Abstract
Background and Objectives
The aim of this study was to evaluate the association between the extent of coronary artery disease assessed by the Gensini score and/or the SYNTAX score and the significant carotid stenosis in patients undergoing coronary artery bypass grafting (CABG).
Subjects and Methods
A total of 225 patients who had carotid doppler ultrasonography prior to CABG were included retrospectively. Significant coronary artery disease was assumed as a lumen diameter stenosis of ≥50% in any of the major epicardial coronary arteries. The severity of carotid stenosis was determined by B-mode and duplex ultrasonography. Clinically significant carotid stenosis was defined as peak systolic velocity greater than 125 cm/s.
Results
The mean value of SYNTAX score and Gensini score was highest in patients allocated to significant carotid stenosis (22.98±7.32, p<0.001 and 77.40±32.35, p<0.001, respectively). The other risk factors for significant carotid stenosis were found to be male gender (p=0.029), carotid bruit (p<0.001), diabetes (p=0.021), left main disease (p=0.002), 3-vessel disease (p=0.008), chronic total coronary occlusion (p=0.001), and coronary artery calcification (p=0.001) in univariate analysis. However, only the Gensini score (odds ratio[OR]=1.030, p=0.004), carotid bruit (OR=0.068, p<0.001), and male gender (OR=0.190, p=0.003) were the independent predictors. The Gensini score cut off value predicting significant carotid stenosis was 50.5 with 77% sensitivity (p<0.001).
Atherosclerosis that results in coronary artery disease (CAD) is a generalized process that may also affect carotid arteries.1) The extent of CAD increases the risk of simultaneous carotid stenosis.2)3)4) However, the extent of CAD has been limited to the number of stenosed coronary vessels in previous studies. Using additional parameters such as the degree of luminal narrowing and geographic importance of the lesion position can precisely determine the extent of atherosclerotic burden.5)6)7) Therefore, an angiographic scoring system such as the Gensini score or the SYNTAX score may show a better relationship with the severity of carotid stenosis.
The coexistence of carotid stenosis increases the risk of a postoperative stroke in patients undergoing coronary artery bypass grafting (CABG).1) However, routine carotid screening prior to CABG is controversial. Determination of the predictors of carotid stenosis may be useful to identify those patients who need carotid screening prior to CABG. We performed a retrospective analysis to identify risk factors for significant carotid stenosis in patients undergoing CABG. The main aim of this study was to evaluate whether the Gensini score and/or the SYNTAX score is related to carotid stenosis. Second, we investigated the relations of the left main coronary artery disease, 3-vessel CAD, coronary artery calcification, and chronic total coronary occlusion to carotid stenosis.
A total of consecutive 225 patients who underwent CABG and carotid doppler ultrasonography (US) were retrospectively included after the exclusion process. Clinical and demographic features of the patients (age, gender, diabetes mellitus, hypertension, hyperlipidemia, peripheral arterial disease, chronic kidney disease, history of smoking) were analyzed by retrospective chart review.
Patients with acute ST segment elevation myocardial infarction, acute symptomatic carotid artery disease or the patients who did not receive preoperative carotid screening were excluded from the study. In addition, we excluded patients younger than 60 years of age because the incidence of carotid stenosis is low within the young population.8) Patients with a history of previous CABG, carotid endarterectomy, carotid stenting and history of stroke were also excluded from the study.
Hypertension was defined as a blood pressure of ≥140/90 mmHg or the use of antihypertensive medication. Hyperlipidemia was defined as a fasting low density lipoprotein concentration of >130 mg/dL or the use of antihyperlipidemic medication. Diabetes mellitus was defined as a fasting plasma glucose concentration ≥126 mg/dL or the use of antidiabetic medication. The study was approved by the local ethics committee on human research at our institution.
