Abstract
Background and Objectives
Heart failure (HF) is an important healthcare issue because of its high mortality, morbidity, and healthcare costs. The number of HF patients is increasing worldwide as a consequence of aging of the population. However, there are limited studies on the prevalence of HF in Korea. This study aimed to estimate the prevalence of HF, its comorbidities, and the projected population with HF in the future.
Materials and Methods
The prevalence and comorbidity estimates of HF were determined using data from the 2002-2013 National Sample Cohort based on the National Health Information Database. We calculated the projected prevalence of HF by multiplying the estimated prevalence in 2013 by the projected population counts for 2015-2040.
Results
The prevalence of HF in Korea was estimated to be 1.53% in 2013. The prevalence of HF in Korea is expected to increase by 2-fold, from 1.60% in 2015 to 3.35% in 2040. By 2040, more than 1.7 million Koreans are expected to have HF. In terms of comorbid diseases of HF, ischemic heart disease, hypertension, and diabetes mellitus were common (45.4%, 43.6%, and 49.1% in 2013, respectively). The prevalence rates of arrhythmia, valvular disease, and cardiomyopathy in HF patients were approximately 22.6%, 5.6%, and 3.1% in 2013, respectively.
HF is the leading cause of morbidity, mortality, and healthcare costs around the world. The number of HF patients is increasing worldwide, and its prevalence is expected to rise more steeply as the population ages. On the basis of data from the National Health and Nutrition Examination Survey (NHANES) 2009-2012, about 5.7 million (2.2%) people over the age of 20 years have HF and more than 550000 people are newly diagnosed with HF every year in the USA.1) By 2030, the prevalence of HF will increase to 46%, affecting more than 8 million people, and total medical costs for HF patients are expected to increase from $20.9 billion to $53.1 billion.1)2) In Japan, it is estimated that 1.0 million individuals have HF, and the number of Japanese outpatients with left ventricular (LV) dysfunction is predicted to gradually increase from 979000 in 2005 to 1.3 million by 2030.3)4)
Therefore, we assume that the prevalence of HF in Korea is also increasing because of the westernization of lifestyle, rapid aging of the population, and the increased number of survivors of serious cardiovascular illness due to recent advances in medical and surgical treatment.5)
However, there are limited studies on the prevalence or comorbidities of HF in Korea. Although there are several studies in developing countries, data are limited to the East and South Asian countries, and the majority of these are not nationwide studies.6)7)8)
The present study aimed to estimate the prevalence of HF, its comorbidities, and the projected population with HF using National Health Insurance Service (NHIS) sample cohort data based on the nationwide database of Korea from 2002 to 2013.
Data from the National Sample Cohort (NSC) based on theNational Health Information Database was used. Korea has anobligatory public health insurance system, termed of the NHISwith which more than 97% of people are affiliated. The NSCwas constructed by the NHIS in 2011 and opened to the publicin July 2014 (http://nhiss.nhis.or.kr). The NSC database consists ofapproximately 1 million medical insurance subscribers, accountingfor about 2% of the entire nation. Data were produced by the NHISusing a systematic sampling method to generate a representativesample from all 46605422 Korean residents in 2002. This databaseincludes all medical claim files from January 2002 to December2013. Each database includes diagnostic codes, procedures,prescription drugs, personal information about the patient,information about the hospital, the direct medical costs of bothinpatient and outpatient care, and dental services. The NHIS usesthe Korean Classification of Disease-6 (KCD-6), which is a similarsystem to the International Classification of Diseases-10 (ICD-10)(Table 1).
HF patients were defined as those with "heart failure" accordingto the disease code in the main code and the sub-code in theclaims data. HF patients who were assigned the following KCD-6 disease codes were considered as: "hypertensive heart diseasewith (congestive) HF" (I11.0), "hypertensive heart and renal diseasewith (congestive) HF" (I13.0), "hypertensive heart and renal diseasewith both (congestive) HF and renal failure" (I13.2), and "HF" (I50)including "congestive HF" (I50.0), "LV failure" (I50.1), and "HF andunspecified" (I50.9). Five comorbidities were defined, namely,hypertension, ischemic heart disease (IHD), diabetes mellitus (DM),arrhythmia, valvular disease, cardiomyopathy, and others, whichare closely related to HF (Supplementary Table 1).6)8)
The prevalence of HF was calculated by multiplying the estimatedprevalence in 2013 by the projected population counts for 2015-2040. The projected population by sex and age between 2015and 2040 in Korea was obtained from the Population Projectionsfor Korea: 2010–2060. Statistics Korea estimated the projectedpopulation by the cohort component method, which reflectschanges in the rates of births, deaths, and migration in the 2013census9) to predict the increase in the population by sex and age.
