Abstract
Background and Objectives
A blood transfusion is almost inevitable in neonatal cardiac surgery. This study aimed to assess the feasibility of using autologous cord blood for a cardiopulmonary bypass (CPB) priming as an alternative to an allo-transfusion in neonatal cardiac surgery.
Subjects and Methods
From January 2012 to December 2014, cord blood had been collected during delivery after informed consent and was stored immediately into a blood bank. Eight neonatal patients had their own cord blood used for CPB priming during cardiac surgery.
Results
All patients underwent surgery for their complex congenital heart disease. The median age and body weight at surgery was 11 days (from 0 to 21 days) and 3.2 kg (from 2.2 to 3.7 kg). The median amount and hematocrit of collected cord blood was 72.5 mL (from 43 to 105 mL) and 48.7% (from 32.0 to 51.2%). The median preoperative hematocrit of neonates was 36.5% (from 31.0 to 45.0%); the median volume of CPB priming was 130 mL (From 120 to 140 mL). Seven out of eight patients did not need an allo-transfusion in CPB priming and only one neonate used 20 mL of packed red blood cells in CPB priming to obtain the target hematocrit.
Since comprehensive blood sparing strategies were proposed to minimize the requirement for blood transfusions that may increase the risks for postoperative complications, bloodless pediatric cardiac surgery has become widely accepted in many centers.1)2)3)4) Those strategies included a miniaturized bypass system, modified ultrafiltration, cell salvage, autologous blood donation and so forth.5) Nonetheless, transfusion-free neonatal cardiac surgery is still a challenge mainly because of the mismatch between the cardiopulmonary bypass (CPB) priming volume and a baby's blood volume. Thus, a new technique is needed for reducing transfusions during neonatal cardiac surgery. Recently usefulness of cord blood for an autologous transfusion was reported in newborns requiring cardiac or non-cardiac surgery.6)7)9) In addition, the improvement in fetal diagnosis of congenital heart disease (CHD) allows to plan for corrective surgeries within the neonatal period and to harvest autologous cord blood for use during surgery. However, clinical use of cord blood for transfusion purposes is still limited.
We aimed to assess the feasibility of using autologous cord blood for CPB priming in neonatal cardiac surgery.
Between January 2012 and December 2014, cord blood was harvested in 20 patients who had been prenatally diagnosed as having a complex congenital heart disease that would require cardiac surgery within the neonatal period. Informed consent was provided by their parents in all patients before harvest of cord blood. Eight patients whose cord blood was used during cardiac surgery were enrolled in the study. The institutional review board approved the study's protocol, and all procedures were performed in accordance with our institutional guidelines for the protection of patient confidentiality.
Immediately after delivery of the newborn, the cord was double clamped and cut as close as possible to the abdomen of the baby. The umbilical vein was punctured with a 16-gauge needle by an obstetrician and cord blood was withdrawn from the vein into a blood bag filled with 24.5 mL of anticoagulant citrate phosphate dextrose adenine solution (CPDA). The following puncture was preceded by cord clamping above the previous puncture. The collected cord blood in the bag was registered and stored as whole blood at 4℃ at the blood bank. The cord blood was discarded after 28 days of storage for the safety of transfusion.
Aerobic bacterial blood culture as well as ABO/Rh blood type, complete blood cell count test and serological tests of cord blood were performed just after harvesting. The serological tests included hepatitis B surface antigen, antibody to HBs, hepatitis C antibody, antigen and antibody to human immunodeficiency virus and rapid plasma reagin test. The cord blood contained in a blood bag was examined grossly before use for signs of clot formation or hemolysis.
In all patients, mini-volume priming methods were used with the prime volume of 120 to 140 mL. The mini-volume priming methods and cardiopulmonary bypass strategy in our institution have been previously described.10) The volume of cord whole blood used for priming fluid was calculated based on the preoperative hematocrit (HCT) level, as follows:
= ({[body weight [kg]×80]+priming volume}×target HCT [30%] - {[body weight [kg]×80] × preoperative HCT [%]}) / cord blood HCT (%)
The target HCT value during CPB was 30% at the point-of-care test arterial blood gas analysis (ABGA). Perfusionists added either remained cord blood or packed red blood cell (pRBC) to the CPB circuit when necessary to maintain the target HCT. Data are expressed as median with range values.
