Abstract
Background and Objectives
The number of permanent pacemakers (PPMs) implanted in patients in Japan and Korea differs significantly. We aimed to investigate the differences in decision making processes of implanting a PPM.
Materials and Methods
Our survey included 15 clinical case scenarios based on the 2008 AHA/ACC/HRS guidelines for device-based therapy of cardiac rhythm abnormalities (class unspecified). Members of the Korean and Japanese Societies of Cardiology were asked to rate each scenario according to a 5-point scale and to indicate their decisions for or against implantation.
Results
Eighty-nine Korean physicians and 192 Japanese physicians replied to the questionnaire. For the case scenarios in which there was a class I indication for PPM implantation, the decision to implant a PPM did not differ significantly between the two physician groups. However, the Japanese physicians were significantly more likely than the Korean physicians to choose implantation in class IIa scenarios (48% vs. 37%, p<0.001), class IIb scenarios (40% vs. 19%, p<0.001), and class III scenarios (36% vs. 18%, p<0.001). These results did not change when the cases were categorized based on disease entity, such as sinus node dysfunction and conduction abnormality.
Different countries appear to differ significantly with respect to rates of permanent pacemaker (PPM) implantations. For example, the number of PPM implantations per capita is much lower in the populations of Asian countries than in Western populations.
According to the 2009 11th World Survey of Arrhythmias Project,1) the number of new PPM implantations in 2009 was 927 per million in Germany and 767 per million in the United States. In contrast, in Japan, PPMs were implanted in 272 patients per million as opposed to only 35 per million in Korea – an eight-fold difference in the rates of per capita PPM implantations. Possible explanations for the differences between two countries may include (1) differences in reimbursement policies, (2) differences in the incidence of sinus node or conduction disorders, and (3) cultural differences regarding the acceptance of device implantation among physicians and patients that may serve as barriers to PPM implantation.
We conducted a survey among physicians in Japan and Korea to determine what factors may be influencing their decision to implant PPMs.
A survey was created that included 15 different clinical case scenarios representative of the class I, IIa, IIb, and III indications for PPM implantation stated in the 2008 AHA/ACC/HRS guidelines.2) Members of the Korean and Japanese Societies of Cardiology (including electrophysiologists, non-electrophysiologists, and cardiac surgeons) were asked to respond to a questionnaire to determine whether or not they would implant a PPM in each of the clinical scenarios presented to them.
Although the classes were not indicated in the questionnaire, they could be broken down as follows: five in class I (group 1), 6 in class IIa (group 2), 2 in class IIb (group 3), and 2 in class III (group 4). (The questionnaire can be found in Table 1 of the supplemental data.) Respondents, who remained anonymous, were asked to rate each scenario according to a 5-point scale; a score of 5 signified that the respondent was confident that a PPM should be implanted and a score of 1 signified that the physician was confident that it should not be implanted.
For the purpose of our analysis, scores of 4 and 5 were considered to be positive for the decision to implant a PPM. Survey results were compiled and analyzed using SPSS software version 15.0 (SPSS Inc., Chicago, IL, USA). p values of less than 0.05 were considered statistically significant.
The surveys were sent to 330 Korean physicians and 390 Japanese physicians, of whom 89 (27%) and 192 (49%) returned the completed questionnaires. Table 1 lists the characteristics of the respondents, and the responses to each questionnaire from the two physician groups are presented in Supplemental Table 2.
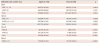
Results were analyzed according to either class indications or disease entities (Table 2 and Fig. 1). For the scenarios described in the group 1, there was no significant difference in the decision to implant a PPM between Korean and Japanese physicians. However, for the group 2, the Japanese physicians were significantly more likely than the Korean physicians to implant a PPM (48% vs. 37%, p<0.001); corresponding rates were 40% vs. 19% (p<0.001) for group 3 and 36% vs. 18% (p<0.001) for the group 4 scenarios. These results did not change when the cases were categorized based on disease entity, such as sinus node dysfunction and conduction abnormality.