The prevalence of HF by sex is shown in Fig. 1. The prevalenceof HF in Korea increased approximately two times (from 0.75% in2002 to 1.53% in 2013), and it was higher in women than in men. The prevalence increased substantially in both sexes from 2002 to2013; it was 0.54% and 0.96% in 2002, and 1.34% and 1.72% in2013 for men and women, respectively.
Age is an important risk factor for HF and the prevalence of HFand LV dysfunction increases with age. In 2013, the prevalence ofHF was 12.6% in subjects aged 80 years or older, while it was 1.0%and 5.5% in those aged 40-59 years and 60-79 years, respectively(Fig. 2). The prevalence of HF in subjects aged 80 years or olderwas approximately 8-fold higher than the overall prevalence of HF(1.53%). The prevalence of HF in females was higher than in malesamong subjects aged 60 or older.
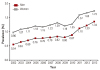
Fig. 3 illustrates the comorbidities of HF patients in the NHIS (2003 vs. 2013). The investigated comorbid diseases were IHD, hypertension, DM, arrhythmia, valvular disease, cardiomyopathy, and others. Others included cardiopulmonary disease, chronic obstructive pulmonary disease and myocarditis. IHD, Hypertension and DM were common in HF patients (36.3%, 46.2%, and 33.4% in 2003; 45.4%, 43.6%, and 49.1% in 2013, respectively). The prevalence rates of IHD and DM were markedly higher in 2013 than in 2003 in both men and women.
IHD was more common in men than in women. Arrhythmia was observed in 22% of the patients. Valvular disease was observed in 5.6% of total HF patients and higher in women than in men in 2013. The prevalence of valvular disease was markedly decreased in men during the last decade (from 7.6% to 4.6%). Approximately 3.1% of HF patients had cardiomyopathy.
The prevalence rates of comorbid diseases according to age and sex are shown in Fig. 4. The prevalence of IHD increased with age; it was 23.0% in subjects younger than 40 years, 39.7% in subjects aged 40-59 years, 49.4% in subjects aged 60-79 years, and 44.2% in subjects aged 80 years or older. Among the comorbidities, hypertension showed high prevalence in most age categories. The prevalence of DM was 27.2% in subjects younger than 40 years, 43.6% in subjects aged 40-59 years, 53.6% in subjects aged 60-79 years, and 46.4% in subjects aged 80 years or older. The prevalence rates of IHD and DM in HF patients were higher in men than in women in all age categories. The prevalence of arrhythmia was relatively high compared to other diseases in subjects younger than 40 years. The prevalence of valvular disease was higher in women than in men in most age categories, except for among subjects younger than 40 years. The prevalence of cardiomyopathy tended to decrease with age both in men and women.
The projected numbers of people in Korea with HF from 2015 to 2040 for different age groups are shown in Table 2. By 2020, the prevalence of HF is expected to be 1.89% and more than 970000 people are expected to have HF. By 2040, more than 1.7 million Koreans are expected to have HF, of whom 628000 are expected to be older than 80 years (>35% of all HF patients). The prevalence of HF in Korea is expected to increase by 2-fold (3.35%) by 2040.