From January 2012 to December 2014, 8 neonates were enrolled in this study. The harvested cord blood was not used in 12 patients. Congenital heart disease of the enrolled patients included total anomalous pulmonary venous return, transposition of the great arteries, coarctation of the aorta with ventricular septal defect, hypoplastic left heart syndrome, interrupted aortic arch with tricuspid atresia and truncus arteriosus. Six labors were induced and elective cesarean section was performed in two women. All newborns were mature (Table 1).
The median amount of harvested cord blood was 72.5 mL (43 to 105). The median hematocrit of cord blood was 48.7% (32.0 to 51.2) and aerobic bacteriological culture and serologic exam were negative in all specimen (Table 2).
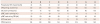
Corrective surgery was performed in all patients with biventricular anatomy. In 2 patients with functional single ventricle physiology, a modified Norwood operation was performed. The median age and body weight at surgery was 11 days (0 to 21) and 3.2 kg (2.2 to 3.7). The median preoperative HCT of neonates was 36.5% (from 31.0 to 45.0%); the median volume of CPB priming was 130 mL (120 to 140). Seven out of eight patients did not need an allo-transfusion in CPB priming and only one neonate used 20 mL of pRBC in CPB priming to obtain the target HCT. In 2 patients, remained cord blood after priming was added to the CPB circuit when necessary to maintain a target HCT (Table 3).
The median postoperative length of stay in the pediatric intensive care unit (PICU) was 11.5 days (6 to 123). There was no evidence of bacteremia as well as significant hemolysis in all patients during the first seven days after operation. The median postoperative length of hospital stay was 22.5 days (16 to 185). The median follow-up duration was 68 days (18 to 748). One early death occurred due to ventricular dysfunction. There was no late mortality during follow-up.
Cord blood was identified as a blood substitute for transfusion in patients with anemia in under-resourced countries as well as in anemic preterm baby.11)12) In recent years, several studies demonstrated the feasibility and safety of the collection, storage, and use of cord blood for autologous transfusions in newborns who underwent cardiac or non-cardiac surgery.6)7)8)9)
Autologous cord blood transfusions have several advantages over homologous transfusions. It is virtually free from immune reactions and infection because it is autologous. It could also be beneficial because cord blood has special properties such as high level of anti-inflammatory cytokines, fetal hemoglobin with its higher oxygen affinity.12) In addition, Cord blood can be harvested without any pain or harm. However autologous cord blood transfusion has a few disadvantages. These include limited amounts of cord blood, appropriateness only for neonates with prenatal diagnosis and potential risk of bacterial contamination.
We could not use the harvested cord blood in 12 patients. The cord blood was discarded because it was not banked immediately after harvest. The other patient underwent a cardiac operation without CPB. Ten of the patients did not undergo cardiac operation during the first 4 weeks after birth. This kind of inaccuracy resulted from the purpose of elevating the sensitivity of fetal surveillance. For example, All patients diagnosed of Tetralogy of Fallot with severe pulmonary stenosis were included in the study for a possibility of neonatal total repair for Tetralogy of Fallot.
The placenta contains about 45 mL of blood per kilogram of fetal weight. So the placenta at term usually contains approximately 150 mL of blood. However harvested volume of cord blood varies from each other. The average storage volume of cord blood has been reported to be 65 mL by Bifano et al.13), 86±16 mL by Bhattacharya12), 72±54 mL by Imura et al.6), 64±35.6 by Taguchi et al.7) and the median volume of harvested cord blood in our series was 72.5 mL. One of the reasons why actual harvested volume was smaller than estimated cord blood is considered to be the hypercoagulability state of cord blood after umbilical clamping. Beattie et al.14) pointed out that thrombosis of blood in the umbilical vessels is commonly highly activated rapidly. And tissue thromboplastin in the placenta has been suggested to enter cord blood by aspiration. Therefore a gentle drawing technique is mandatory. In this study, we withdrew the cord blood by gravity soon after delivery of the baby to increase the harvested volume of blood.