Coronary angiography was assessed by two experienced independent observers who were blinded to both the patient's clinical characteristics and carotid Doppler US findings. Significant CAD was assumed as a lumen diameter stenosis of ≥50% in any of the major epicardial coronary arteries including the left main coronary artery, left anterior descending artery, left circumflex artery, right coronary artery, or one of their major branches. Dispersion of the CAD categorized as one-vessel disease (1-VD; disease in 1 vessel), two-vessel disease (2-VD; disease in 2 vessels or left main trunk disease without right coronary artery stenosis) or three-vessel disease (3-VD; disease in 3 vessels or left main trunk disease with right coronary artery stenosis). Left main disease is defined as significant stenosis (≥50%) of the left main trunk, with or without concomitant lesions in other vessels.
Based on the baseline diagnostic angiogram, the total SYNTAX score was calculated from the summation of the individual scorings for each separate lesion by using a SYNTAX score algorithm available on the SYNTAX website (http://www.syntaxscore.com).
Calculation of the Gensini score was initiated by giving a severity score to each coronary stenosis as follows: 1 point for ≤25% narrowing, 2 points for 26 to 50% narrowing, 4 points for 51 to 75% narrowing, 8 points for 76 to 90% narrowing, 16 points for 91 to 99% narrowing, and 32 points for total occlusion. Thereafter, each lesion score is multiplied by a factor that takes into account the importance of the lesion's position in the coronary circulation (5 for the left main coronary artery, 2.5 for the proximal segment of the left anterior descending coronary artery, 2.5 for the proximal segment of the circumflex artery, 1.5 for the mid-segment of the left anterior descending coronary artery, 1.0 for the right coronary artery, the distal segment of the left anterior descending coronary artery, the posterolateral artery, and the obtuse marginal artery, and 0.5 for other segments). Finally, the Gensini score was calculated by summation of the individual coronary segment scores. The patients were classified into 3 groups according to the tertile of Gensini score.
B-mode and duplex US findings were obtained from the right and left common carotid and internal carotid arteries using the Logiq 9 ultrasound machine (GE Healthcare Technologies, Ultrasound, Milwaukee, WI, USA) centrally at the deparment of radiology. The severity of stenosis was determined by the maximum percentage of diameter reduction recorded by B-mode US, and by the peak-systolic velocities (PSV) measured in the internal carotid artery. The patients who had a significant discrepancy between B-mode ultrasound and PSV were excluded from the study.
PSV <125 cm/s with no sign of atherosclerosis was considered as normal carotid artery. PSV <125 cm/s with the presence of a sonographic atherosclerotic lesion was considered to represent <50% stenosis. PSV between 125 and 230 cm/s was considered to represent 50 to 70% stenosis, whereas PSV greater than 230 cm/s was accepted as 70 to 99% stenosis. Total or near occlusion was defined as 0 PSV and no visible flow.9) Clinically significant carotid stenosis was defined as a PSV greater than 125 cm/s.3)
Continuous variables were expressed as mean±SD. Categorical variables were expressed as frequencies and percentages. Statistical comparison between the groups was performed by 1-way analysis of variance. Chi-square test was used to compare categorical variables. 'Correlation analysis was performed by Spearman correlation test for variables with abnormal distribution.' Multivariate binary logistic regression analysis was used to identify the independent risk factors for significant carotid stenosis. Receiver-operating characteristic (ROC) curve for the prediction of significant carotid stenosis (≥50%) was constructed and the area under the curve (AUC) was calculated for the Gensini score. The CI value for the cut off Gensini score was calculated using the sensitivity and specificity estimates. A p value less than 0.05 was considered as statistically significant. All statistical analysis was performed by statistical software ver. 16.0 (SPSS Inc., Chicago, IL, USA).
The mean age of patients was 66.16±5.66 years. Sixty-four patients (28.4%) had normal carotid arteries without any evidence of atherosclerotic plaque. One hundred-two patients (45.3%) had nonsignificant carotid stenosis (<50%), whereas the number of patients with 50 to 69% and ≥70% carotid stenosis was 40 (17.8%) and 19 (8.4%), respectively. The number of patients classified as 1-VD, 2-VD, and 3-VD was 34 (15.1%), 69 (30.7%), and 122 (54.2), respectively. The mean value of Gensini score and SYNTAX score was 54.15±30.13 and 18.96±6.93, respectively. The demographic and clinical characteristics of the entire study population are summarized in Table 1.