The prevalence of HF in the population of Korea increased from 0.75% (370000 people) in 2002 to 1.53% (755000 people) in 2013. The main reason for the increasing prevalence of HF is the rapid aging of the Korean population. The elderly population growth rate in Korea is the highest among countries that are members of the Organization for Economic Cooperation and Development. The prevalence of HF among people aged 60 or older in 2013 was high (7.6%) in our study. By 2040, >1.7 million (3.35%) Koreans will have HF, of whom 1551000 will be aged ≥60 years (>90% of all HF patients). The other reasons for the increased prevalence of HF are that the number of IHD patients has increased due to the accelerated westernization of lifestyle in Korean people, and the number of survivors of an acute coronary event has dramatically increased due to progress in treatment. Recently, similar trends toward ischemia as a cause of HF were observed in Asia, including China and Japan.3)
The prevalence of HF was lower in Korea (1.53%) than in the USA (2.2%).1) We speculate that this is for two reasons. First, IHD is the predominant cause of HF in Western high-income nations, whereas the prevalence of IHD is relatively low in Asia.10) The prevalence of IHD among total HF patients in Korea was 45.4%, which is considerably lower than in Western studies (50-57%).11)12) Second, the prevalence of HF in the USA was based on data from health interviews of the NHANES, whereas our study used NHIS sample cohort data based on KCD-6 disease codes in Korea. Our data relied on hospital dismissal codes and may underestimate the true burden of HF by "discounting" all cases ever diagnosed with IHD, hypertension, or other disorders. There are only several reports regarding the prevalence of HF in Asia. A survey of the adult population (aged ≥35 years) of Xinjiang, China (n=8459) reported that the prevalence of congestive HF was 1.26%.13) A single center-based study in Malaysia reported that the prevalence of HF among acute medical admissions period was 6.7%.14) Since these aforementioned Asian studies were hospital-based, the prevalence of HF in Korea and other Asian countries cannot be accurately compared.6)
Being of the male sex is a classic demographic risk factor for the development of HF, along with older age, ethnicity, and low socioeconomic state.1)15) However, the prevalence of HF was higher in women than in men in our study (1.72% vs. 1.34%, Fig. 1). Our estimates of HF prevalence in Korea differ from those published in the Heart Disease and Stroke Statistics-2015 Update, which reported a higher prevalence of HF in men than in women in the USA.1) Although the reason for this difference is uncertain, we have several suggestions. First, the omission of "HF" diagnostic codes for HF patients with IHD that was more prevalent in men, which would have led to the exclusion of more men than women. Second, patients with HF and a preserved ejection fraction (HFpEF) are more likely to be female and to have more comorbidities.16)17) It is cautiously forecasted that the prevalence of HFpEF increases with age and that increased access to echocardiography contributed to an increase in the diagnosis of HFpEF.18)
We investigated the prevalence of comorbid diseases associated with HF. In our study, the prevalence rates of patients with a history of IHD, hypertension, and DM were high (45.4% and 43.6%, and 49.1%, respectively), and arrhythmia was observed in approximately 22% of HF patients. The prevalence of IHD has increased markedly during the last decade (36.3% vs. 45.4%). The prevalence of most comorbidities increased with age except for cardiomyopathy. The prevalence of cardiomyopathy was higher in young people than in elderly people.
IHD is thought to be the most important risk factor for HF. In the Korean Heart Failure (KorHF) study, 52.3% of patients had a history of IHD.19) Additionally, 38% of HF patients were reported to have IHD in the Korean Acute Heart Failure(KorAHF) study.20) This discrepancy may be due to differences in the enrolled patients. The KorHF study recruited subjects hospitalized at university hospitals and the KorAHF study enrolled acute HF syndrome patients who were admitted to hospitals. In our study, the prevalence of IHD (45.4%) in HF patients was considerably lower than that reported in Western studies (50-57%).10)11)12) In Japan, coronary artery disease has the highest prevalence; its incidence ranges from 32.0% to 53.1% among those who experience HF.5)6)
In comparison to IHD, hypertension is associated with a smaller relative risk of developing HF, but contributes more to the overall population burden of HF because it has a higher prevalence.21) The prevalence of hypertension as a comorbidity of HF patients was lower in Korea (43.6%) than in other studies, such as in the Acute Decompensated Heart Failure Syndromes (ATTEND) registry (71%),22) the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) (71%),23) and the Euro-Heart Failure Survey II (EHFSII) (63%).24) In Japan, the prevalence of hypertension varied widely, ranging from 39.2% to 77.6%.5)22)25) In the KorHF study, 46.5% of patients had a history of hypertension.19) The reason for the low prevalence of hypertension in HF patients in Korea should be investigated in future studies.