The amount of cord blood required for CPB priming without pRBC depends on CPB protocol as well as hematocrit of the patient and cord blood. Although hematocrit of the patient and cord blood is determined preoperatively, crucial factors calculating the amount of cord blood for CPB priming is CPB protocol including priming volume and target hematocrit during CPB. Mini-volume priming methods were used and high hematocrit strategy was chosen in all patients of this study. One patient needed pRBC for CPB priming and most patients (7 out of 8) needed pRBC during CPB in this study. Therefore to achieve a goal of neonatal cardiac operation without an allo-transfusion, the technique of harvesting cord blood should be refined and the CPB protocol should be applied timely.
Several studies investigated whether harvested cord blood could be banked for transfusion purposes. Bifano et al.13) stored placental whole blood in CPDA for 28 days and reported the hemolysis rate was minimal and the increase in potassium was comparable to stored adult red blood cell (RBC) during a similar period. Other studies however, showed different results.15)16)17) The hemolysis rate increased significantly in time and the pH levels in the cord blood products after 35 days storage were also significantly lower compared to adult RBC products. As a consequence it is likely that the cord blood products would have a similar metabolic profile as adult red cells when adapted to a shorter storage period, and the whole blood storage would cause less deterioration than RBC product. In this study, cord blood was stored as whole blood and discarded when it had been stored more than 28 days.
The bacterial contamination rate was mentioned in the majority of the studies. The proportion of contaminated cord blood used in the clinical studies on autologous cord blood transfusion was between 0 and 9%.18) Imura et al.6) reported negative cultures in all 32 cases of cesarean delivery, but positive cultures in 3 of 18 cases of vaginal delivery, which suggest the risk of contamination by vaginal commensal bacteria. Some studies mentioned that the contamination rates could be lowered significantly by extensive training and showed no bacteriologic contamination in all cases regardless of the type of delivery.8)9) No bacteriologic contamination of cord blood was detected in all 8 cases of this study.
The cord blood was used for CPB priming during neonatal cardiac surgery in this study. The reasons for this are as follows. First, the harvested cord blood can be used entirely at a time with no concern about volume overload. A cord blood transfusion during cardiac surgery can make the harvest, storage and transfusion methods as simple as possible, and the volume of cord whole blood mixed to CPB circuit can be handled by ultrafiltration during CPB. Second, cord whole blood has the potential for reducing systemic inflammatory responses, which remains one of the major causes of CPB-associated organ injury, during CPB because cord blood is rich in anti-inflammatory cytokines. However, it is difficult to prove the benefits of cord blood within clinical settings because the postoperative status of the neonate who underwent cardiac surgery for complex congenital heart disease may be influenced by multifactorial causes. Further studies are mandatory, including experimental as well as clinical ones.
Our clinical experience in the management of prenatally diagnosed complex CHD demonstrated that use of autologous cord blood during neonatal cardiac surgery is encouraging, and show the feasibility and safety of the described method.
This study has some limitations such as small number of patients and simple study design. However, this is a preliminary study to assess safety and feasibility of a new blood management strategy in neonatal cardiac surgery. In addition, homologous blood as well as autologous cord blood was transfused during CPB in most patients. Further studies are warranted on the effects of autologous cord blood transfusion on neonates undergoing cardiac surgery.
In conclusion, autologous cord blood can be used as an alternative to pRBC for CPB priming in neonatal congenital cardiac surgery when patient management is carefully planned.
Figures and Tables
Table 1
Demographic characteristics (n=8, A-H)
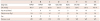
TAPVR: total anomalous pulmonary venous return, TGA: transposition of the great arteries, COA: coarctation of the aorta, VSD: ventricular septal defect, HLHS: hypoplastic left heart syndrome, IAA: interrupted aortic arch, FSV: functional single ventricle, TA: truncus arteriosus, GA: gestational age, op: operation, Kg: kilogram, M: male, F: female, V/D: vaginal delivery, C/S: cesarean section
Table 2
Variables of harvested cord blood (n=8, A-H)
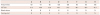
| A | B | C | D | E | F | G | H | |
|---|---|---|---|---|---|---|---|---|
| Amount (mL) | 60 | 43 | 65 | 100 | 100 | 80 | 60 | 105 |
| HCT (%) | 51.2 | 49.6 | 32.0 | 49.7 | 37.9 | 48.7 | 48.7 | 41.9 |
| Blood culture | N | N | N | N | N | N | N | N |
| Serology test | N | N | N | N | N | N | N | N |
Table 3
Operative variables (n=8, A-H)
Acknowledgments
This research is financially supported by 'The Korean Society of Cardiology' (201203-3).