The study population was divided into 3 groups as patients with normal carotid artery, nonsignificant carotid stenosis (<50%) and significant carotid stenosis (≥50%). These three groups were compared in terms of demographic, anatomic and hematological characteristics in Table 2. The mean value of the Gensini score and Syntax score was highest in patients allocated to significant carotid stenosis ( p<0.001 and p<0.001, respectively), (Fig. 1). In addition, there were statistically significant correlations between the severity of carotid stenosis and the SYNTAX score (r: 0.349, p<0.001) and the Gensini score (r: 0.477, p<0.001).
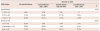
The predictors of coexisting significant carotid stenosis in patients undergoing CABG were found to be male gender (p=0.029), carotid bruit (p<0.001), diabetes (p=0.021), left main disease (p=0.002), 3-VD (p=0.008), chronic total coronary occlusion (p=0.001), coronary artery calcification (p=0.001), the Gensini score (p<0.001) and the SYNTAX score (p<0.001) in univariate analysis (Table 3). From these factors, multivariate analysis revealed the Gensini score (OR=1.030, p=0.004), carotid bruit (OR=0.068, p<0.001), and male gender (OR=0.190, p=0.003) as the independent predictors of significant carotid stenosis (Table 3). The prevalence of patients with various categories of carotid stenosis according to the tertiles of Gensini score and the number of stenosed coronary vessels was demonstrated in Table 4. There was a remarkable increase in the number of patients with significant carotid stenosis among the patients with increasing tertile of the Gensini score (Fig. 2). The Gensini score cut off value predicting significant carotid stenosis was 50.5 with 77% sensitivity and 63% specificity (AUC, 0.778; 95% CI, 0.712-0.843; p<0.001), (Fig. 3).
The main finding of this study is that the Gensini score is independently associated with the severity of carotid stenosis in patients undergoing CABG. There was a statistically significant correlation between the Gensini scores and severity of carotid stenosis. The incidence of significant carotid stenosis increases among patients with high Gensini score. Although the SYNTAX score and 3-VD terminology have showed a relationship with significant carotid stenosis, they were not independent predictors. These findings indicate that carotid artery screening may be recommended for patients having high Gensini score prior to CABG.
Carotid artery disease is an important risk factor for stroke in patients undergoing CABG.1) Atherosclerosis of carotid artery increases the risk of neurological complications via embolization from an ulcerated plaque regardless of the degree of carotid stenosis or by causing hypoperfusion distal to critical stenosis.10)11)12)13) However, routine carotid screening prior to CABG is controversial. Screening of carotid artery is essential in patients with a history of stroke or carotid bruit.14) In addition, routine carotid screening has a class IIa recommendation for patients with multivessel CAD, peripheric vascular disease, or >70 years of age.14) However, the predictors for coexisting significant carotid stenosis are not clearly established in patients undergoing CABG.
Carotid artery disease is related to the extent of CAD.2)3)4) Multivessel CAD has shown to be an independent predictor for carotid stenosis.3) However, the distribution of coronary atherosclerosis has been limited to the number of significantly stenotic coronary arteries in previous studies. 3-VD terminology is insufficient to represent the entire extent of coronary atherosclerosis. For instance, a significant lesion in mid or distal portion of any coronary artery is pooled together with a lesion in proximal portion despite the fact that the latter represents a higher atherosclerotic burden. Whereas, considering the number of coronary stenosis and degree of luminal narowing with a combination of geographic importance of the lesion position provides a more complete evaluation for the atherosclerotic burden.5)6)7) Therefore, an angiographic score such as the SYNTAX score or the Gensini score that can quantify the extent of CAD6) may be more correlated with the severity of carotid stenosis.
