Abstract
Total absence of superior vena cava (SVC) is a very rare anomaly, and the patient usually suffers from SVC syndrome or conduction disturbances. We report an asymptomatic 27 year-old male, with complete absence of SVC. Transthoracic echocardiography and computed tomography demonstrated the absence of SVC and other congenital cardiac anomalies, but the presence of prominent collateral vessels that allow a sufficient venous return.
Superior vena cava (SVC) drains blood from the head and upper extremities to the heart. When the blood flow becomes limited by extraluminal compression or intraluminal obstruction, SVC syndrome may occur. As SVC obstruction progresses, the blood pressure in the venous system increases and the collateral vessels dilate. The severity of symptoms is related to the speed and degree of SVC narrowing.1)
Bilateral absence of SVC is a rarely reported etiology of SVC syndrome, and it is often found with other congenital cardiac anomalies and/or conduction abnormalities.2) Herein, we report a case of a patient with complete absence of SVC, but without any sign of SVC syndrome and electrical disturbance.
A 27 year-old man was referred to our hospital for evaluation of chronic cough. He was previously healthy, and his only symptom was a one-year history of cough. He denied any neurologic, respiratory and cardiovascular symptoms. He was a current smoker, with 2.5 pack-year smoking history. His vital signs were normal and physical examination was unremarkable; there was no facial and upper extremity swelling, and the lung and heart sounds were normal. He also denied any family history of congenital anomaly of the cardiovascular system. No previous medical illnesses were reported, or any history of pediatric malignancy, central venous catheterization, or chronic infection.
In his initial visit to the hospital, he underwent a chest X-ray and non-contrast computed tomography (CT) scan; was no significant abnormality was seen in the lung parenchyma. Tortuous collateral vascular structure in the anterior mediastinum suggested the possibility of SVC obstruction, but the etiology of the SVC obstruction was unclear in these images. He later underwent a contrast CT scan at our institute, for further evaluation. CT showed no evidence of neoplasm, thrombus or fibrotic scar in the thoracic cavity. Interestingly, although the right and left brachiocephalic veins were present, the SVC was completely absent after the confluence of the brachiocephalic veins (Fig. 1, Fig. 2B, C). Instead, there were prominent collateral pathways such as azygos-hemiazygos, internal and external mammary thoracic, lateral thoracic collateral, pericardiophrenic, and caval-superficial-umbilical-portal pathways. (Fig. 2A, D, E, 3A and B). Contrary to complete absence of SVC, the inferior vena cava of this patient was intact (Fig. 2D). Both the transthoracic echocardiography and pulmonary function test showed unremarkable results. We planned a superior vena cavography, but the patient rejected any further evaluation.
Limitation of blood flow through the SVC can cause dyspnea, fullness of breathing, cough, hemoptysis, chest pain, swelling of head and upper extremities, headache, and even cerebral edema, which are clinically defined as the SVC syndrome. For evaluation of SVC abnormalities, although non-invasive CT scan is the initially preferred imaging modality nowadays,3) conventional venography still remains an important alternative when intervention is warranted.3)4)
The common etiologies for SVC syndrome include infectious diseases (e.g. syphilitic aortic aneurysm) and malignancies (e.g. lung cancer or lymphoma). With increasing use of central venous catheter and implantable cardiac devices, thrombosis in the central vein also becomes a prevalent cause of SVC syndrome.3) Since this patient denied any medical history that may have caused SVC obstruction along with the CT images, congenital agenesis of SVC was the more likely cause than secondary obliteration. As a shallow structure linked to the right atrium might be a trace of SVC (Fig. 1), however, we cannot completely exclude the possibility of chronic SVC obstruction.
Congenital absence of SVC is a rare cause of SVC syndrome. In previous reports,5)6) patients with an absence of the right SVC were almost always related with a persistence of left SVC. Complete absence of both SVC is very rare and usually accompanied by other congenital anomalies of the heart, including cardiac conduction system, or thoracic duct system.2)7)8) Most patients with complete absence of SVC complained of various symptoms and signs related to the accompanied abnormalities and SVC syndrome, with a varying degree of severity.9)
Cough is observed in half the patients with SVC obstruction. However, the patient had none of the other above mentioned symptoms; thus, it is less likely that cough is related to SVC obstruction.1)3)
The severity of the SVC syndrome is known to be dependent on the rapidity of SVC occlusion and the development of collateral vessels. In our case, the patient had no other anomalies or medical history, except for the absence of SVC. He also showed prominent collateral vessels, which might have started to develop in the fetal period. These well-developed collateral vessels allowed sufficient venous return and made the patient asymptomatic, even in the complete absence of bilateral SVC.
Figures and Tables
Fig. 1
Reconstructed computed tomography scan showed the absence of superior vena cava (SVC). After confluence of the brachiocephalic veins, the SVC was absent. RA: right atrium, Rt.BCV: right brachiocephalic vein.
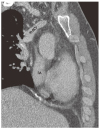
Fig. 2
(A-E) These coronal images were obtained from contrast computed tomography scan. Prominently dilated collateral vessels were observed. After confluence of left and right brachiocephalic veins, blood flow was no more visible. (C, D) Contrary to absence of SVC, blood from the IVC flows into the right atrium intact. Rt.PV: right pericardiphrenic vein, Lt.PV: left pericardiophrenic vein, RA: right atrium, Az: Azygos vein (*), IVC: inferior vena cava, LumbV: lumbar vein, SVC: superior vena cava.

Acknowledgments
We thank Dr. Eun Ju Chun, Department of Radiology, Seoul National University Bundang Hospital, Seongnam, South Korea, for assistance for investigation of images demonstrated in this article.
References
1. Wudel LJ Jr, Nesbitt JC. Superior vena cava syndrome. Curr Treat Options Oncol. 2001; 2:77–91.
2. Ylänen K, Poutanen T, Savikurki-Heikkilä P, Uotila J, Korppi M, Eerola A. Bilateral absence of the superior vena cava. Case Rep Cardiol. 2012; 2012:461040.
3. Wilson LD, Detterbeck FC, Yahalom J. Clinical practice. Superior vena cava syndrome with malignant causes. N Engl J Med. 2007; 356:1862–1869.
4. Wan JF, Bezjak A. Superior vena cava syndrome. Hematol Oncol Clin North Am. 2010; 24:501–513.
5. Bartram U, Van Praagh S, Levine JC, Hines M, Bensky AS, Van Praagh R. Absent right superior vena cava in visceroatrial situs solitus. Am J Cardiol. 1997; 80:175–183.
6. Lenox CC, Zuberbuhler JR, Park SC, et al. Absent right superior vena cava with persistent left superior vena cava: implications and management. Am J Cardiol. 1980; 45:117–122.
7. Romer S, Opgen-Rhein B, Chaoui R, Scheer I, Czernik C, Obladen M. Bilateral agenesis of the superior vena cava associated with congenital hydrothorax. Ultrasound Obstet Gynecol. 2006; 28:842–844.
8. Lee CY, Jan SL, Wang TM, Chi CS. Congenital chylothorax associated with isolated congenital hypoplastic superior caval vein: a case report. Acta paediatr. 2005; 94:1840–1843.
9. Saunders RN, Richens DR, Morris GK. Bilateral absence of the superior vena cava. Ann Thorac Surg. 2001; 71:2041–2043.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download