References
1. Society of Thoracic Surgeons Blood Conservation Guideline Task Force. Ferraris VA, Ferraris SP, et al. Perioperative blood transfusion and blood conservation in cardiac surgery: the Society of Thoracic Surgeons and The Society of Cardiovascular Anesthesiologists clinical practice guideline. Ann Thorac Surg. 2007; 83:5 Suppl. S27–S86.
2. Society of Thoracic Surgeons Blood Conservation Guideline Task Force. Ferraris VA, Brown JR, et al. 2011 update to the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists blood conservation clinical practice guidelines. Ann Thorac Surg. 2011; 91:944–982.
3. Redlin M, Kukucka M, Boettcher W, et al. Blood transfusion determines postoperative morbidity in pediatric cardiac surgery applying a comprehensive blood-sparing approach. J Thorac Cardiovasc Surg. 2013; 146:537–542.
4. Choi J, Kim WH, Nam J, Lee YO, Min BJ, Lim HG. Bloodless cardiac surgery in a neonate weighing 2.8 kg. Korean J Thorac Cardiovasc Surg. 2010; 43:721–724.
5. Redlin M, Habazettl H, Boettcher W, et al. Effects of a comprehensive blood-sparing approach using body weight-adjusted miniaturized cardiopulmonary bypass circuits on transfusion requirements in pediatric cardiac surgery. J Thorac Cardiovasc Surg. 2012; 144:493–499.
6. Imura K, Kawahara H, Kitayama Y, Yoneda A, Yagi M, Suehara N. Usefulness of cord-blood harvesting for autologous transfusion in surgical newborns with antenatal diagnosis of congenital anomalies. J Pediatr Surg. 2001; 36:851–854.
7. Taguchi T, Suita S, Nakamura M, et al. The efficacy of autologous cord-blood transfusions in neonatal surgical patients. J Pediatr Surg. 2003; 38:604–607.
8. Fedevych O, Chasovskyi K, Vorobiova G, et al. Open cardiac surgery in the first hours of life using autologous umbilical cord blood. Eur J Cardiothorac Surg. 2011; 40:985–989.
9. Chasovskyi K, Fedevych O, Vorobiova G, et al. Arterial switch operation in the first hours of life using autologous umbilical cord blood. Ann Thorac Surg. 2012; 93:1571–1576.
10. Chang HW, Nam J, Cho JH, Lee JR, Kim YJ, Kim WH. Five-year experience with mini-volume priming in infants </=5 kg: safety of significantly smaller transfusion volumes. Artif Organs. 2014; 38:78–87.
11. Hassall O, Bedu-Addo G, Adarkwa M, Danso K, Bates I. Umbilicalcord blood for transfusion in children with severe anaemia in under-resourced countries. Lancet. 2003; 361:678–679.
12. Bhattacharya N. Placental umbilical cord whole blood transfusion: a safe and genuine blood substitute for patients of the under-resourced world at emergency. J Am Coll Surg. 2005; 200:557–563.
13. Bifano EM, Dracker RA, Lorah K, Palit A. Collection and 28-day storage of human placental blood. Pediatr Res. 1994; 36(1 Pt 1):90–94.
14. Beattie R, Stark JM, Wardrop CA, Holland BM, Kinmond S. Autologous umbilical cord blood transfusion. Arch Dis Child Fetal Neonatal Ed. 1996; 74:F221.
15. Brune T, Garritsen H, Witteler R, et al. Autologous placental blood transfusion for the therapy of anaemic neonates. Biol Neonate. 2002; 81:236–243.
16. Brune T, Fill S, Heim G, Rabsilber A, Wohlfarth K, Garritsen HS. Quality and stability of red cells derived from gravity-separated placental blood with a hollow-fiber system. Transfusion. 2007; 47:2271–2275.
17. Widing L, Bechensteen AG, Mirlashari MR, Vetlesen A, Kjeldsen-Kragh J. Evaluation of nonleukoreduced red blood cell transfusion units collected at delivery from the placenta. Transfusion. 2007; 47:1481–1487.
18. Durandy Y. Use of blood products in pediatric cardiac surgery. Artif Organs. 2015; 39:21–27.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download