In our study, the Gensini score, the SYNTAX score, and 3 vessel CAD were found to be associated with carotid stenosis in patients undergoing CABG. The Gensini score and the SYNTAX score were well correlated with the severity of carotid stenosis. However, only the Gensini score showed an independent relationship with significant carotid stenosis. 33.6% of patients with 3-VD had significant carotid stenosis while 50% of patients with high Gensini score had significant carotid stenosis. The Gensini score higher than 50.5 had 77% sensitivity in prediction of significant carotid stenosis. These findings represent the role of Gensini score in prediction of significant carotid stenosis among the patients undergoing CABG.
In a recent study, the SYNTAX score has not been found to be associated with carotid atherosclerosis in patients with multivessel coronary disease.15) In contrast, we demonstrated an association between the SYNTAX score and significant carotid stenosis. However, this association was not an independent finding. This can be explained by the following reasons. First, the SYNTAX score defines a lesion as significant when it causes >50% luminal narrowing in vessels >1.5 mm diameter whereas the Gensini score defines stenosis starting at a level of 25% obstruction.5)6) Second, distinction has been made only between occlusive (100% diameter stenosis) and non occlusive (50-99% diameter stenosis) disease in the SYNTAX score.5) However, the Gensini score considers the diameter stenosis in an algorithmic methodology5) as 0-25%, 26-50%, 51-75%, 76-90%, 91-99% and total occlusion.16) Third, the SYNTAX score includes additional parameters in comparison to the Gensini score such as coronary artery dominance, thrombus, tortuosity, and, bifurcation or trifurcation type lesions.5)7) These individual components of SYNTAX score are not associated with atherosclerotic burden. They indicate increased difficulty for percutaneous coronary intervention and take a role in the selection of revascularization strategies.5)7) Therefore, the SYNTAX score is more related to the complexity of lesion rather than the extent of coronary atherosclerosis. In contrast, the Gensini score is well known angiographic tool for grading the severity and extension of coronary lesions.5)6)16) Because carotid stenosis is related to the extent of CAD,2)4) the SYNTAX score can not accurately predict significant carotid stenosis likewise the Gensini score.
Left main disease, chronic total occlusion and coronary artery calcification were the other pathological features of CAD associated with significant carotid stenosis. However, they were not independent predictors in the multivariate analysis. In addition, male gender, diabetes mellitus, and carotid bruit were found to be related to the significant carotid stenosis in univariate analysis. However, only male sex, and carotid bruit were independently associated with significant carotid stenosis. Variables such as hypertension, hyperlipidemia, and hemodialysis were not statistically different between the study groups. Although advanced age is a well established risk factor,3)4)11)13) we could not find an association between age and significant carotid stenosis. This may be due to the exclusion of patients aged <60.
CAS >50% is an established risk factor for post-operative neurological complication.11) The best management to decrease the risk of perioperative stroke related to carotid stenosis remains challenging. Regardless of the decision to revascularize carotid disease, providing the best medical theraphy has paramount importance in patients undergoing CABG, particulary over the long term.2) There is an uncertainty for selective screening to provide guidance for centers seeking to systematically optimize their carotid screening practices.17) We represent an objective assessment by using the Gensini score to predict coexisting significant carotid stenosis in patients undergoing CABG. Because many patients with 3-VD were referred for CABG, a further evaluation for carotid stenosis may be done in patients having a high Gensini score.
This study was based on a retrospective analysis in a single center. We only reviewed a group of consecutive patients who were scheduled for CABG. Our study population did not cover all patients who were scheduled for CABG because of the exclusion criteria. Therefore, our findings can not be generalized for patients who were younger than 60 years of age or with acute ST elevation myocardial infarction. In addition, because postoperative neurological complications, morbidity and mortality outcomes were outside the scope of this study, the predictive value of Gensini score on these parameters is not known. Prospectively designed studies are needed to clarify this subject.
Figures and Tables
Fig. 1
Comparison of the Gensini score and the SYNTAX score between the groups according to the severity of carotid artery stenosis.

Fig. 2
Distribution of the patients with various severity of CAS between the tertiles of Gensini score. CAS: carotid artery stenosis.

