI or acute kidney injury as well as stent thrombosis.24)25) Moreover, patients with high/intermediate risks of NSTE-ACS are often in a poor clinical state or have concomitant comorbidities. PCI on the culprit lesion first and staged non-culprit PCI at a later date with optimal medical therapy usually results in the patient being stable and also allows clinicians to reassess the patient's clinical and angiographic states.
Risk stratification is essential for the clinical decision-making process in NSTE-ACS patients. With respect to outcomes, periprocedural complications of intervention, as well as the long-term ischemic risk, remain higher in high/intermediate risk NSTE-ACS than in low-risk NSTE-ACS patients.26)27)28)29)30) When choosing the optimal treatment strategy in the individual patient with NSTE-ACS and MVD, general patient condition and concomitant comorbidities have to be taken into account. However, the optimal strategy for the management of NSTE-ACS patients with poor clinical presentation and multivessel disease has not been well established. Therefore, our patient inclusion criteria, which were based on ESC guidelines, selected NSTE-ACS patients with intermediate- to very high-risk features.
Our study had several limitations. First, this was a retrospective analysis from a prospective single center registry. The decisions for one-time vs. staged PCI were not based on a randomization but at physicians' discretion, which resulted in obvious confounding and selection bias. Although we analyzed by adjusting many possible confounding factors, unmeasured confounding or selection bias might have influenced our findings. Second, in this study, all patients underwent PCI in the setting of antiplatelet therapy with clopidogrel. When the new antiplatelet agent ticagrelor is available, this finding deserves further investigation. Third, the relatively high frequency of angiography during the period between 6 to 12 months after the procedure could bias the MACE, especially TVR. However, this bias was limited, because the two groups had similar frequencies of follow-up angiography and because repeat intervention was guided by either recurrent angina or signs of ischemia that had progressed angiographically, even without angina based on invasive or noninvasive testing. Fourth, our data were collected before current practice guidelines2) were published. Therefore, timing of invasive strategies were not run according to current guidelines. Fifth, given the low absolute number of events at 90-day follow up in the propensity score matched cohort, our study was not powered to detect significant differences in cardiac death, MI, TVR and stent thrombosis at 90 days. Last, considering follow-up angiography and routine cardiac biomarkers surveillance was not mandatory, therefore the incidence of MI might have been underestimated.
Figures and Tables
Fig. 1
Patient flow diagram. PCI: percutaneous coronary intervention, STEMI: ST-segment elevation myocardial infarction, CAD: coronary artery disease, NSTE-ACS: non–ST-segment elevation acute coronary syndromes, eGFR: estimated glomerular filtration rate.

Fig. 2
Kaplan-Meier assessment of MACE for unadjusted (A) and propensity score matched (B) patients; 90-day landmark analysis of MACE for unadjusted (C) and propensity score matched (D) patients. MACE: major adverse cardiac events, PCI: percutaneous coronary intervention.

Fig. 3
Kaplan-Meier assessment for the composite of cardiac death or MI for unadjusted (A) and propensity score matched(B) patients; 90-day landmark analysis of the composite of cardiac death or MI for unadjusted (C) and propensity score matched (D) patients. PCI: percutaneous coronary intervention. MI: myocardial infarction.
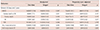
Table 1
Baseline characteristics
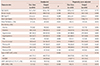
BMI: body mass index, PAD: peripheral arterial disease, MI: myocardial infarction, PCI: percutaneous coronary intervention, CVD: cerebrovascular disease, Hb: hemoglobin, NSTE-ACS: non–ST-segment elevation acute coronary syndromes, UA: unstable angina, NSTEMI: non-ST-segment elevation myocardial infarction, eGFR: estimated glomerular filtration rate, LVEF: Left ventricular ejection fraction
Table 2
Treatment and procedure related characteristics
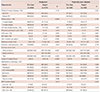
Table 3
90-day and 3-year outcomes for unadjusted and adjusted populations
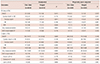
Table 4
Clinical outcomes from 90 days to 3 years after index PCI
References
1. Authors/Task Force members. Windecker S, Kolh P, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014; 35:2541–2619.
2. Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016; 37:267–315.
3. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 64:e139–e228.
4. Loscalzo J, Longo DL, Fauci AS, et al. Unstable angina and non-STelevation myocardial infarction. In : Cannon CP, editor. Harrison Cardiovascular Medicine. New York: McGraw-Hill Education;2013. p. 407–414.
5. Shishehbor MH, Lauer MS, Singh IM, et al. In unstable angina or non-ST-segment acute coronary syndrome, should patients with multivessel coronary artery disease undergo multivessel or culprit-only stenting? J Am Coll Cardiol. 2007; 49:849–854.
6. Kim MC, Jeong MH, Ahn Y, et al. What is optimal revascularization strategy in patients with multivessel coronary artery disease in non-ST-elevation myocardial infarction? Multivessel or culprit-only revascularization. Int J Cardiol. 2011; 153:148–153.