DM, obesity, valvular disease, cigarette smoking, and racial differences are other risk factors for HF. DM is becoming increasingly recognised as being responsible for HF, while hypertension and valvular disease have become less prevalent causes of HF because of improvements in detection and therapy.26)27) Over four decades of observation in the Framingham Study, the prevalence of DM as a contributing cause increased by more than 20% per decade.26) The prevalence of IHD and DM in HF patients is also expected to increase due to the acceleration in the adoption of Western lifestyles and the development of treatments in Korea. By contrast, the prevalence of valvular disease is expected to decrease in Korea.
HF is an important healthcare issue because of its medical costs. This issue will become increasingly important as the population ages. Total medical costs for HF in the USA are expected to increase from $20.9 billion in 2012 to $53.1 billion in 2030, a 2.5-fold increase. The total cost of HF (direct and indirect costs) is expected to increase from $30.7 billion in 2012 to $69.8 billion in 2030.2) According to our analysis, the projected prevalence of HF in Korea is also expected to markedly increase because of its aging population. Therefore, the cost of caring for HF patients care in Korea is expected to greatly increase and will remain a significant concern and economic burden for our healthcare system. We think the best solution is prevention of HF. This requires early detection and the treatment of predisposing conditions and of high-risk patients. A further study that projects the cost of HF patient health care is needed to predict the economic burden on the Korean healthcare system and to devise a strategy for the prevention and treatment of HF.
This study has several limitations. First, we estimated the prevalence and comorbidities of HF by using the NSC database, which is based on KCD-6 disease codes in Korea, and the accuracy of diagnosis was not validated in this study. Further studies to validate HF patients with health insurance data using either hospital-based medical records or prospective studies are required. The true burden of HF may have been underestimated due to the omission of HF patients who were assigned diagnostic codes for IHD, hypertension, or others. Due to the characteristics of the claim data, it was not possible to discriminate etiologic diseases from simple comorbid disorders. Therefore, we had to present the prevalence of the representative diseases as comorbidities (IHD, hypertension, DM, arrhythmia, valvular disease, cardiomyopathy, and others) of HF. To identify the main causative disease, a prospective study involving the detailed investigation of baseline characteristics, including obesity, cigarette smoking, and others, will be required. Studies such as the KorHF study will be helpful in this regard. To get more information to aid in HF management and prevention, a nationwide registry containing accurate data concerning the prevalence, etiology, comorbidities, mortality, and associated healthcare costs of HF is needed.
In conclusion, our study shows an increase in the prevalence of HF and its comorbidities during the last decade and provides basic information that may be useful for the prevention and management of HF in Korea.
Figures and Tables
Fig. 2
Estimated prevalence of heart failure by age group (National Insurance Service's sample cohort database, 2013).
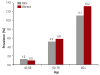
Fig. 3
Comorbidities of heart failure patients in NHIS (2003 vs. 2013). IHD:ischemic heart disease, DM:diabetes mellitus.

Fig. 4
Prevalence of comorbid diseases according to age and sex in NHIS (2013). (A) Ischemic heart disease, (B) Hypertension, (C) Diabetes mellitus (DM), (D) Arrhythmia, (E) Valvular heart diseases and (F) Cardiomyopathy.

Table 1
Contents of the NSC database (DB) and variables

Table 2
Projected number of HF patients in 2015-2040 according to age group

Acknowledgments
This work was supported by funding from the Korea National Institute of Health [4800-4845-302-210 (2011-NG63002-00)]. This study used NHIS-NSC data (NHIS-2014-2-010) made by NHIS. The authors declare no conflict of interest with NHIS. The authors alone are responsible for the contents and writing of the paper.
References
1. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015; 131:e29–e322.
2. Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013; 6:606–619.
3. Okamoto H, Kitabatake A. The epidemiology of heart failure in Japan. Nihon Rinsho. 2003; 61:709–714.
4. Okura Y, Ramadan MM, Ohno Y, et al. Impending epidemic: Future projection of heart failure in Japan to the year 2055. Circ J. 2008; 72:489–491.
5. Shiba N, Nochioka K, Miura M, Kohno H, Shimokawa H. CHART-2 Investigators. Trend of westernization of etiology and clinical characteristics of heart failure patients in Japan--first report from the CHART-2 study. Circ J. 2011; 75:823–833.