This study demonstrates significant differences in the clinical decisions made by Korean and Japanese physicians based on various indications for PPM implantation. Most likely, these differences are not simply due to relative conservatism among Korean electrophysiologists compared with their Japanese counterparts. Other factors such as national reimbursement policies and cultural differences with respect to patient acceptance of PPM implantation may also influence their decisions.
Both countries have mandatory health insurance systems, but their reimbursement processes differ. The Korean government is in charge of the single health insurance organization in the country, and all medical practices are monitored by the Health Insurance Review and Assessment (HIRA) service. The Japanese government runs two health insurance organizations but does not impose the additional level of regulation found in Korea (Korean HIRA). In general, the reimbursement environment is more strict in Korea than in Japan. In Japan, all the procedures and treatments are reimbursed by the insurance system regardless of the class indications stated in the AHA/ACC/HRS guidelines. In contrast, physicians in Korea can be reimbursed only for class I and selective class IIa indications in implanting a PPM. This difference in reimbursement systems between the two countries is likely to play a major role in physician decisions about whether or not to implant a PPM.
According to our survey analysis, Korean and Japanese physicians differed mainly in their decisions regarding class II PPM indication scenarios (groups 2 and 3). In both countries, the majority of respondents did not favor implantation of PPMs for class III indication scenarios (group 4), although Japanese physicians responded more positively to these scenarios. Japanese physicians have their own guidelines for pacemaker implantation3) that do not include class III indications in patients with sinus node dysfunction or atrioventricular block, and this could explain the difference in their decisions regarding the group 4 scenarios.
It is well known that racial differences can affect decisions about the utilization of certain medical procedures.4)5)6) This discrepancy may be due in part to cultural factors regarding the acceptance of innovative medical technologies.7) Differences in the relative acceptance of pacemaker implantation by patients in Korea and Japan may also influence physician decision making processes.
The present study has several limitations. The response rate was lower in Korea (27%) than in Japan (49%). In studies with this type of methodological design, response bias can be an important limitation. We believe that this is partially adjusted by keeping the names of respondents anonymous. In addition, in order to increase participation in this survey, we limited the number of questions and made each question as simple as possible. Our case scenarios were carefully designed to represent scenarios for which a divergence of opinion was likely, thus disclosing subtle differences in physician decision making. Furthermore, during the design of the questionnaire, each case scenario required consensus among three electrophysiologists in the assignment of appropriate class indications.
Korean physicians are generally less likely to favor implantation of a PPM than are Japanese physicians for class IIa and IIb PPM indications. These differences in physician decision making probably contribute to the small number of PPMs implanted in Korea, as compared with Japan. Insurance reimbursement systems as well as cultural differences might influence physicians' decision in implanting a PPM.
Figures and Tables
 | Fig. 1Rate of positive responses for the PPM implantation. PPM: permanent pacemaker, SND: sinus node dysfunction, AVB: atrioventricular block. |
Table 1
Characteristics of survey respondents
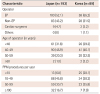
Table 2
Rates of positive responses regarding PPM implantation
References
1. Mond HG, Proclemer A. The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: calendar year 2009-A World Society of Arrhythmia's project. Pacing Clin Electrophysiol. 2011; 34:1013–1027.
2. Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices) developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008; 51:e1–e62.
3. JCS Joint Working Group. Guidelines for Non-Pharmacotherapy of Cardiac Arrhythmias (JCS 2011). Circ J. 2013; 77:249–274.
4. Barnhart JM, Fang J, Alderman MH. Differential use of coronary revascularization and hospital mortality following acute myocardial infarction. Arch Intern Med. 2003; 163:461–466.
5. Groeneveld PW, Heidenreich PA, Garber AM. Trends in implantable cardioverter-defibrillator racial disparity: the importance of geography. J Am Coll Cardiol. 2005; 45:72–78.
6. Thomas KL, Al-Khatib SM, Kelsey RC 2nd, et al. Racial disparity in the utilization of implantable-cardioverter defibrillators among patients with prior myocardial infarction and an ejection fraction of <or=35%. Am J Cardiol. 2007; 100:924–929.
7. Groeneveld PW, Sonnad SS, Lee AK, Asch DA, Shea JE. Racial differences in attitudes toward innovative medical technology. J Gen Intern Med. 2006; 21:559–563.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download