7. Brener SJ, Milford-Beland S, Roe MT, et al. Culprit-only or multivessel revascularization in patients with acute coronary syndromes: an American College of Cardiology National Cardiovascular Database Registry report. Am Heart J. 2008; 155:140–146.
8. Zapata GO, Lasave LI, Kozak F, et al. Culprit-only or multivessel percutaneous coronary stenting in patients with non-ST-segment elevation acute coronary syndromes: one-year follow-up. J Interv Cardiol. 2009; 22:329–335.
9. Ambrose JA, Winters SL, Stern A, et al. Angiographic morphology and the pathogenesis of unstable angina pectoris. J Am Coll Cardiol. 1985; 5:609–616.
10. Kerensky RA, Wade M, Deedwania P, Boden WE, Pepine CJ. Revisiting the culprit lesion in non-Q-wave myocardial infarction. Results from the VANQWISH trial angiographic core laboratory. J Am Coll Cardiol. 2002; 39:1456–1463.
11. Goldstein JA, Demetriou D, Grines CL, Pica M, Shoukfeh M, O'Neill WW. Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med. 2000; 343:915–922.
12. Luczak D, Majda W, Dabrowski R, et al. Prognostic importance of the extent of coronary revascularisation in patients with acute coronary syndromes and multivessel disease: one-year prospective follow-up. Kardiol Pol. 2015; 73:159–166.
13. Ma YC, Zuo L, Chen JH, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006; 17:2937–2944.
14. XH W, XF L. Diagnostics. 8th ed. Beijing: People's Medical Publishing House;2013.
15. Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012; 60:1581–1598.
16. Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007; 115:2344–2351.
17. Dangas GD, George JC, Weintraub W, Popma JJ. Timing of staged percutaneous coronary intervention in multivessel coronary artery disease. JACC Cardiovasc Interv. 2010; 3:1096–1099.
18. Hannan EL, Samadashvili Z, Walford G, et al. Staged versus one-time complete revascularization with percutaneous coronary intervention for multivessel coronary artery disease patients without ST-elevation myocardial infarction. Circ Cardiovasc Interv. 2013; 6:12–20.
19. Ohashi Y, Kawashima S, Mori T, et al. Soluble CD40 ligand and interleukin-6 in the coronary circulation after acute myocardial infarction. Int J Cardiol. 2006; 112:52–58.
20. Kereiakes DJ, Gurbel PA. Peri-procedural platelet function and platelet inhibition in percutaneous coronary intervention. JACC Cardiovasc Interv. 2008; 1:111–121.
21. Chan MY, Andreotti F, Becker RC. Hypercoagulable states in cardiovascular disease. Circulation. 2008; 118:2286–2297.
22. Brummel-Ziedins K, Undas A, Orfeo T, et al. Thrombin generation in acute coronary syndrome and stable coronary artery disease: dependence on plasma factor composition. J Thromb Haemost. 2008; 6:104–110.
23. Di Mario C, Mara S, Flavio A, et al. Single vs multivessel treatment during primary angioplasty: results of the multicentre randomised HEpacoat for cuLPrit or multivessel stenting for Acute Myocardial Infarction (HELP AMI) Study. Int J Cardiovasc Intervent. 2004; 6:128–133.
24. Gasior P, Desperak P, Gierlaszynska K, et al. Percutaneous coronary intervention in treatment of multivessel coronary artery disease in patients with non-ST-segment elevation acute coronary syndrome. Postepy Kardiol Interwencyjnej. 2013; 9:136–145.
25. Zimarino M, Curzen N, Cicchitti V, De Caterina R. The adequacy of myocardial revascularization in patients with multivessel coronary artery disease. Int J Cardiol. 2013; 168:1748–1757.
26. Jernberg T, Hasvold P, Henriksson M, Hjelm H, Thuresson M, Janzon M. Cardiovascular risk in post-myocardial infarction patients: nationwide real world data demonstrate the importance of a long-term perspective. Eur Heart J. 2015; 36:1163–1170.
27. Marso SP, McGuire DK. Coronary revascularization strategies in patients with diabetes and multivessel coronary artery disease: has the final chapter been written? J Am Coll Cardiol. 2014; 64:1198–1201.
28. Elbarouni B, Ismaeil N, Yan RT, et al. Temporal changes in the management and outcome of Canadian diabetic patients hospitalized for non-ST-elevation acute coronary syndromes. Am Heart J. 2011; 162:347–355.e1.
29. Abu-Assi E, Ferreira-Gonzalez I, Ribera A, et al. "Do GRACE (Global Registry of Acute Coronary events) risk scores still maintain their performance for predicting mortality in the era of contemporary management of acute coronary syndromes?". Am Heart J. 2010; 160:826–834.e1-3.
30. Reuter PG, Rouchy C, Cattan S, et al. Early invasive strategy in high-risk acute coronary syndrome without ST-segment elevation. The Sisca randomized trial. Int J Cardiol. 2015; 182:414–418.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download