Abstract
Background and Objectives
Subjects and Methods
Results
Figures and Tables
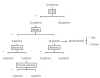 | Fig. 1A diagram showing the outcomes of the study population. LVSD: left ventricular systolic dysfunction, RWMA: regional wall motion abnormality. |
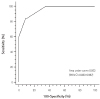 | Fig. 2Receiver operating curve analysis in the detection of left ventricular systolic dysfunction by a clinical score. Clinical score ≥8 showed optimal sensitivity (84%) and specificity (91%). CI: confidence interval. |
Table 1
Baseline characteristics (n=81)

EMS: emergency management service, CK: creatinine kinase, CK-MB: creatinine kinase-MB fraction, IQR: inter-quartile range, LVEDD: left ventricular end-diastolic dimension, LVESD: left ventricular end-systolic dimension, LVEDV: left ventricular end-diastolic volume, LVESV: left ventricular end-systolic volume, LVEF: left ventricular ejection fraction, LA: left atrium, DT: deceleration time, RWMA: regional wall motion abnormality, LVSD: left ventricular systolic dysfunction
Table 2
Univariate analysis according to the presence of left ventricular systolic dysfunction
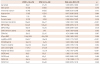
Values are presented as mean±SD or n (%). CI: confidence interval, LVSD: left ventricular systolic dysfunction, SBP: systolic blood pressure, DBP: diastolic blood pressure, CXR: chest X-ray, COHb: carboxyhemoglobin, NT pro-BNP: N-terminal pro-B type natriuretic peptide, CK: creatinine kinase, LVESD: left ventricular end-systolic dimension, LVEDD: left ventricular end-diastolic dimension, LVESV: left ventricular end-systolic volume, LVEDV: left ventricular end-diastolic volume
Table 3
Multivariate analysis with clinical variables in the prediction of left ventricular systolic dysfunction

Table 4
Areas under the curve in the detection of left ventricular systolic dysfunction





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download