6. Sakata Y, Shimokawa H. Epidemiology of heart failure in Asia. Circ J. 2013; 77:2209–2217.
7. Pillai HS, Ganapathi S. Heart failure in South Asia. Curr Cardiol Rev. 2013; 9:102–111.
8. Guo Y, Lip GY, Banerjee A. Heart failure in East Asia. Curr Cardiol Rev. 2013; 9:112–122.
9. Statistics Korea. Population projections for Korea: 2010-2060 (based on the 2010 census). Daejeon: Statistics Korea;2011.
10. Khatibzadeh S, Farzadfar F, Oliver J, Ezzati M, Moran A. Worldwide risk factors for heart failure: A systematic review and pooled analysis. Int J Cardiol. 2013; 168:1186–1194.
11. Adams KF Jr, Fonarow GC, Emerman CL, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: Rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005; 149:209–216.
12. Abraham WT, Fonarow GC, Albert NM, et al. Predictors of in-hospital mortality in patients hospitalized for heart failure: Insights from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). J Am Coll Cardiol. 2008; 52:347–356.
13. Yang YN, Ma YT, Liu F, et al. Incidence and distributing feature of chronic heart failure in adult population of Xinjiang. Zhonghua Xin Xue Guan Bing Za Zhi. 2010; 38:460–464.
14. Chong AY, Rajaratnam R, Hussein NR, Lip GY. Heart failure in a multiethnic population in Kuala Lumpur, Malaysia. Eur J Heart Fail. 2003; 5:569–574.
15. Schocken DD, Benjamin EJ, Fonarow GC, et al. Prevention of heart failure: a scientific statement from the American Heart Association Councils on Epidemiology and Prevention, Clinical Cardiology, Cardiovascular Nursing, and High Blood Pressure Research; Quality of Care and Outcomes Research Interdisciplinary Working Group; and Functional Genomics and Translational Biology Interdisciplinary Working Group. Circulation. 2008; 117:2544–2565.
16. Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006; 355:251–259.
17. Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006; 355:260–269.
18. Shiba N, Shimokawa H. Chronic heart failure in Japan: Implications of the CHART studies. Vasc Health Risk Manag. 2008; 4:103–113.
19. Choi DJ, Han S, Jeon ES, et al. Characteristics, outcomes and predictors of long-term mortality for patients hospitalized for acute heart failure: a report from the Korean heart failure (KorHF) registry. Korean Circ J. 2011; 41:363–371.
20. Lee SE, Cho HJ, Lee HY, et al. A multicentre cohort study of acute heart failure syndromes in Korea: rationale, design, and interim observations of the Korean Acute Heart Failure (KorAHF) registry. Eur J Heart Fail. 2014; 16:700–708.
21. Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 2007; 93:1137–1146.
22. Kajimoto K, Sato N, Keida T, et al. investigators of the Acute Decompensated Heart Failure Syndromes (ATTEND) registry. Association between length of stay, frequency of in-hospital death, and causes of death in Japanese patients with acute heart failure syndromes. Int J Cardiol. 2013; 168:554–556.
23. Abraham WT, Fonarow GC, Albert NM, et al. OPTIMIZE-HF Investigators and Coordinators. Predictors of in-hospital mortality in patients hospitalized for heart failure: insights from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). J Am Coll Cardiol. 2008; 52:347–356.
24. Nieminen MS, Brutsaert D, Dickstein K, et al. EuroHeart Survey Investigators. Heart Failure Association, European Society of Cardiology. EuroHeart Failure Survey II (EHFS II): A survey on hospitalized acute heart failure patients: Description of population. Eur Heart J. 2006; 27:2725–2736.
25. Hamaguchi S, Kinugawa S, Tsuchihashi-Makaya M, et al. JCARE-CARD Investigators. Loop diuretic use at discharge is associated with adverse outcomes in hospitalized patients with heart failure: A report from the Japanese cardiac registry of heart failure in cardiology (JCARE-CARD). Circ J. 2012; 76:1920–1927.
26. Kannel WB, Ho K, Thom T. Changing epidemiological features of cardiac failure. Br Heart J. 1994; 72:2 Suppl. S3–S9.
27. He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med. 2001; 161:996–1002.
Supplementary Materials
The online-only Data Supplement is available with this article at http://dx.doi.org/10.4070/kcj.2016.46.5.658.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download