Fig. 3
Receiver operating characteristic curve of the Gensini score for predicting significant CAS in patients undergoing CABG. CAS: carotid artery stenosis, CABG: coronary artery bypass grafting, AUC: area under the curve.
Table 1
Baseline characteristics of the study population (n=225)

Table 2
Comparison of the patient characteristics according to the degree of carotid artery stenosis
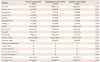
Table 3
Univariate and multivariate logistic regression analysis of variables predictive of significant carotid stenosis
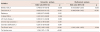
Table 4
Percentages of various severity of carotid artery disease according to the extent of coronary artery disease
References
1. Stamou SC, Hill PC, Dangas G, et al. Stroke after coronary artery bypass: incidence, predictors, and clinical outcome. Stroke. 2001; 32:1508–1513.
2. Venkatachalam S, Shishehbor MH. Management of carotid disease in patients undergoing coronary artery bypass surgery: is it time to change our approach? Curr Opin Cardiol. 2011; 26:480–487.
3. Steinvil A, Sadeh B, Arbel Y, et al. Prevalence and predictors of concomitant carotid and coronary artery atherosclerotic disease. J Am Coll Cardiol. 2011; 57:779–783.
4. Tanimoto S, Ikari Y, Tanabe K, et al. Prevalence of carotid artery stenosis in patients with coronary artery disease in Japanese population. Stroke. 2005; 36:2094–2098.
5. Sianos G, Morel MA, Kappetein AP, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005; 1:219–227.
6. Sinning C, Lillpopp L, Appelbaum S, et al. Angiographic score assessment improves cardiovascular risk prediction: the clinical value of SYNTAX and Gensini application. Clin Res Cardiol. 2013; 102:495–503.
7. Yadav M, Palmerini T, Caixeta A, et al. Prediction of coronary risk by SYNTAX and derived scores: synergy between percutaneous coronary intervention with taxus and cardiac surgery. J Am Coll Cardiol. 2013; 62:1219–1230.
8. Faggioli GL, Curl GR, Ricotta JJ. The role of carotid screening before coronary artery bypass. J Vasc Surg. 1990; 12:724–729.
9. Grant EG, Benson CB, Moneta GL, et al. Carotid artery stenosis: gray-scale and Doppler US diagnosis--Society of Radiologists in Ultrasound Consensus Conference. Radiology. 2003; 229:340–346.
10. Paciaroni M, Caso V, Acciarresi M, Baumgartner RW, Agnelli G. Management of asymptomatic carotid stenosis in patients undergoing general and vascular surgical procedures. J Neurol Neurosurg Psychiatry. 2005; 76:1332–1336.
11. Drohomirecka A, Kołtowski L, Kwinecki P, Wronecki K, Cichoń R. Risk factors for carotid artery disease in patients scheduled for coronary artery bypass grafting. Kardiol Pol. 2010; 68:789–794.
12. Kolh PH, Comte L, Tchana-Sato V, et al. Concurrent coronary and carotid artery surgery: factors influencing perioperative outcome and long-term results. Eur Heart J. 2006; 27:49–56.
13. Wanamaker KM, Moraca RJ, Nitzberg D, Magovern GJ Jr. Contemporary incidence and risk factors for carotid artery disease in patients referred for coronary artery bypass surgery. J Cardiothorac Surg. 2012; 7:78.
14. Authors/Task Force members. Windecker S, Kolh P, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014; 35:2541–2619.
15. Costanzo L, Campisano MB, Capodanno D, et al. The SYNTAX score does not predict presence of carotid disease in a multivessel coronary disease population. Catheter Cardiovasc Interv. 2014; 83:1169–1175.
16. Goyal BM, Sharma SM, Walia M. B-type natriuretic peptide levels predict extent and severity of coronary artery disease in non-ST elevation acute coronary syndrome and normal left ventricular function. Indian Heart J. 2014; 66:183–187.
17. Durand DJ, Perler BA, Roseborough GS, et al. Mandatory versus selective preoperative carotid screening: a retrospective analysis. Ann Thorac Surg. 2004; 78:159–166.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download